In the past, it was believed that the adolescent was too biologically immature
to achieve and complete a successful, uncomplicated pregnancy. The
very young adolescent, defined as within 2 years of menarche, was
felt to be subfertile secondary to an immature hypothalamic-pituitary-gonadal
axis and the resultant anovulatory cycles. In the
United States, the average age of menarche is 12.8 for white and 12.2 for
black girls.35 Contrary to traditional beliefs, teenagers initiating intercourse before
age 15 years are twice as likely to conceive within the first 6 months
of sexual activity as older teens.36 Ten percent of teenagers younger than age 15 years become pregnant within
the first month of initiating sexual activity; 50% of pregnancies
occur within the first 6 months of sexual activity.36 This increased risk is believed to be secondary to the low rate of contraceptive
use during the first few months of sexual activity and lack
of education regarding the times of increased fertility during the menstrual
cycle. In general, older studies described the adolescent pregnancy as a high-risk
pregnancy with an increased risk for the development of pregnancy
induced hypertension, preterm labor and delivery, LBW infants, cephalo-pelvic
disproportion, operative vaginal delivery, cesarean
delivery, and increased perinatal morbidity or mortality. Recent
literature has begun to dispute these beliefs. By dividing adolescents
into two age groups (typically 10 to 14 years and 15 to 19 years) and
by parity, a disparity in pregnancy outcomes has been noted. According
to the National Vital Statistics Report in 2001, the rate
of LBW infants born to teenage mothers younger than 15 years of age was 13% compared
with an incidence of 9% for mothers aged 15 to 19 years.7 A racial disparity was also noted in the national statistics. The LBW
infant rate was much higher for black adolescent mothers (14% for
ages 15 to 19) than white adolescents (8.4% for
ages 15 to 19). Satin and associates reviewed 16,512 births to girls aged 11 to 15, 16 to 19, and 20 and
older.37 They found that first births to adolescent mothers ages 16 to 19 years
had no increase medical complications of pregnancy when compared with
primigravidas older than age 20. Specifically, there was no increase
in prematurity, hypertensive complications, or neonatal morbidity. In
fact, the cesarean rate for the 16 to 19 age group was lower than the
rate for the older than 20 age group (14% vs. 18%, respectively).37 However, significant differences in pregnancy complications and outcomes
were found in adolescents younger than 15 years old. There was an increased
risk of preterm delivery in teenage mothers younger than age 15. The
percent of LBW infants (less than 2500 g) was also found
to be significantly increased when compared with older adolescents
and women older than age 20: 14% versus 10% versus 9%, respectively.37 Fraser and colleagues reviewed the outcomes of first pregnancies occurring
in white middle-class mothers aged 13 to 24.38 Their findings confirmed the influence of socio-demographic factors
on reproductive outcome. Inadequate prenatal care was associated
with an increased preterm delivery rates. They also found an increased
risk for preterm and LBW babies in the youngest gravidas, even in those
with the most favorable socioeconomic background, suggesting that adequate
prenatal care and improvement in socioeconomic factors do not
totally eliminate the medical risks of adolescent pregnancy in the youngest
age group.38 Increased risk for adolescents, particularly young adolescents, has been
demonstrated in a recently published retrospective chart review of 25,000 deliveries, which
included 2930 young adolescents, 11,788 mature
adolescents, and 11,830 controls older than age 2030 (Fig. 9). This study not only documented that pregnant adolescents were more
likely to be black, diagnosed with a sexually transmitted disease, and
reside with people other than their parents than were older pregnant
women but also showed that risks for poor obstetric outcome differed
by age of the adolescent. The risk of preeclampsia, eclampsia, preterm
delivery, LBW, and very LBW was greater in the very young adolescent, while
the mature adolescent was only at increased risk of eclampsia. All
adolescents were less likely to have a cesarean section or an operative
vaginal delivery than were older women. Other studies have also
documented a lower cesarean section rate in adolescents.39 It is unclear why very young adolescents should have a lower cesarean
rate.  Fig. 9. Risk of adverse pregnancy outcomes by age of adolescent. (Eure C, Lindsay M, Graves W: Risk of adverse pregnancy outcomes in young adolescent parturients in
an inner-city hospital.
Am J Obstet Gynecol
186:918–920, 2002) Fig. 9. Risk of adverse pregnancy outcomes by age of adolescent. (Eure C, Lindsay M, Graves W: Risk of adverse pregnancy outcomes in young adolescent parturients in
an inner-city hospital.
Am J Obstet Gynecol
186:918–920, 2002)
|
Similar outcomes have been observed in earlier studies by Scholl and associates40 and Stevens-Simon.41 Scholl and associates reviewed pregnancy and fetal outcomes in adolescents
by age and parity. The preterm birth rate for the young primigravida (within 3 years
of menarche) was 21%, compared with 14.7% for
the older adolescent primigravida.40 A decrease in the preterm birth rate by 21% was found for every
year the pregnancy occurred beyond menarche.40 While the mature gravid patient will generally have an increase in birth
weight in subsequent pregnancies, the young adolescent multipara with
a previous history of a LBW infant has a 44% risk of delivering
another LBW infant, compared with a 9.6% risk in the older adolescent
multipara with a previous LBW infant.40 For the young multipara younger than age 15 years, the adverse outcome
with the greatest frequency was that of delivering a LBW infant, not
prematurity. Young multiparas had a two-fold increased risk of
LBW infants compared with the multiparas older than age 16 years: 12.29% versus 8.51%.40 Poor prepregnancy nutritional state appears to be the main associated
finding in the young multipara with a resultant LBW infant. Scholl and
associates also noted that for multiparas younger than age 15 with a
previous preterm delivery, the risk for another preterm delivery was 37%, compared
with 8% for the older multipara with the same
history. These data suggest that poor prepregnancy nutrition and continued
maternal growth may have a substantial impact on fetal growth
and length of gestation in the adolescent gravida under age.36 Other maternal characteristics that placed the pregnant adolescent patient
at risk for a preterm delivery were conception within 3 years of
menarche, a low body mass index, a past history of physical or sexual
abuse, a socially deviant father of the baby, and vaginal bleeding during
the first 8 weeks of gestation.41 From these studies, it appears that the adolescent patient can expect a
positive obstetrical outcome. No increase in adverse obstetrical or perinatal
outcome has been demonstrated in the adolescent patient older
than age 15 years. Some studies suggest that the young adolescent (younger
than 15 years or within 3 years of menarche) is at an
increased risk for LBW infants and preterm delivery. However, this may
be related to multiparity and poor prepregnancy nutrition, rather than
to age alone. Nutrition Nutrition is one of the most important factors affecting pregnancy outcome
for any woman; prepregnancy weight and poor weight gain during pregnancy
are the two main factors linked with LBW infants. Teenagers, in
general, have lower nutritional reserves than their adult counterparts, secondary
to their own bodies' continued increased metabolic demands
for growth and their poor diets. Adolescents most likely to become
pregnant are often those who have inadequate nutritional status and
lower socio-economic background. The physical growth spurt may start as early as 10 years of age, with an
average age of onset of 12.5 years of age. Menarche typically occurs
toward the end of the linear growth spurt. While growth slows after menarche, it
continues for several more years.42 The reproductive organs and other body tissues also continue to grow for
several years after menarche.43 Pregnant adolescents continue to grow; however, their growth rate may
be slower than nonpregnant adolescents at the same developmental age.42 Because measurements of linear bone growth are obscured because of increased
lordosis during pregnancy, knee height measurements have been used
in pregnant adolescents and have shown that approximately half of
adolescents continue to get taller during pregnancy.44 What impact this continued growth and its metabolic demands have on pregnancy
outcome is still controversial. Adolescents within 3 years of
menarche tend to have lower total weight gains during pregnancy than do
older women. Obesity has reached an all time high in the United States, and excessive
weight gain in adolescent pregnancy may lead to a greater risk of obesity
after pregnancy. One study showed that excessive weight gain in
adolescents and young adults who have normal prepregnancy body mass indices
is associated with neither maternal growth nor duration of gestation, but
rather with retention of postpartum weight and triceps skin-fold
measures. Age is felt to be a less important factor in gestational weight gain than
prepregnancy body mass index (body mass index = weight ÷ height
squared). The Institute of Medicine's recommendations
for gestational weight gain in adolescents were originally published
in 1990 and were reviewed in 1997. The comment was made that
although new studies are necessary, no change in recommendations was required.36 Recommendations for weight gain by BMI are shown in Table 4. It is recommended that an adolescent with a low body mass index gain
amounts at the upper end of the range. Early inadequate weight gain in
the adolescent pregnancy may increase the risk for poor pregnancy outcome. A
weight gain of less than 4.3 kg by 24 weeks has been associated
with a significant increase in LBW infants.45 Late pregnancy weight gains of less than .4 kg/wk were found to be
associated with an increased rate of preterm delivery.45,46 Table 4. Recommended Total Weight Gain Ranges for Pregnant Women* by Prepregnancy Body Mass Index†
|
Recommended Total Gain |
| Weight-for-Height Category |
kg |
lb |
| Low (BMI <19.8) |
12.5–18 |
28–40 |
| Normal (BMI of 19.8–26.0) |
11.5–16 |
25–35 |
| High‡(BMI>26.0–29.0) |
7–11.5 |
15–25 |
*Young adolescents and black women should strive for gains at the upper
end of the recommended range. Short women (<157 cm, or 62 in) should
strive for gains at the lower end of the range.
†BMI is calculated using metric units.
‡The recommended target weight gain for obese women >29.0) is
at least 6.0 kg (15 lb).
(Nutrition During Pregnancy. © 1990, National Academy Press.)
The nutritional requirements for pregnant teenagers are not fully understood. Typically, the
requirements for pregnant adults are added to the
nutritional requirements for nonpregnant adolescents to provide an estimate
for the pregnant adolescent's daily nutritional needs. Because
of the very young adolescent's continued growth demands, the
daily nutritional requirements are usually placed at the upper limit
of the range. The average energy cost for a full-term pregnancy
is estimated at 300 kcal/day in a woman gaining 27.8 pounds (12.5 kg) and
delivering a 7.8-pound (3.4-kg) infant. Very
young adolescents are encouraged to consume an additional 200 kcal/day
for a total of 500 kcal/day.47 Twenty-five percent of all pregnant teenagers have diets deficient
in calcium, protein, vitamins, and iron.46 The 2001 Youth Risk Behavior Survey indicated that 84% of high
school students drink fewer than three glasses of milk per day,2 which is the daily recommended intake of calcium for pregnant adolescents
is 1300 mg, corresponding to more than four 8-ounce glasses
of milk per day.44 Most prenatal vitamin preparations provide only 300 mg of calcium. Protein
should provide 15% of the total energy needs. The additional
amount of protein needed during pregnancy is based on the amount of
protein deposited in new tissues, plus the efficiency of conversion of
dietary protein to tissue protein. Protein needs follow the pattern
of fetal growth needs, increasing in the late gestation. Currently, it
is recommended that pregnant adolescents maintain a daily protein intake
of 60 g per day.46 This is usually met by increasing the amount of whole grains, milk, and
meat from prepregnancy diet. Adequate intake of vitamins and minerals is essential to a healthy pregnancy; folate
and iron are particularly important. Folate supplementation
both before and during pregnancy is known to decrease the risk of
neural tube defects, and the recommended daily supplement is .4 mg of
folate or a daily intake of .6 mg.44 Because more than 50% of pregnant women in developing countries
have iron-deficient anemia, adequate iron intake before and during
pregnancy is essential. Physiologic iron requirements are three-times
higher in pregnancy than they are in menstruating women, and
that need is most significant during the second and third trimester
when requirements reach between 4 to 6 mg per day.48 During late pregnancy, most women have exhausted their iron stores and
rely on absorption of iron from their diet or from supplements. Women
who conceive during or soon after adolescence are even more likely than
their adult counterparts to enter pregnancy with low or even absent
iron stores.48 Iron deficiency during pregnancy is known to be associated with premature
delivery, LBW and increased perinatal mortality. In addition, infants
born to iron-deficient mothers have a higher prevalence of
anemia in the first 6 months of life.48 Adolescents who become pregnant are often in lower socioeconomic groups, have
poor baseline nutrition, and are not very knowledgeable about nutrition. One
study compared pregnant women who were eligible for the
Special Supplemental Nutrition Program of WIC but who were not participating
in the program with those who were participating. Results showed
that the longer a woman participated in WIC, the heavier her baby was
likely to be at birth. In addition, those who entered prenatal care
and received WIC support before 12 weeks of gestation were 25% less
likely to deliver a small-for-gestation baby.44 Risk-Taking During Pregnancy Adolescents are still maturing, emotionally and cognitively, and their
immaturity often results in risk-taking behaviors that have serious
consequences, especially during pregnancy. For an adolescent, social
acceptance gained by smoking, for example, may be considered a benefit
that outweighs the risk of poor pregnancy outcome. This is related
in part to the fact that young adolescents are typically concrete in
their thinking and not developmentally able to appreciate the future
consequences of their current actions. Decisions about health and risky
behaviors are more strongly associated with an adolescent's perception
of the current benefits of certain choices (such as choosing
to drink, smoke, not using seatbelts) than influenced by knowledge
or understanding of the risks associated with those behaviors.49 Substance Use National data suggest that more than 17% of pregnant adolescents
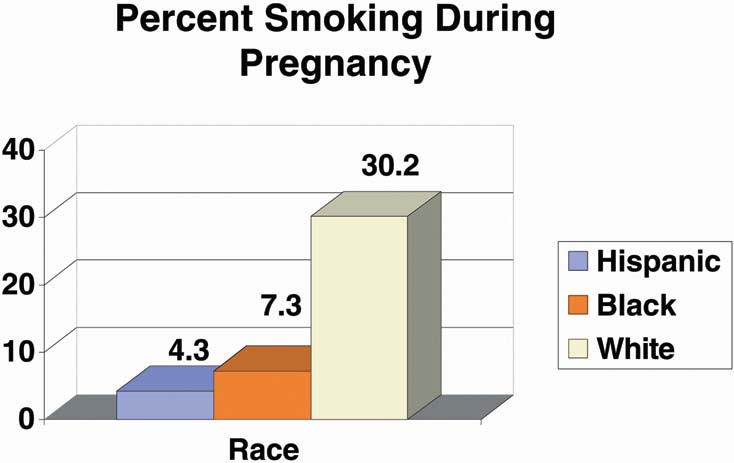
between the ages of 15 and 19 smoke cigarettes.49 Smoking varies by race, with more than 30% of nonHispanic white
girls reporting smoking during pregnancy50 (Fig. 10). Estimates of alcohol use by pregnant teens range between 17% and 54%, and
a significant number of pregnant adolescents
do not abstain from alcohol even after recognizing that they are pregnant, particularly
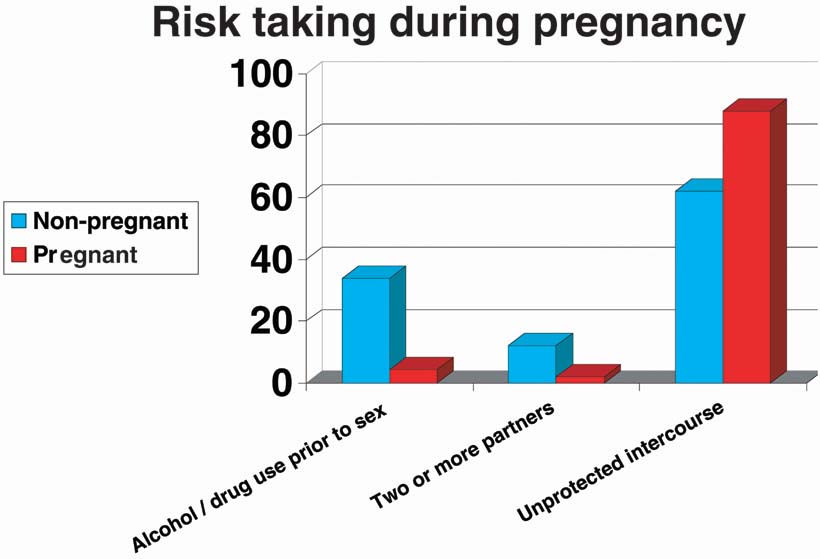
if their partners use alcohol.49 Interestingly, in a 2003 study by Niccoli and associates, only 4.5% of
pregnant adolescents reported using alcohol or drugs before sex, compared
with 34% of matched nonpregnant controls51 (Fig. 11). |
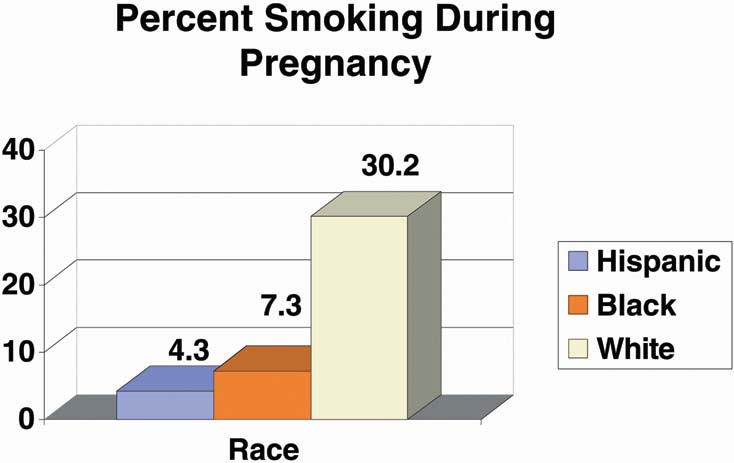 Fig. 10. Percent smoking during pregnancy.
Fig. 10. Percent smoking during pregnancy.
|
|
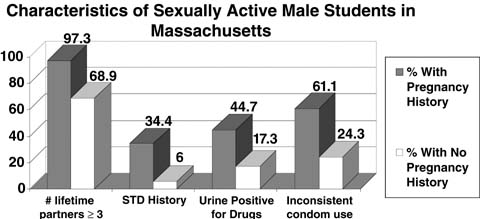
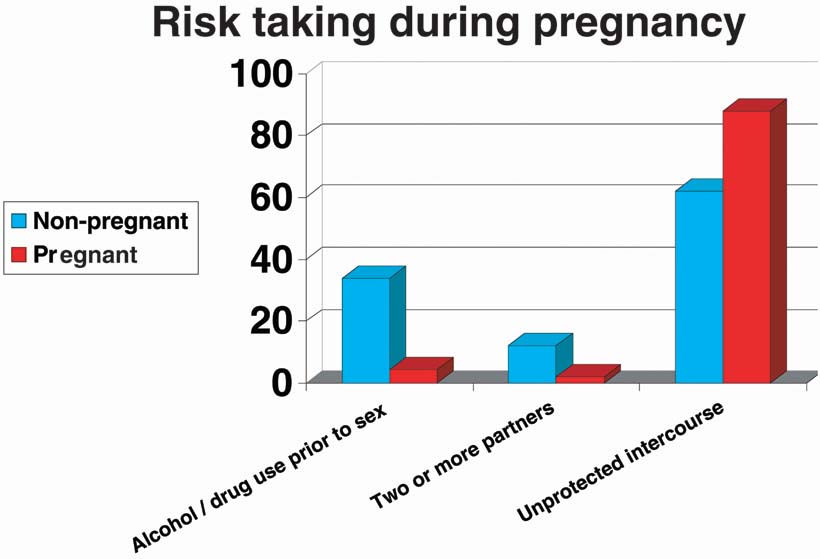 Fig. 11. Risk-taking during pregnancy. From Niccolai LM, Ethier KA, Kershaw TS et al: Pregnant Adolescents at Risk: Sexual behaviors and sexually transmitted
disease prevalence. Am J Obstet Gynecol
188:63–70, 2003)
Fig. 11. Risk-taking during pregnancy. From Niccolai LM, Ethier KA, Kershaw TS et al: Pregnant Adolescents at Risk: Sexual behaviors and sexually transmitted
disease prevalence. Am J Obstet Gynecol
188:63–70, 2003)
|
Sexually Transmitted Disease: Adolescents and Pregnant Adolescents Nearly four million adolescents are infected with sexually transmitted
diseases (STDs) each year, and 25% of the 12 million
new sexually transmitted infections occur in the adolescent population.50 A variety of diseases exist today that can be transmitted sexually. Chlamydia trachomatis, Neisseria gonorrhea, genital herpes, hepatitis B, syphilis, HIV, the human papilloma virus (HPV), and
trichomoniasis are the most common. Our knowledge
of the rates of Chlamydia infection has been enhanced by three main factors: (1) Chlamydia is now a reportable infection in all 50 of the United States; (2) Chlamydia can be found with voided urine or cervical specimens; and (3) the
DNA amplification tests have higher sensitivity than older tests. In 2001, the
CDC reported that females aged 15 to 19 had the highest
rates of chlamydia infection compared with all other groups, with an infection rate of 2536.1 per 100,000 girls
in the population. It is estimated that one of
every 10 sexually active girls has chlamydia.50 The prevalence of HPV infection in sexually active adolescents varies
depending on the population studied but appears to be 30% to 50%.52,53,54 In 2001, 1155 new cases of HIV were reported among adolescents aged 13 to 19, with
three-times that number reported among women aged 20 to 24. Because
the average time between infection with HIV and the
onset of AIDS symptoms is 10 years, most of the new cases of AIDS in the 20 to 29 age
group were contracted during the teen years. More than 50% of
adolescents with new diagnoses of HIV contracted it through
heterosexual contact.55 This, combined with the knowledge that 10% to 25% of teenage
girls have had more than four sex partners, makes it imperative that
clinicians who see adolescents be comfortable and knowledgeable about
sexually transmitted diseases to diagnose, treat, and counsel the
adolescent patient regarding high-risk sexual behaviors. Sexually transmitted infections are even more common among pregnant adolescents
than nonpregnant sexually active girls, with one recent study
from an inner-city clinic reporting that 19% had chlamydia and 3.5% had gonorrhea during pregnancy.51 Pregnancy represents a risk marker for unprotected sexual activity. Chlamydia and gonorrhea rates vary dramatically by region, and it is essential to
screen adolescents during pregnancy, both at initiation of care and
later in gestation to evaluate for re-infection. Adolescents are
much less likely to use condoms once they know they are pregnant, with 87% of
pregnant adolescents reporting unprotected intercourse
within the last 30 days, compared with 62% of matched nonpregnant
controls.51 Although rates of HIV infection are relatively low among adolescents, those
who become pregnant may be at higher risk than other teens. Pregnancy
is an excellent time to screen adolescents for HIV and provide education
about HIV transmission. In addition, babies who were infected
at birth are now reaching reproductive age. HIV screening is recommended
by the American College of Obstetrics and Gynecology (ACOG) for
all pregnant women at initiation of care. Prenatal care for adolescents is also an excellent opportunity to provide
preventative care and guidance. Pregnant adolescents are at high risk
for other STDs, and therefore should also be screened for chlamydia, gonorrhea, HIV, and syphilis during pregnancy and should be encouraged
to have the hepatitis B vaccine if nonimmune. Although a Pap test has
been a routine part of prenatal care, current guidelines for screening
recommend that screening be initiated approximately 3 years after first
vaginal intercourse; thus, cervical cytology screening may not be
indicated for some adolescents who are currently being screened routinely.56 Because we know adolescents are less likely to use condoms while pregnant, condom
use for STD prevention should be encouraged. Violence Before, During, and after Pregnancy Many pregnant girls have been victims of physical or sexual abuse before
pregnancy, and this strong association has been well-documented
in the literature. The rate of abuse reported by adolescents has ranged
from 26% to 31.6%.57 Adolescent girls may be especially vulnerable to abuse because of lower
self-esteem and greater adherence to dependent female gender
roles. A significant number of pregnant girls are abused by their male
partners; others are victims of continuing physical abuse from parents
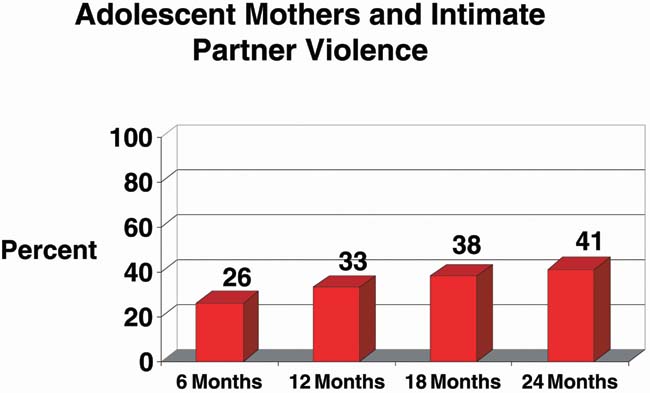
or guardians. Twelve percent of adolescents of diverse ethnic background
reported intimate partner violence during pregnancy, and even higher
rates postpartum, according to a 2002 study58 (Fig. 12). In one study reporting prospective abuse screening, 28% percent
of teens versus 23% of adult gravidas reported abuse before
the pregnancy.57 Fifty percent of the patients reporting a history of abuse during the
year before pregnancy would go on to experience further abuse during pregnancy, making
a previous history of abuse the number one risk factor
for abuse during pregnancy. The rate of abuse during pregnancy was 20.6% for
teens and 14.2% for adults. While the rate of abuse
was higher for teens, the intensity of abuse was greater in the adult
gravidas. The association between abuse and late onset of prenatal
care was demonstrated in this study. Of abused teens, 21.9% entered
prenatal care in the third trimester compared with 7.5% of
nonabused teens. While abuse during pregnancy was found to be a significant
risk factor for delivering a LBW infant, it was a more significant
associated risk factor for the adult women than for the teens. Abused
teens were found to have a significantly greater risk for poor weight
gain, first or second trimester bleeding, smoking, alcohol, and
illicit drug use.57 |
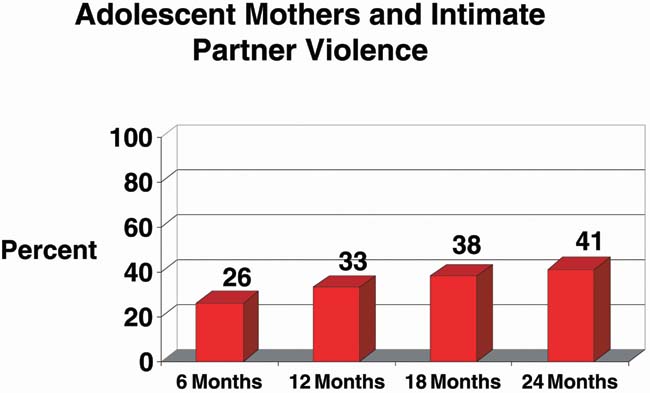 Fig. 12. Intimate partner violence. (Harrykissoon S, Rickert V, Wiemann C: Prevalence and patterns of intimate partner violence among adolescent
mothers during the postpartum period. Arch Pediatr Adolesc Med
156:325–330, 2002)
Fig. 12. Intimate partner violence. (Harrykissoon S, Rickert V, Wiemann C: Prevalence and patterns of intimate partner violence among adolescent
mothers during the postpartum period. Arch Pediatr Adolesc Med
156:325–330, 2002)
|
Pregnancy provides one of the few times adolescents may be motivated to
seek health care. Clinicians thus have a unique opportunity to offer
intervention and assistance to the abused adolescent patient, perhaps
breaking the cycle of abuse and preventing the escalating intensity of
abuse that occurs for one out of five adolescents as they become adults.57 |