Diagnosis The concept that early diagnosis of twin pregnancy leads to a decreased
likelihood of perinatal mortality was described as early as 1979.17 Today, consensus exists that early diagnosis not only decreases mortality
and morbidity rates, but is the key to providing optimal antepartum
care and the cornerstone of effective management of labor and delivery. Among
the most important advantages of early diagnosis is elimination
of the possibility that the second twin will remain unrecognized until
after the birth of the first. When the senior author (LK) initially
reviewed data from the Department of Obstetrics and Gynecology at Northwestern
University and the 13 hospitals that then referred their newborns
for care from 1970 to 1975, he found that approximately 40% of
twin gestations were unknown or undetected either until the mother arrived
at the delivery room or until after the delivery of the first twin.18 This figure had declined to 10% by 1984, when Chervenak and co-workers19 published data on a series of 385 consecutive twin deliveries. Recent
data from Sweden showed that the majority (97%) of all pregnant women
received an ultrasound screen in the year 1990.20 Of these, 90% were performed from 16 to 18 weeks and 10% at 10 to 12 weeks. Thus
the likelihood of undiagnosed twins was remote in these circumstances. Population-based figures such as these can be extrapolated
to the United States or, for that matter, to any other country. Whether or not population-based ultrasound should be the standard of care
remains a matter of debate. European countries, most notably France
and England, consider it as such. In the United States, however, opinions
are divided based on whether even a single ultrasound is a cost-effective
means to reduce morbidity and mortality. One prospective randomized
study suggests that it is not,21 but this opinion is not accepted by all,22 especially when multiples are concerned. Opponents of routine ultrasound
suggest that numerous clinical criteria suggestive of multiple pregnancy
exist and that one or more should be present to trigger the decision
to order an ultrasound. These clinical indicia include: (1) fundal
height greater than expected for dates; (2) simultaneous auscultation
of two or more fetal heart tones (FHTs) (an attempt to find a second
FHT is rarely, if ever, made); (3) presence of hydramnios; (4) unexplained
excessive maternal weight gain; (5) unexpected severe anemia; (6) increased
fetal activity; (7) early onset of pregnancy-induced hypertension; (8) personal
or family history of twins; and (9) an abnormally
elevated alpha-fetoprotein or triple screen in the second trimester. It
is important to remember, however, that all of these clinical indicia
were well recognized in the era before the advent of ultrasound. Without
doubt, their lack of use has contributed to the underdiagnosis
of twins. The use of first-trimester ultrasound for diagnosis of twins is intuitively
attractive, but unfortunately not without certain limitations (see
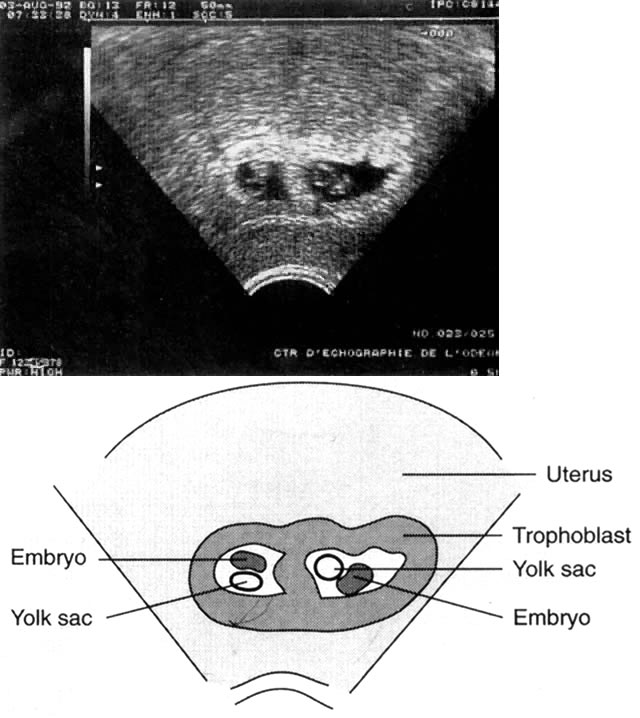
later discussion). In either the first or second trimester, the diagnosis
of a twin pregnancy is based on the simultaneous visualization, on
the same ultrasound section, of the corresponding body parts of two
fetuses.23 Some years ago this observation was mainly restricted to the simultaneous
visualization of two fetal heads as they often were the only easily
identifiable parts using the technology of the time. In contrast, current
technology permits easy identification of complete embryos (Fig. 5). Ideally both embryos should be visualized at the same initial exploratory
examination. However, once a twin gestation has been identified, the examination should continue
in order to avoid missing a higher order pregnancy.24 Although multiple sacs are clearly identifiable at 5 weeks of amenorrhea (3 weeks
postfertilization), embryonic visualization is usually possible
only at week 7 of amenorrhea (depending on operator experience and
technical capacity). 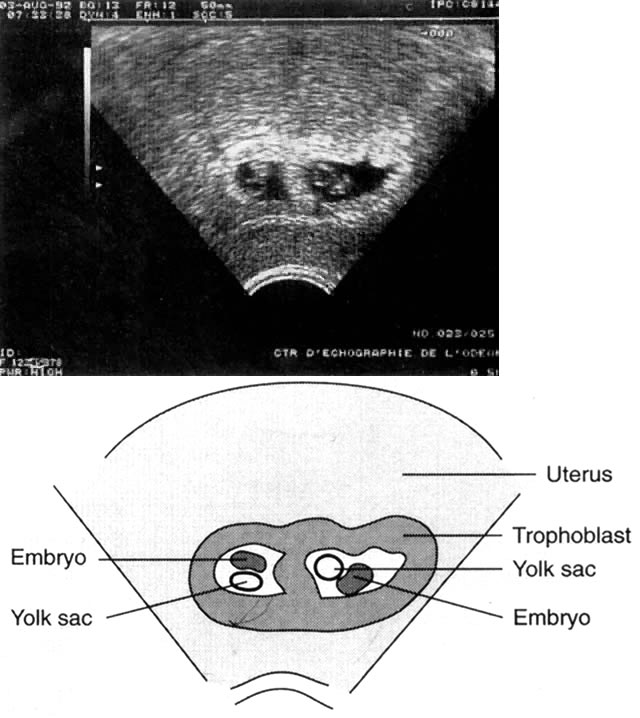 Fig. 5. Dichorionic twin pregnancy (6 weeks). (Bessis R: Ultrasound scanning techniques. In Keith LG, Papiernik E, Keith
DM, Luke B [eds]: Multiple Pregnancy: Epidemiology, Gestation
and Perinatal Outcome. London, Parthenon Publishing Group, 1995) Fig. 5. Dichorionic twin pregnancy (6 weeks). (Bessis R: Ultrasound scanning techniques. In Keith LG, Papiernik E, Keith
DM, Luke B [eds]: Multiple Pregnancy: Epidemiology, Gestation
and Perinatal Outcome. London, Parthenon Publishing Group, 1995)
|
In the opinion of most experts, the major advantage of first or very early second trimester diagnosis is
the confirmation or adjustment of the estimated date of conception as
well as the clear delineation of chorionicity. The confirmation of estimated date of conception is particularly valuable
because of the high rate of fetal growth abnormalities in twins as
well as higher order multiple pregnancies. It is important to distinguish
monochorionic from dichorionic placentas because of the far greater
rates of morbidity and mortality for monochorionic compared to dichorionic
twins (see earlier discussion). The question of zygosity is related, but
of much less importance. It should be recalled that monozygotic
twinning in pregnancies produced via artificially reproductive technology
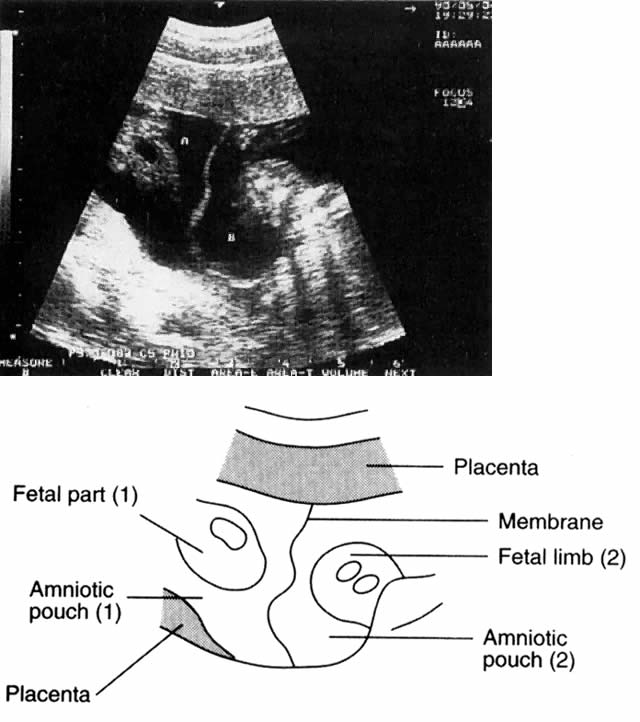
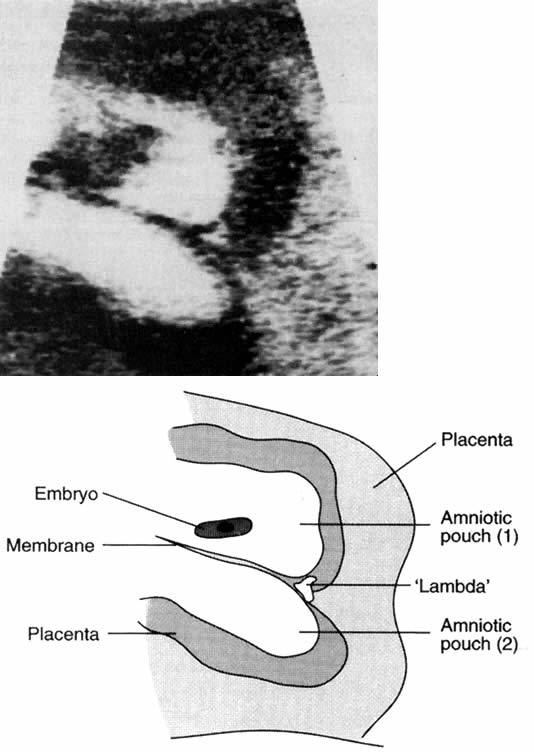
is almost triple the rate seen in spontaneous gestations.13,14 Many of these may be monochorionic. The presence of a webbed, lambda-shaped
structure at the end of the interovular membrane is pathognomonic
of dichorionic (or multichorionic) pregnancies (Fig. 6).25 This structure is particularly visible between 8 and 13 weeks of amenorrhea, and
its presence or absence should be mentioned in any clinical
report. The thickness of the intertwin membrane is also indicative of chorionicity. To some degree, the reliability of this measurement is as dependent on
the technical conditions of the examination as it is on the actual thickness
of the structure being examined (Fig. 7). The following is a useful clinical tool: 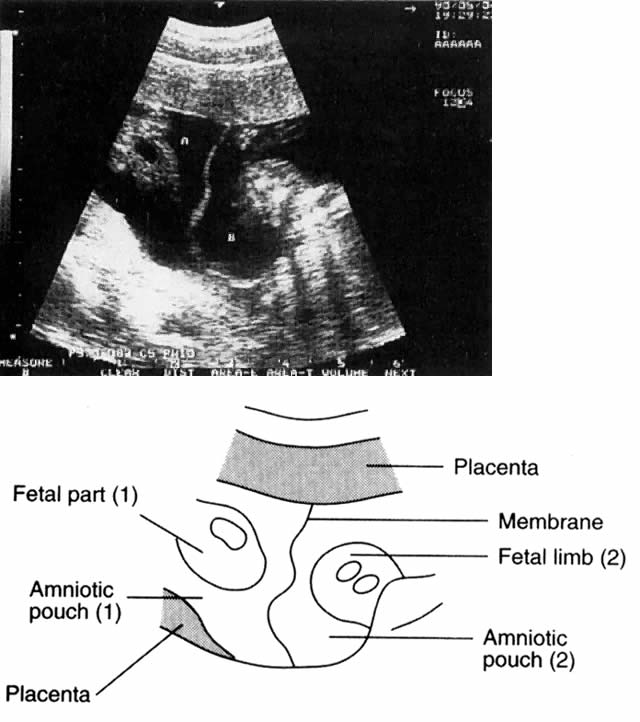 Fig. 6. Lambda-shaped membrane.(Bessis R: Ultrasound scanning techniques. In Keith LG, Papiernik E, Keith
DM, Luke B [eds]: Multiple Pregnancy: Epidemiology, Gestation
and Perinatal Outcome. London, Parthenon Publishing Group, 1995) Fig. 6. Lambda-shaped membrane.(Bessis R: Ultrasound scanning techniques. In Keith LG, Papiernik E, Keith
DM, Luke B [eds]: Multiple Pregnancy: Epidemiology, Gestation
and Perinatal Outcome. London, Parthenon Publishing Group, 1995)
|
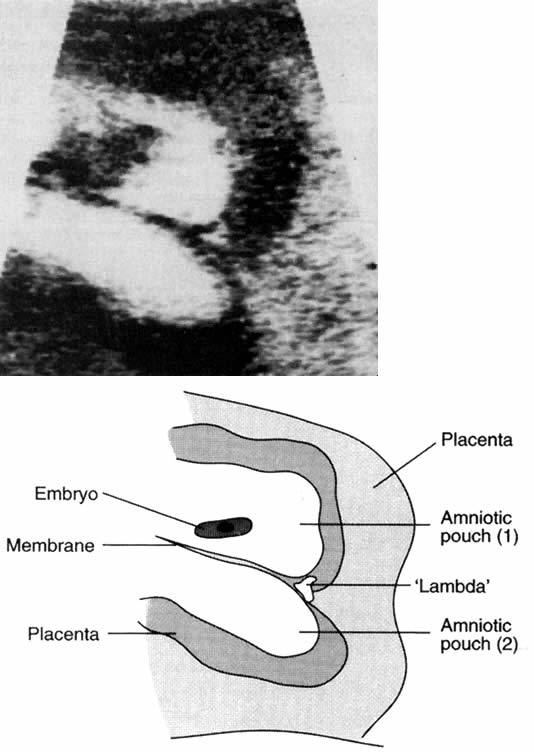 Fig. 7. Interovular membrane in a monochorionic pregnancy.(Bessis R: Ultrasound scanning techniques. In Keith LG, Papiernik E, Keith
DM, Luke B [eds]: Multiple Pregnancy: Epidemiology, Gestation
and Perinatal Outcome. London, Parthenon Publishing Group, 1995) Fig. 7. Interovular membrane in a monochorionic pregnancy.(Bessis R: Ultrasound scanning techniques. In Keith LG, Papiernik E, Keith
DM, Luke B [eds]: Multiple Pregnancy: Epidemiology, Gestation
and Perinatal Outcome. London, Parthenon Publishing Group, 1995)
|
In the presence of a single placenta, a membrane thickness of 2 mm or less
favors the likelihood of monochorionic-diamniotic placentation.
If, however, the membrane thickness is 4 mm or greater, fused dichorionic-diamniotic
placentation is indicated in the presence of a single placental
disc.26
In the second trimester, in addition to the detection of the twin condition, advantages
of ultrasound examination include reliable estimation
of gestational age; exclusion of placenta previa; detection of major
structural anomalies, such as spina bifida, acrania, or conjoined twinning; and
an opportunity for early bonding between a mother and her children. It
is important to remember that later ultrasound is more productive
for the detection of structural and/or body stalk abnormalities
and progress of growth than for the optimal detection of chorionicity. For
this reason, some experts believe that the improved outcomes that
accrue from early detection of any deviation from normal more than compensate
for the extra cost of multiple ultrasound examinations.22 An extensive review on the use of ultrasound in multiple gestation is
provided by Lopez-Zeno and colleagues27 as well as by Bessis.23 As suggested above, clinical methods of diagnosing twin pregnancy are underutilized. More
important, each method is fraught with inherent inaccuracies. For
example, examination of fundal height is not only dependent
on operator experience and skill, but may be reflective of the thickness
of the maternal abdominal wall or whether the uterus is in a state
of relaxation or contraction at the time of the examination. Because
auscultation of the FHT is considered successful once heart tones
are found, it is speculative how often this test is used to the point
of calling another person to listen for a second sound. Further, unless
the onset of hydramnios is acute and severe enough to cause symptoms, the
quantity of fluid may be insufficient to allow its detection without
the use of an ultrasound scan. Although excessive weight gain may
be the first clinical sign of a twin gestation, lack of a precise definition
of “excessive” may hinder its clinical utility. Recently
the National Academy of Sciences (NAS) recommended an ideal total
weight gain of 35 to 45 lb for twin pregnancy,28 but provided no definition of excessive weight gain. The NAS recommendation
is useful, however, because it can be the basis of early intervention
after initial diagnosis. Indeed, Luke29 and others15 have refined this recommendation to include the necessity of gaining 24 lb
by the 24th week. Before recommending a comprehensive plan of weight
gain, care givers should take into account the maternal prepregnancy
body mass index and stature as well as the fact that about one half
of twin pregnancies deliver at the 37th week of gestation or earlier. This
latter point mandates an early gain, as opposed to waiting until
after 32 weeks to try to augment weight. Unfortunately, anemia is clearly too ubiquitous a sign to relate solely
to multiple gestation. At the minimum, a complete blood count should
be obtained and a stool sample studied for the presence of blood and/or
parasites if and when severe anemia is present. Because maternal perception
of increased fetal activity is uniquely subjective, an ultrasound
examination may help determine whether a perception of “too
much movement” is indeed a result of twins. The use of a personal
or familial history of twins as a screen for obtaining an ultrasound
is paradoxical: many women with a strong family history of twinning do
not have twins, and many without it do. Of course, such clinical considerations
are superfluous in patients who have undergone any form of
artificial reproductive technology. In these instances, both the patient
and the clinician want to know about the existence of pregnancy and
its type as soon as possible. Without ultrasound, their wishes would
be frustrated. Although specific biochemical parameters, such as human chorionic gonadotropin
and human placenta lactogen levels, exhibit slow and predictable
increases as pregnancy progresses, these cannot be accurately applied
to twins.30 This statement may be modified by the recent observation of the use of
the three components of the pan - alpha-fetoprotein test.31 In the past, the use of any biochemical marker for the detection of twin
pregnancy was hampered by day-to-day fluctuations in individual patients; the
possibility of inaccurate conclusions based on miscalculations
of gestational age; and the need to confirm any abnormal test with
another of greater sensitivity. Because the finding of any abnormal biochemical
marker is almost invariably followed by an ultrasound examination, many
practitioners (at least at Northwestern) prefer to obtain
an ultrasound in the first trimester and biochemical assessments in the
second. In contrast, the policy at the University of Michigan is to
obtain an ultrasound routinely at 16 to 18 weeks (see earlier discussion). This
may preclude determination of chorionicity to some degree. Regardless, in
institutions where first-trimester ultrasound is underutilized, the
initial evidence suggesting the presence of twins may be
the alpha-fetoprotein test. Nutritional Considerations The importance of prenatal nutrition cannot be overstressed. Having said
this, until recently it was difficult for practitioners to develop practical
guidelines to share with their patients. Although a variety of
recommendations on the composition of the prenatal diet have been put
forward since antiquity, specific recommendations are of fairly recent
origin. Moreover, until 1990, recommendations were based purely on
the needs of a singleton pregnancy. The origins of dietary recommendations in pregnancy until at least the
late 1950s were based on the writings of the German obstetrician Prochownik, and
his predecessor Glassner, both of whom practiced in the latter
half of the 19th century.32,33 Their suggestions were based on the fact that weight restriction was beneficial
in producing smaller infants who were more likely to pass through
deformed, contracted, rachitic pelves. The Prochownik diet, as well
as other forms of weight restriction, which allegedly had no adverse
effect on small infants born at term, influenced medical thinking until
the middle of the 20th century.32,33 Writers inferred that the fetus and its mother were locked into a parasitic/symbiotic
relationship in which the maternal dietary intake or nutritional
status was immaterial. These opinions, though vehemently opposed
by more physiologically oriented authors, were the basis of the
widely accepted recommendation of a total weight gain of 20 lb. This dictum
remained unchanged until around the late 1970s, despite the fact
that several large hospital series published after 1940 suggested that
many patients did not adhere to the 20 lb recommendation and actually
gained more (20 to 30 lb) during their pregnancies.32,33 Among the deficiencies of these early hospital studies, however, was a
general lack of consideration of preconceptional weight or anthropometric
factors, such as short stature and low weight for height (body mass
index), along with gestational weight gain as they may have influenced
birth weight and length of gestation. After the association between
pregravid weight and birth weight was recognized, gestational weight
gain began to be viewed as a therapeutic intervention that not only augmented
deficiencies of pregravid weight in the mother, but led to increased
fetal growth and higher birth weights.32,33 Unfortunately, the “starvation mentality” initiated in the
late 1800s was apparent as late as 1980. Taffel34 analyzed the gestational weight gain component of the 1980 National Mortality
Survey and the National Fetal Mortality Survey. A total of 23% of
women giving birth in 1980 gained less than 21 lb, and 12% less than 16 lb. Black
mothers were more likely to gain less than 21 lb and were
twice as likely to gain less than 16 lb compared to white mothers. Fortunately, the 1990 NAS
publication, Nutrition During Pregnancy, served as a crucial turning point in developing rational guidelines for
weight gain in pregnancy.35 This report reviewed all available data on gestational weight gain. It
recommended, for the first time, ranges of gain by pregravid weight categories, including 28 to 40 lb for underweight women, 25 to 35 lb for
normal-weight women, and 15 to 25 lb for overweight women.28 It also recommended, for the first time, a 35- to 45-lb weight gain in
normal women with twin pregnancies. Two independent studies paralleled the NAS publication and provided an
indication of the future direction of subsequent clinical investigations. In
one, based on birth/death certificates from the Office of Vital
Statistics, Kansas Department of Health and Environment, from the years 1980 to 1996,36 a total of 922 twin gestations delivered at term were described. It was
determined that the proportion of infants born with LBW declined as
maternal prepregnancy weight status increased. It was further determined
that infant birth weights increased linearly with prenatal weight gain
for women who entered their pregnancy either underweight or at normal
weight, but not for those who were overweight or obese at the start
of their pregnancy. In another study, optimal pregnancy outcome (greater
than 37 weeks' gestation; both infants greater than 2500 g each, with
Apgar scores greater than 7) was associated with gestational weight
gains of 44 lb (20 kg) compared to 37 lb (16.8 kg) for women with less-than-optimal
outcomes.37 The concept of ideal or optimal twin pregnancy vis-à-vis maternal
weight gain was studied extensively by Luke and co-workers38 in a series of papers published between 1991 and 1995. These investigations
were based on all twin pregnancies of 28 or more weeks' gestation
delivered between January 1, 1979, and December 31, 1989, at the Johns
Hopkins Medical Institutions in Baltimore. Pregnancies complicated
by extreme maternal obesity or pathologic weight gain were excluded in
order to facilitate the evaluation of the maternal anthropometric characteristic
of pregravid weight and subsequent gestational weight gain. Of
the 274 available pregnancies, 111 were excluded because of one or
more exclusion factors, and 163 twin pairs remained for analysis. When
total weight gain was investigated in terms of early (before 24 weeks) and
late (after 24 weeks) gain, twins with higher birth weights and
shorter lengths of stay were delivered of mothers with higher late rates
of gain. Luke and colleagues39 suggested that an early rate of gain of 1 lb/week before the 24th week
and a late rate of gain of 1.5 lb per week might have therapeutic advantage. These
analyses support the recommendations of the National Academy
of Sciences. More important, however, they clarify the relationship
between early and late rate of weight gain, total weight gain, and
perinatal outcomes, including birth weight and length of stay (LOS), as
shown in Table 4. TABLE 4. Comparison of Perinatal Outcomes by Term vs Preterm and by Average
of Twin Birth Rates <2500g vs  2500g 2500g
Pregravid Weight | | Gain | Length of | Birth | Length | Birth |
for Height and Birth | | Rate of Gain (lb/wk) | Gestation | Weight | of Stay | Weight |
Weight Categories | n | Early | Late | Total (lb) | (weeks) | (g) | (days) | Ratio |
Preterm* | 90 | 0.93 | 1.13 | 33.2 | 33.6 | 2024 | 16.3 | 0.973 |
Term† | 73 | 0.9 | 1.31 | 40.5 | 38.4 | 2641 | 7.8 | 0.836 |
p value | | NS | 0.03 | 0.001 | <0.001 | <0.001 | <0.001 | <0.001 |
Preterm | | | | | | | | |
<2500 g | 78 | 0.92 | 1.1 | 32.2 | 33.3 | 1921 | 18.1 | 0.948 |
 2500 g 2500 g | 12 | 1.03 | 1.35 | 39.6 | 35.1 | 2693 | 4.5 | 1.135 |
p value | | NS | NS | NS | 0.01 | <0.001 | <0.001 | 0.01 |
Term | | | | | | | | |
<2500 g | 27 | 0.87 | 1.05 | 35.7 | 38.2 | 2184 | 10.6 | 0.704 |
 2500 g 2500 g | 46 | 0.92 | 1.47 | 43.3 | 38.5 | 2910 | 6.2 | 0.913 |
p value | | NS | <0.001 | 0.02 | NS | <0.001 | <0.001 | <0.001 |
 2500 g 2500 g
| | | | | | | | |
Preterm | 12 | 1.03 | 1.35 | 39.6 | 35.1 | 2693 | 4.5 | 1.135 |
Term | 46 | 0.92 | 1.47 | 43.3 | 38.5 | 2910 | 6.2 | 0.913 |
p value | | NS | NS | NS | <0.001 | 0.01 | 0.03 | <0.001 |
* Preterm is defined as <37 complete weeks of gestation.
† Term is defined as {ewc MVIMG, MVIMAGE,!greateq.bmp}37 completed
weeks of gestation.
NS not significant at the 0.05 level (two-tailed).
(Luke B: Maternal characteristics and prenatal nutrition. In Keith LG, Papiernik
E, Keith DM, Luke B [eds]: Multiple Pregnancy: Epidemiology, Gestation
and Perinatal Outcome, p 303. London, Parthenon Publishing
Group, 1995)A companion investigation was conducted by Luke and associates at the Twins
Day Festival in Twinburg, Ohio, in the years 1989, 1990, 1991, and 1993. A
total of 924 mothers of twins were interviewed, and data were
obtained on their 1848 twin children. Study variables were compared
by “ideal outcomes” (2500 to 2800 g birth weight and 35 to 38 weeks' gestational
age) versus “nonideal outcomes” (birth
weight above or below 2500 to 2800 g and/or gestational duration less
than 35 weeks). Ideal twin outcomes had significantly fewer birth
weights below the 10th percentile (11% vs 28%; p < 0.0001).40 Further, a significantly greater number of mothers with ideal outcomes
did not smoke during their pregnancies (95.5% vs 17.3%; p = 0.01); they gained significantly more weight than mothers with nonideal
outcomes (44.8 vs 41.1 lb [p = 0.005] and 1.23 lb/week vs 1.14 lb/week [p = 0.02]). Finally, it was determined that both body mass index and
weight gain were positive factors affecting outcome. There was a progressive
increase in the odds ratio of an ideal twin outcome with increasing
weight gain. Weight gains below 35 lb were significantly associated
with a nonideal outcome, whereas gains of 35 lb or more, or even
more than 45 lb, were associated with ideal outcomes.40 The study also compared actual weight gains with those gains that the
mothers had been advised by their respective care givers. Actual gains
averaged closer to 45 to 50 lb, an amount substantially higher than the
advised average of 30 lb. In this study, the NAS recommendation of
a 25- to 45-lb weight gain was not significantly associated with ideal
twin outcome (adjusted odds ratio, 1.22; 95% confidence interval, 0.85 to 1.77), whereas
weight gain greater than 45 lb was (adjusted odds
ratio, 1.67; 95% confidence interval, 1.17 to 2.39; p = 0.005).40 The weight gains of twins studied at the Johns Hopkins Institution are
graphed alongside the NAS recommendations for singletons. Triplet weight
gains are also shown (Fig. 8). This figure emphasizes the gain required by the 24th week of gestation
in order to achieve “optimal gain” in the shortened average
gestational time that is common in twins and triplets.  Fig. 8. Recommendations for gestational weight gain by plurality.(*, National Academy of Science) (Luke B, Johnson TRB, Petrie R: Clinical
Maternal-Fetal Nutrition, p 287. Boston, Little, Brown & Co, 1993) Fig. 8. Recommendations for gestational weight gain by plurality.(*, National Academy of Science) (Luke B, Johnson TRB, Petrie R: Clinical
Maternal-Fetal Nutrition, p 287. Boston, Little, Brown & Co, 1993)
|
The enormous potential impact of aggressive efforts at maximizing maternal
weight gain was described by Luke and colleagues41 in a theoretic model in which the birth weights of twins were shifted
upward by 500 g at the lower side of the gaussian distribution of all
twin birth weights, while the upper end of the distribution curve was
maintained in its regular position. The net effect was to narrow the curve
and the area under it. Luke and associates calculated that if such
a shift could be implemented on a national basis by improved nutrition
or prolongation of pregnancy it would reduce VLBW and perinatal mortality
by 59.5% and 84.6%, respectively. It would also result in a lifetime
cost saving of $219 million annually for each year's birth
cohort by reducing physical handicap among survivors. Increasing birth
weights and gestation length also have dramatic effects on LOS. In the
Johns Hopkins database, for infants born at less than 37 weeks of gestation, LOS
was 1.5 to 2.0 times greater for twins with intrauterine
growth retardation (IUGR) compared to non-IUGR twins, whereas no significant
differences were found between non-IUGR twins and singletons.42 At weights below 2500 g, IUGR twins had significantly higher LOS compared
to singletons.42 Specifically, for non-IUGR twins compared to singletons, LOS was nearly 50% and 30% shorter, respectively, for the birth weight categories of 1000 to 1499 g
and 1500 to 1999 g. In contrast to the growing consensus regarding total weight gain and rate
of gain considered optimal in twin pregnancies, little consensus exists
regarding dietary supplementation with iron, vitamins, minerals, and
folic acid, although the value of folic acid in terms of its ability
to prevent neural tube defects is now widely appreciated. The recommendations
contained in Nutrition During Pregnancy35 are as follows: - Beginning at the 12th week of gestation, routine use of 12 mg of ferrous
iron per day is recommended. Ferrous sulfate or fumarate are preferable
because the former contains 20% iron by weight (60 mg of elemental
iron in a 300 mg tablet). Ferrous fumarate contains 32% iron by weight (96 mg
elemental iron in a 300 mg tablet).43
- Supplemental medication should be free of additional ingredients, such
as calcium, magnesium, or zinc, all of which reduce the absorption of
iron.
- Supplemental iron should be taken between meals with liquids other than
milk, tea, or coffee.
- Hemoglobin level should be determined early to detect preexisting anemia. Levels
below 11 g/dL during the first and third trimesters or below 10.5 g/dL
during the second trimester are characteristic of anemia.
Table 5 shows the cutoff values for anemia in women—pregnant and nonpregnant, smokers
and nonsmokers—adapted from the Centers for Disease Control criteria
for anemia in childbearing-aged women.44 When accompanied by a serum ferritin concentration of less than 12 μg/dL, iron
deficiency anemia can be diagnosed with certainty. Required
treatment consists of 60 to 120 mg/day of ferrous iron until the hemoglobin
concentration becomes normal. At this time, the dose of iron can
be decreased to 30 mg/day. No specific prenatal dietary guidelines
have been published for expectant mothers of twins. In the absence of
such recommendations, Luke and co-workers suggested that a 50% to 100% increase
in the recommended dietary allowances for singleton pregnancies
be used for women with twins. Their adaptation of the 10th edition
of The Pregnancy RDAs in National Academy of Sciences is shown in Table 6.44 TABLE 5. Cutoff Values for Anemia in Women: Nonpregnant and Pregnant, Smokers
and Nonsmokers
| Hemoglobin (g/100 mL) | Hematocrit (%) |
| Smokers | Smokers |
| Nonsmokers | 10–20* | 21–40* | Nonsmokers | 10–20* | 21–40 |
Nonpregnant | 12.0 | 12.3 | 12.5 | 36.0 | 37.0 | 37.5 |
Pregnant | | | | | | |
1st Trimester | 11.0 | 11.3 | 11.5 | 33.0 | 34.0 | 34.5 |
2nd Trimester | 10.5 | 10.8 | 11.0 | 32.0 | 33.0 | 33.5 |
3rd Trimester | 11.0 | 11.3 | 11.5 | 33.0 | 34.0 | 34.5 |
* Number of cigarettes smoked per day.
(Luke B, Johnson TRB, Petrie R: Clinical Maternal-Fetal Nutrition, p 196. Boston, Little, Brown & Co, 1993)TABLE 6. Summary of RDAs* for Women Aged 25 and Older, Pregnant with Singletons
vs Twins
| Singleton | Twin/Triplet | |
Nutrient | Pregnant | Pregnant | Dietary Sources |
Folic Acid | 400 mg | 800 mg | Leafy vegetables, liver |
Vitamin D | 10 μg | 15 μg | Fortified dairy products |
Iron | 30 mg | 50 mg | Meats, eggs, grains |
Calcium | 1200 mg | 1800 mg | Dairy products |
Phosphorus | 1200 mg | 1800 mg | Meats |
Pyroxidine | 2.2 mg | 4.0 mg | Meats, liver, grains |
Thiamine | 1.5 mg | 3.0 mg | Enriched grains, pork |
Zinc | 15 mg | 30 mg | Meats, seafood, eggs |
Riboflavin | 1.6 mg | 3.0 mg | Meats, liver, grains |
Protein | 60 mg | 120 mg | Meats, fish, poultry, dairy |
Iodine | 175 mg | 300 mg | Iodized salt, seafood |
Vitamin C | 70 mg | 150 mg | Citrus fruits, tomatoes |
Energy | 2500 kcal | 3000 kcal | Protein, fat, carbohydrate |
Magnesium | 320 mg | 450 mg | Seafood, legumes, grains |
Niacin | 17 mg | 25 mg | Meats, nuts, legumes |
Vitamin B12 | 2.2 mg | 3.0 mg | Animal proteins |
Vitamin A | 800 μg | 1000 μg | Dark green, yellow, or orange fruits and vegetables, liver |
* Recommended dietary allowances.
(Luke B, Johnson TRB, petrie R: Clinical Maternal Fetal Nutrition, p 285. Boston, Little, Brown & Co, 1993)Schedule of Visits A key element of intensive prenatal care for multiples should be the scheduling
of more frequent visits: every 2 weeks until 20 weeks, and weekly
thereafter. An alternative scheduling schema has been presented by
others.15 The rationale behind this precept is the fact that the mother must receive
not only the routine care provided to any pregnant woman (e.g., testing for neural tube defects and abnormalities of carbohydrate metabolism, amniocentesis ), but also the additional tests mandated by the
presence of multiple gestation (e.g., repeat ultrasound to clarify the type of placentation or membrane status, or
for surveillance for signs of preterm labor) as well as crucial
educational counseling. Regardless of the socioeconomic status of the parents and whether the pregnancy
was planned or unplanned, natural or assisted, the reactions
of prospective parents of twins are not the same as in a singleton pregnancy. Surprise
and delight are often admixed with apprehension and fear. Physicians and staff should guard themselves from being swept along in
the parents' euphoria; instead, they should present a rational and balanced
account of the increased risks associated with twin pregnancy and
what can be done to prevent them. Parents often leap from diagnosis
to delivery planning in their enthusiasm. They must be informed, and physicians
need to continually remind themselves and their staffs that
good prenatal care for twins consists of a multitude of special considerations
designed to bring the pregnancy to an optimal outcome and that
despite such efforts adverse events may occur before delivery. In the vast majority of instances, the prospective parents worry
about their ability to cope with the physical, emotional, and financial
demands of a multiple pregnancy.45 In addition, parents often bombard physicians and their staffs with questions, many
of which are based on reading or conversations with other
parents of multiples. More frequent visits not only facilitate obtaining
requisite examinations in a timely fashion, but also help establish
the rapport that is so helpful in guiding these pregnancies to successful
outcomes. More frequent visits also benefit monochorionic twins who are clearly at
higher risk as TTTS may be appreciated from 18 weeks onward. Therefore, weekly visits and liberal use of ultrasound is indicated for
these patients. More frequent visits also allow the mother to avail herself of information
about self-help groups, which can provide invaluable assistance for
prospective parents. For twin gestations, the National Organization
of Mothers of Twins Clubs is unique because it has numerous chapters located
throughout the country. As the mother is adjusting to the many
changes that will occur in the near future, she can also obtain valuable
information on breast feeding from La Leche League. A list of useful
addresses and phone/FAX numbers of some of the most important organizations
is provided at the end of the reference section (see Appendix). Selective Fetal Reduction in Multiple Pregnancy Most twin pregnancies will not benefit from selective reduction. Even in
higher order gestations, its use is controversial. The timing of selective
reduction in multiple pregnancy varies. In some instances, it is
performed in the first trimester, usually but not invariably for the
purpose of reducing the number of fetuses. Second-trimester reductions
are usually, but also not invariably, performed because one or more
fetuses are found to to have abnormalities (structural, chromosomal, or
mendelian). Access to this technique is not universal. In the United
States, nine centers have reported outcome data to date, but it cannot
be stated with certainty how frequently this operation is performed
outside of these reporting centers or the results of these endeavors. It
is clear, however, that this technique is not without risks (e.g., loss of the entire pregnancy, occasional infection). A learning period
is required before the technique is mastered, and the decision to resort
to reduction is never easy for the patient, especially if she has
been infertile for a period of years and only became pregnant as a result
of prolonged and costly efforts. Two summary chapters on the operative
technique of selective reduction are available for further reference.46,47 Two specific outcome variables associated with fetal reduction merit special
attention: (1) maternal serum alpha-fetoprotein level after second-trimester
reduction; and (2) rate of preterm delivery subsequent to
reduction. With regard to the first point, according to Lynch and Berkowitz,48 maternal alpha-fetoprotein in the second trimester is always elevated
after a reduction procedure and is not necessarily indicative of fetal
defects. This elevation is probably caused by release of tissue or serum
from the dead fetus or fetuses. Amniocentesis is not indicated in
these cases; rather, ultrasonography should be used to search for the
presence of fetal defects. Lynch and Berkowitz further noted that although
some patients may have laboratory evidence of disseminated intravascular
coagulation after reduction procedures, such changes generally
resolve spontaneously.48 With regard to the second point, in another report from the same institution, Berkowitz
and associates49 described the outcomes of 200 cases. In this series, higher order pregnancies (three
to nine fetuses) were reduced to 189 sets of twins, 5 sets
of triplets and 6 singletons. A total of 19 (9.5%) patients lost their
remaining fetuses before the 24th week of gestation. The mean gestational
age at delivery was 35.7 weeks for the pregnancies that continued. However, gestational
age at delivery varied inversely with the initial
number of fetuses from 36.1 weeks for women who presented with
triplets to 33.8 weeks for women who had six or more fetuses. This trend
was statistically significant. Of the 19 complete pregnancy losses, 16 occurred
more than 4 weeks after the reduction procedure. |
 2500g
2500g
 = cervical scores;
= cervical scores;  = contraction frequency.
= contraction frequency. 0 on or Before 34 Weeks' Gestation
0 on or Before 34 Weeks' Gestation