Interview
Most women are uncomfortable and somewhat apprehensive about consulting a gynecologist. These feelings are even more intense in teenagers who have heard various horror stories from their peers about such experiences-stories they are much more likely to believe than any realistic communication coming from an adult. Therefore, the most important part of the gynecologic interview may be the time spent by the physician to gain the patient's confidence. A survey of 84 adolescents reveals that most concerns about the pelvic examination were fear of the discovery of pathology, fear of pain, and embarrassment.1
One technique useful in beginning the adolescent interview is to explain pelvic anatomy. Most adolescents have a burning desire to learn the facts of life and facts about their bodies. A brief discussion directed to the adolescent will quickly put her parent (who usually is present during the interview) in the background. This will then lead to direct questioning of the adolescent herself, encouraging her to provide useful information. The conversation can thus be comfortably geared toward identifying the adolescent as the patient without alienating the mother. In general, adolescents relish the opportunity to assume adult roles and, in return, become cooperative and trusting.
In fact, propriety of parental presence in the interview is itself a point of debate. It is usually necessary to have a parent in the initial interview to complete the medical history for the patient; however, the presence of a parent may also inhibit the patient's free speech and prevent a trusting doctor-patient relationship from developing. Adolescents over 18 may be treated without parental consent; some states allow treatment of younger adolescents for venereal disease or drug abuse without parental consent.2
One compromise is to begin the interview with the parent present and then to dismiss him/her before the examination, thus giving the patient confidential time alone with her doctor. This is also a good time to inform the patient that you will tell her parent only that which she herself allows you to tell, and it is for this reason that her parent will not be invited into the examination room. Some patients will protest, but most will cooperate better without a parent in the room. Both the patient and her parent should be reassured that a gynecologic examination will not damage the patient's hymen, and the exam will not change her virginity. A diagrammatic explanation of the pelvic exam will help the patient understand exactly what is to be done.
History
The history itself should include all the essentials of a detailed medical history, as well as specific ages of adrenarche, thelarche, and menarche. This obvious point is all too often taken lightly by the gynecologist accustomed to dealing with adults referred to them by internists. (Adults usually have a complete examination only by the integration of the examinations of a few consultants: internists, gynecologists, ophthalmologists.) Adolescents often have not seen their pediatricians in years; thus, they require careful, thorough reviews of systems. Each positive symptom should be questioned as to frequency, relationship to menstrual cycle, and to ameliorating and provocative events. Inquiring how the patient is doing in school may be a tactful way to introduce questions about the patient's temperament, social history, and boyfriends.
Menstrual history of the patient's mother may help to explain a precocious or delayed menarche. Similarly, maternal drug ingestion during the patient's gestation may be relevant to the patient's complaint.
A menstrual history should be ascertained through specific questions regarding amount, length and frequency of flow. Questions such as, “Are your menses light or heavy?”, may not elicit correct information from a patient who has had only a few menstrual periods and is unaware of what is normal, light, or heavy. The number of pads or tampons used may also lead to an inaccurate assessment of menstrual pattern, Some females will change as soon as the pad is soiled, whereas others only when the pad is soaked. Questions are better focused on whether bleeding is so heavy that it cannot be contained in a pad or tampon, whether it requires both a pad and tampon, or whether the patient must awaken at night to change. All these findings indicate an abnormally heavy flow.
Dysmenorrhea usually does not occur until after the patient begins to ovulate. Because over 80% of the first years' menses are anovulatory,3 dysmenorrhea does not usually occur in early cycles.4 Severe pain with menses. requiring absence from school, must be investigated. During the history, the physician may also explain symptoms such as molimina and dysmenorrhea to reassure the patient that nothing is seriously wrong.
Particular attention should be given to the urologic history. Frequent urinary tract infections or previous urologic surgery may be related to a gynecologic problem. It may be difficult for some patients to distinguish between hematuria and intermenstrual spotting. It is usually difficult for all patients to distinguish between hematuria and menstrual blood in urine.
Adolescent patients have difficulty knowing what symptoms are important and require direct questioning in a specific manner, Open-ended questions, usually preferable in a medical history, are rarely beneficial in an adolescent history.
Examination
With the help of a nurse, the patient should be instructed to empty her bladder and then disrobe completely. A hospital gown will make the patient feel much more comfortable than a sheet alone. The patient's vital signs, including blood pressure with a properly sized cuff, should be taken. Her height and weight should be recorded along with arm span. The patient' s stature and posture should be noted. Congenital abnormalities, hair distribution, and skin lesions may suggest systemic disease. Similarly, an examination of the head and neck may reveal changes associated with systemic disease, such as lymphadenopathy, mucosal changes, or scleral icterus.
A heart and lung examination should be performed. Auscultation of the patients' abdomen prior to palpation will prevent falsely heightened bowel sounds. Abdominal contour and scars will uncover previous surgery, hernias, and masses. Palpation of the liver edge, spleen, and kidneys should be attempted; abdominal tenderness, rebound, or guarding should be noted. The presence of ascites should be ruled out. The Tanner stage of breast development must be recorded.
The breast examination must include an exam to elicit masses as well as nipple secretion. Usually, breast development is staged according to the Tanner classification, but this morphologic classification does not always reflect actual glandular development.5 In patients with precocious or delayed puberty, or with abnormal breast development, ultrasound examination of the breast is more reproducible and documentable. In addition, serial ultrasound examinations over time may prove a more reliable reflection of pubertal progression and therapeutic efficacy than Tanner staging alone.5
The pelvic examination of an adolescent should always be done on an examining table. The patient must be informed of what is to happen before each step. It is just as unwise to inform the patient, “This is not going to hurt,” as it is to inform her, “This is going to hurt.” It is much better to explain what is going to be done, perform the pelvic exam as gently as possible, and allow the patient to decide how painful it was or was not.
The external genitalia should also be staged according to the Tanner classification. The clitoris should be measured with a small ruler. The clitoris should not be larger than the average adult clitoris, 5.4 × 4.4 mm.6
The patient's hymen should be examined for patency as well as for caruncles. The secretions normally covering the hymen originate from the vestibular glands. An imperforate hymen will, of course, preclude the vaginal exam until hymenotomy is performed. At the superior aspect of the hymen lies the urethral meatus. which should be palpated to elicit tenderness and thickening, both signs of infection.
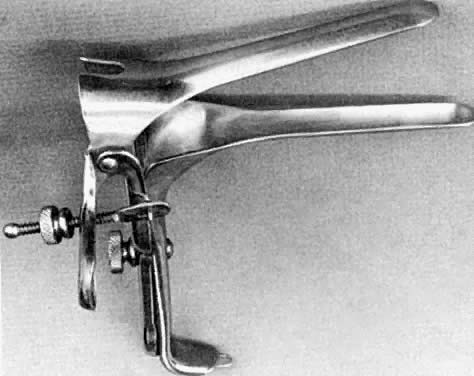
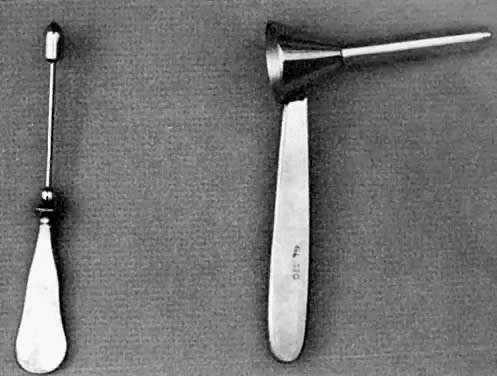
Visual examination of the vagina and cervix is best performed with a Huffman adolescent speculum (Fig. 1). This instrument has a 1.5-cm diameter and an 11-cm length. If the patient has been using tampons or having intercourse, the Huffman speculum will not be too big. However, if the introitus is too narrow to admit a speculum, a limited exam can be performed with a pediatric vaginoscope (Fig. 2). Unfortunately, visualization with this instrument is so poor that in most cases this exam yields little information and causes so much discomfort that the patient is less cooperative for the bimanual examination. The vaginoscope is useful, however, for removal of a foreign body. If the patient's complaint or symptoms mandate cervical visualization and the Huffman speculum is too large for her, it may be preferable to perform an examination under anesthesia than to perform inadequate vaginoscopy. In any case. the instrument used should be warm and lubricated. If a cytologic smear is to be taken, then lubrication with warm water is substituted for jelly. The instrument is inserted with the speculum blades closed and pointed posteriorly toward the coccyx. The patient may be asked to perform a valsalva maneuver while pressure is simultaneously exerted on the perineal body by the speculum. Posteriorly directed pressure avoids pressure on the anterior wall of the vagina and more sensitive urethra. Insertion is more comfortable if done slowly. The cervix should be examined for lesions, infection, or congenital anomalies. Directing the patient to flex her knees onto her abdomen will help position an eccentrically placed cervix.
|
|
One lubricated finger can usually be inserted in the vagina for a bimanual exam. If the introitus is too small, the digital exam must be rectal. After .entry, it is advisable to stop and allow the patient to regain composure and become accustomed to the finger in her vagina or rectum before proceeding with actual palpation. Palpation of the cervix will elicit tenderness produced by inflammation, ectopic gestation, and perhaps endometriosis. The uterine fundus can be palpated and its position, size, shape. and consistency noted. Normal tubes cannot be palpated. Normal ovaries can usually be palpated in thin patients. Any abnormal enlargement of the adnexae requires further investigation.
A rectovaginal exam with one finger in each orifice is too painful for the adolescent patient unless the introitus is well dilated. Thus, this exam should be avoided. A rectal exam alone will suffice.
Findings of the exam should be discussed with the patient immediately upon completion. Parenthetically, the adolescent should be informed that intercourse does not feel the same as a pelvic exam. The physician should stress that foreplay will increase vaginal compliance and lubrication to allow pleasurable lovemaking. This is, of course, a good time to inform the patient of her contraceptive choices. She should also be informed that when she decides to have intercourse, it should be pleasurable for her as well as her partner. A man mature enough for intercourse should be mature enough to understand the needs of his partner. It is a nice gesture to ask her permission to explain the findings to her mother and then repeat the discussion to both with the addition of therapeutic plans.
The adolescent gynecologic exam can be performed successfully only if enough time is allotted for the patient. One full hour is necessary for such exams. Physicians desiring to provide care for adolescents should be willing to amend their office schedule accordingly.
Prescribing for Minors
American law has traditionally considered an individual younger than twenty-one to be a minor, but most states have now lowered the age to eighteen.7 Of relevance is the concept of an emancipated minor, defined as an individual younger than eighteen who is married, has parental consent, is self-supporting, and is living apart from his or her parents, has parents who have failed their legal responsibilities, or has a judicial decree deeming him or her to be of the majority.7 Many states consider a pregnant female emancipated and therefore able to consent to abortion without the consent of her own parents. Many states consider the minor able to consent to medical care for herself if she is able to understand the risks and complications. This, of course, puts the physician in a difficult spot when dealing with a minor who has no parental consent. Indeed, the physician should consult with legal advisors as to what rights and responsibilities he or she has to the patient under the state law.