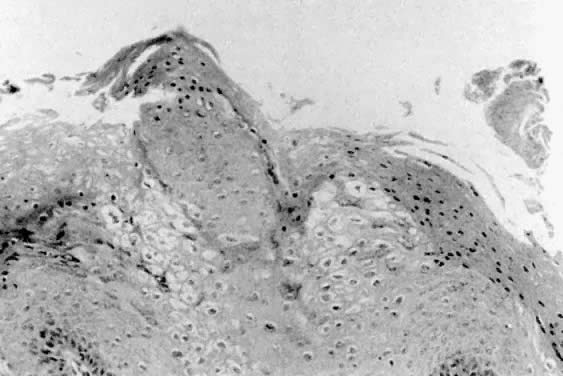
 Fig. 3. Condylomata showing acanthosis, parakeratosis
and koilocytotic changes. Volume 1, Chapter 9
Fig. 3. Condylomata showing acanthosis, parakeratosis
and koilocytotic changes. Volume 1, Chapter 9
|
Pathology Atlas: Vulva Michael John Hughey |
|
|
Michael John Hughey, MD |
| Condyloma |
|
|
| Vulvar Intraepithelial Neoplasia (VIN) |
|
|
| Paget Disease |
|
|
| Squamous Cell Carcinoma |
|
|
|
|
|
| Basal Cell Carcinoma |
|
| Melanoma |
|
| Leiomyosarcoma |
|
| Histiocytoma |
|
| Carcinoma in situ |
|
|
| Hidradenoma |
|
|
| Syringoma |
|
|
| Nevi |
|
|
|
|
|
|
| Fibroma |
|
|
| Neurofibroma |
|
|
| Granular cell tumor |
| Lymphangioma |
|
|