Authors
INTRODUCTION
The cervical mucus examination of infertile women is an essential step in the infertility evaluation, considering that a cervical factor has been implicated in 5–10% of all cases of infertility.1, 2 In facilitating conception, the uterine cervix and its secretions have the following important actions:3
- Protection of sperm from the hostile environment of the vagina;
- Protection of sperm from phagocytosis;
- Supplementation of energy requirements of spermatozoa;
- Facilitation of sperm transport in the periovulatory period and interference at other times;
- Filtration of morphologically abnormal sperm;
- Preservation of large numbers of sperm within the cervical crypts and release of sperm into the upper genital tract.
PROPERTIES OF CERVICAL MUCUS
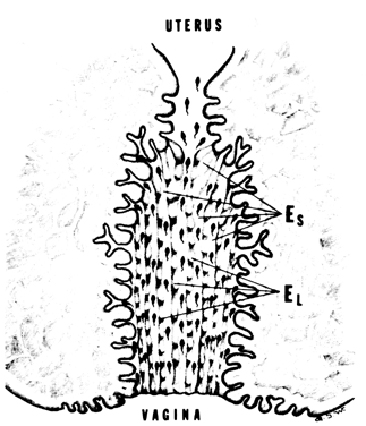
The conceptive functions and the receptivity of cervical mucus are determined by mucus composition. Cervical mucus is composed of several different types of mucus. The three most important, as described by Odeblad,4 are types E-S, E-L, and G. Types E-S and E-L constitute the ovulatory mucus; type G reflects the stimulation of gestagenic hormones on cervical mucus.3, 4, 5, 6
The ovulatory mucus is a mosaic composed of mucus “strings” and “loaves.” The strings (E-S) are fluid gels, and the loaves are more viscid gels (E-L). The result of estrogenic ovulatory stimulation on the mucin components is the production of abundant, watery, thin mucus that is nearly free of cell elements and possesses a high spinnbarkheit and pronounced ferning capacity. The sperm penetrability is highest at this time (Fig. 1). The sperm is found in the fluid (E-S) portion of the mucus, the composition of which allows rapid sperm transport to occur.
Fig. 1. Midcycle cervical mucus, after Odeblad's model, during early sperm transport.
CLINICAL APPROACH AND EVALUATION
Although the value of the clinical postcoital test (PCT) is the subject of considerable debate (see below), because the cervical factor plays an important role in infertility evaluations, the PCT of midcycle cervical mucus is widely used. The reasons for this are as follows:
- It is a qualitative measure of estrogen stimulation.
- It is only by examining the cervical mucus for spermatozoa that any direct information about the adequacy of insemination can be obtained.
- It provides information as to how sperm are interacting with the cervical secretions.
This microscopic examination of postcoital mucus has been practiced for more than 100 years. It was originally described by Sims, was modified by Huhner, and still is commonly called the Sims–Huhner test. The PCT has long suffered from inadequate standardization because of differences in variables such as the number of days of abstinence before testing, the time intervals between coitus and the PCT, the methods of collection, and the criteria of normality.
Abstinence before testing
The period of abstinence required to obtain the optimal PCT result is debatable, as it is for semen analysis. Some recommend up to 5 days, but most investigators recommend 2 days.1, 2
Time interval between coitus and the postcoital test
There have been various recommended time intervals from coitus to the microscopic examination of the cervical mucus. The shortest recorded time interval is 90 s,7 and the longest is 7–8 days.8 Clinically, it has been shown that there is a marked decrease in the number of sperm after 24 h, being negligible after 48 h.9, 10, 11 The decrease becomes clinically apparent after an 8-h interval. These findings have been substantiated by in vivo sperm transport studies.12 With the use of the fractional collection method (see below), the optimal time for collection was 2.5 h after coitus.13
The practical point from this discussion is that any PCT that is normal (i.e. revealing a large number of motile sperm) can be obtained at 2, 6, 8, or even 12 h after coitus, allowing some flexibility for the clinician. If, however, the results are abnormal, the test should be repeated at the optimal time of 2–3 h after coitus.
Method of collection
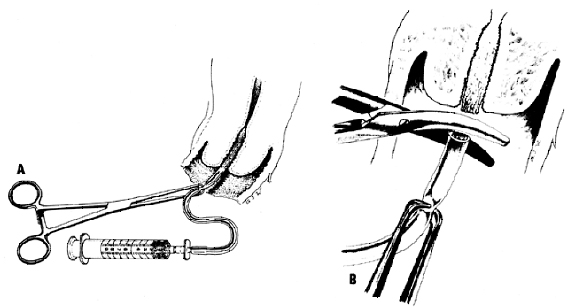
Difficulties in PCT interpretation have resulted from the different methods of collection used, such as a swab, polyp forceps, and catheters. Davajan and colleagues2 attempted to standardize the PCT interpretation by means of a fractional collection method, and I have found it to be very useful. The midcycle cervical mucus is aspirated into a polyethylene suction catheter attached to a large syringe. With a vaginal speculum in place, a wet mount of the vaginal pool is collected and the portio vaginalis cervicis is carefully cleansed with a cotton swab. Then a polyethylene catheter (3 mm in diameter, standard intravenous connecting tubing) is inserted into the endocervical canal. Without allowing contamination by the vaginal contents, the examiner stabilizes the tubing by grasping it 3 cm from the distal end with an atraumatic cervical clamp (large Allis or ring forceps) (Fig. 2). The grip should be adjusted so that the clamp is set at the first ratchet. In that manner the tube is partially, but not totally, occluded. The tube is advanced to the level of the internal cervical os, while gentle suction is applied to the tubing with a 10-mL syringe. The aspiration is stopped, and the grip of the clamp is closed completely. The tubing is gently removed from the endocervical canal, and any remaining mucus at the tip of the tubing is cut with scissors. The spinnbarkheit of the mucus is measured, and the mucus is placed under a coverslip on a slide (Fig. 3). The number of sperm and the percentage motility are determined by counting five separate fields under high power (×400). The results are recorded on the PCT data sheet (Fig. 4).
|
| Figure 3. The spinnbarkeit is measured and the mucus is placed on a slide. A. Longitudinal preparation. B. Cross-sectional preparation. |
| Figure 4. Postcoital test data sheet. |
It should be mentioned at this point that the PCT as originally described was a fractional PCT. The polyethylene catheter was divided into three sections corresponding to the internal, mid-, and external cervical canal. The internal os count was considered the meaningful determination. It has been shown that this method of testing postcoital cervical mucus is a true reflection of sperm transport in cervical mucus.14 Despite the validity of this method of collection, the necessity of fractionalization is debatable. Drake and associates15 collected 25 specimens in the fractional manner. To check the validity of this method, they interpreted the segments in a blind, random manner. There was a homogeneous distribution of motile and nonmotile sperm throughout the cervical mucus column and therefore no significant difference among the three segments; the use of any portion of the endocervical mucus column would be equally sufficient for PCT interpretation.
Interpretation
Although there is some disagreement concerning the method of PCT collection, there is even more disagreement concerning its interpretation. For some investigators, the mere presence of sperm in the cervical mucus is a normal test; others require 5, 15, or 20 sperm per high-power field. In an attempt to answer the question as to what constitutes a normal PCT, I applied the sperm transport method to the human female reproductive tract.12 Using the fractional collection method (see Fig. 2), I found the median number of sperm counted to be greater than 15 motile sperm per high-power field;14 however, compared with the number of sperm inseminated, the limitations of the PCT are apparent (Table 1). If the PCT is to be used as a measure of semen quantity, then only when there are greater than 15 motile sperm per high-power field can one be assured that the sperm count is at least 20 × 106/mL with 60% motility. A smaller count requires repeated semen analysis.
Table 1. Correlative values of serum and cervical mucus sperm
Sperm inseminated (×106 sperm/mL) | Cervical mucus sperm (motile sperm/hpf) | |
Median | 28.4 | >15 |
−1 SD | 8.8 | 11–12 |
−2 SD | 2.64 | 5.6 |
(Modified from Tredway DR, Buchanan GS, Drake TS. Comparison of the fractional postcoital test and semen analysis. Am J Obstet Gynecol 1978;130:647.)
It is important to note that a microscopic evaluation of cervical mucus after coitus will reveal a dumping of sperm. This results from the composition of ovulatory cervical mucus (discussed above). Because it is a mosaic of strings containing a fluid gel and loaves containing a more viscid gel, the sperm will lie in the fluid portion of the mucus. Whether sperm appears to be dumped on microscopic evaluation will depend on how the slide is prepared: longitudinally or cross-sectionally with the cervical mucus (see Figs. 3, 5). This emphasizes the importance of viewing multiple microscopic fields. The interpretative values of the PCT are listed in Table 2.
Table 2. Postcoital test
Criteria | Finding |
Days of abstinence | 2 |
Days of examination | Preovulatory (24 h after urinary LH surge, or 1–2 days before basal body temperature rise) |
Hours from coitus to exam | |
Optimal | 2–3 |
Acceptable, if normal | 3–8 |
Possible (often needs to be repeated) | 8–24 |
Number of motile sperm/hfp (400×) | |
Normal (one semen analysis) | 15 or more |
Can be normal (need repeated PCT and semen analysis) | |
Abnormal | <5 |
Cervical mucus | Clear, acellular |
Spinnbarkeit | 6 cm |
LH, luteinizing hormone
CLINICAL INTERPRETATION AND TREATMENT
With the basis and method of evaluation for the PCT established as described in the previous sections, it is important to distinguish the different factors that can be assessed during the clinical evaluation. The first problem to be solved is to distinguish among nonovulatory cervical mucus, altered sperm deposition, altered sperm penetration (sperm defect), and altered sperm transport (mucus defect).
Nonovulatory cervical mucus
One of the most prevalent etiologic factors for poor cervical mucus is improper time of collection due to nonovulatory cycles or to incorrect time of the cycle. Ovulation must be documented before the cervical mucus is sampled, and correct interpretations can be based only on preovulatory cervical mucus.2 It should be remembered that cervical mucus deficiencies with consequent impedance of sperm penetration are quite frequently the result of nonovulation and insufficient estrogen stimulation. Ovulation can be easily documented by measuring urinary luteinizing hormone (LH) levels collected every morning, and in some situations, in the late afternoon as well. This is determined by a monoclonal antibody technique.16, 17 In addition, the use of ultrasound monitoring to document ovulation has increased the prognostic value of the PCT.18 Once ovulation is secured, then the other factors can be determined from the PCT.
Altered sperm deposition
When the cervical mucus is normal, the PCT can determine difficulties with sperm deposition. Premature ejaculation, hypospadias, oligospermia, azoospermia, decreased semen volume, and impotence are conditions that can be identified. In conditions such as these, there will also be a decreased or absent number of sperm in the vaginal pool. The various etiologic factors must be considered, and once appropriate counseling is accomplished, artificial insemination can be a viable method of conception in many cases.
Homologous insemination (or artificial insemination, husband [AIH]) can be done by intracervical or cup (Milex Products, Chicago, IL) insemination.1, 2 The volume of the semen usually determines the method. If there is only 1 mL or less, intracervical insemination is usually done; a cup is used for larger quantities. It is important that the PCT be repeated after the insemination. Adequate sperm exposure to the cervical mucus should result in a normal PCT after the insemination. From the cervical mucus–sperm transport studies. it has been noted that by 15 min the total number of sperm in cervical mucus remains fairly constant for 24 h; however, a decline in the number of sperm starts 2.5 h after insemination.12, 13 The cervical cup is left in place for 20–30 min and then removed; the portio vaginalis cervicis is cleansed, and the PCT is performed. Conditions applicable to this form of therapy result in a success rate of 30–50%.2, 16 If the PCT is abnormal after the cervical insemination, intrauterine insemination (IUI) can be performed with washed motile sperm.19, 20
Altered sperm penetration
Poor PCT results often are associated with abnormal semen analysis. Poor motility can be noted when varicoceles and infection are present. If a varicocele is confirmed by physical examination and semen analysis, high ligation of the internal spermatic vein results in an improvement of motility and a 40–55% pregnancy rate.21
Occasionally, the PCT is abnormal because of sperm immobilization. Nonspecific prostatitis can be treated successfully with trimethoprim-sulfamethoxazole (1 tablet by mouth two times a day for 1–2 months) or, if ureaplasma or Chlamydia infection is suspected, with doxycycline (206 mg by mouth the first day, then 100 mg by mouth four times a day for 9 days).22 Although ureaplasma and Chlamydia infections have been proposed as factors contributing to poor PCT, recent studies have found no correlation.23, 24 Immunologic immobilization of sperm in the endocervical canal can occur, but this diagnosis must be confirmed by immunologic tests.1, 2, 25, 26, 27
I also have seen a few instances of poor sperm penetration in patients with grossly normal-appearing cervical mucus. Immunologic test results were negative, but when the pH of the mucus was determined, it was very acidic. In vitro, this mucus can be dialyzed to a normal pH, allowing normal sperm penetration. The activity of the cervical mucus can be improved by an alkaline douche28 or by high-dose estrogen therapy (discussed below).
Altered cervical mucus
Preovulatory cervical mucus has the following characteristics: (1) it is thick, opaque, and cellular; (2) it has a poor spinnbarkheit; and (3) it is found in approximately 60% of abnormal PCTs. Repeated cervical bleeding during mucus collection may indicate anatomic defects or cervicitis. Colposcopic examination sometimes reveals a poorly developed endocervical canal with thin, columnar epithelium; this has been successfully treated with cryosurgery. A very cellular cervical mucus often represents cervicitis, which should be treated with antibiotic therapy after appropriate cultures are obtained. If the infection is not resolved by systemic antibiotic therapy, cryosurgery can be employed.
In most of these patients, poor cervical mucus is not secondary to infection but represents a partial or total lack of response of the cervical crypts and glands to estrogen stimulation. The impaired function in these cases may be a late sequela of an inflammatory process or a consequence of surgical procedures such as conization, amputation, or electrocoagulation (loop electrical excision procedure [LEEP]) of the cervix. In many cases, however, no etiology can be determined.
Treatment
Treatment of poor cervical mucus is best accomplished with low-dose estrogen (0.1 mg diethylstilbestrol, 0.625 mg conjugated estrogen, or 50 μg ethinyl estradiol) for the 14 days before ovulation. In a 28-day menstrual cycle, this would be from day 1 to day 14. There is no advantage to continuing the hormonal therapy during the luteal phase. This treatment markedly improves the quality of cervical mucus in approximately 40% of patients.2 After the quality of the cervical mucus is corrected, the PCT should be repeated.
It should be mentioned that in some patients receiving clomiphene (Clomid) therapy there is a persistent antiestrogen effect on the cervical mucus. Once the ovulatory dose of clomiphene is achieved, low-dose estrogen therapy is given for 7 days following the 5 days of clomiphene. Another antiestrogen, tamoxifen (Nolvadex), has been recommended in place of clomiphene for patients in whom clomiphene produces a persistent antiestrogen effect on the cervical mucus.27
In some patients, human menopausal gonadotropin-human chorionic gonadotropin (HMG-HCG) therapy has been successfully used to induce higher endogenous estrogen levels. This results in greater cervical mucus production and is successful, but it requires close monitoring.20, 29
Relative dysmucorrhea
Lunenfeld and Insler3 have interpreted these problems as either relative or absolute dysmucorrhea, depending on whether or not the cervical mucus is responsive to high doses of estrogen therapy, respectively. In patients who do not respond to low-dose estrogen therapy, I have used an altered version of their therapy (Fig. 6) as follows:
- For the first week, ethinyl estradiol (50 μg/day) is given: a PCT is done on day 12 of the cycle.
- The dosage is increased for another week (150 μg/day) and the PCT is repeated. Abundant cervical mucus should be obtained.
- A progestin is then added to accomplish withdrawal bleeding.
|
This cycle is of course lost for conceptive purposes because of the high-dose estrogen therapy. The purpose is to see whether the cervical crypts and glands will respond to this therapy. Lunenfeld and Insler3 originally described this as a diagnostic procedure, but I found it useful therapeutically. This therapy is successful in a majority of patients. After the one cycle of therapy, the pre-ovulatory cervical mucus is assessed again by PCT during the subsequent spontaneous cycle. Most patients continue to have good cervical mucus production after this therapy cycle. Full scientific evaluation of this therapeutic mode requires the collection of a larger amount of clinical data.
Absolute dysmucorrhea
The only therapy available to overcome the barrier of unresponsive thick cervical mucus is IUI.1, 2, 19 In fact, IUI techniques have essentially replaced both estrogen therapy and cervical insemination as a means of treating the cervical factor in infertility.19, 20, 30 A sterile polyethylene tube (No. 16 intercatheter), a Jones in vitro fertilization (IVF) catheter, or a Tefcat catheter (Monoject: Shearwood Medical, St. Louis, MO) attached to a tuberculin syringe, is threaded through the cervix. In the past, only 0.2 mL of whole semen was used because a larger quantity could produce an anaphylactic-type reaction and strong uterine contractions. Recently, the use of washed motile sperm instead of whole sperm has been proposed.2, 19, 29 In performing the IUI, the spermatozoa can be prepared for insemination by different washed sperm and sperm-selection techniques.2, 19, 20, 29
Before ending this section, it should be mentioned at this point that although the previous section established a basis and method of evaluation that resulted in the useful clinical approach noted in this section, not all literature agrees with this approach due to the questioned predictive value of the PCT and the advent of IUI, IVF, and intracytoplasmic sperm injection (ICSI). Recent literature noted poor predictive value of the PCT in a randomized trial which concludes that PCT results are largely irrelevant because they seldom changed clinical management.31, 32, 33, 34 In addition, current therapy for unexplained infertility generally includes IUI often in combination with ovarian stimulation20, 29 and of course IVF as treatment for oligospermia or unexplained infertility. Both treatments negate any recognized or unrecognized cervical mucus factor.
CONCLUSIONS
The importance of cervical mucus as a conduit for sperm migration through the female genital tract is evident. The clinicial evaluation of the cervical factor has been established since Sims–Hubner in the infertility work-up. By initiating a standardized, well-defined postcoital evaluation, one can determine the degree of estrogen stimulation, the adequacy of insemination, and the interaction between male and female secretions. In this manner, different factors can be identified and treatment modalities initiated. While the PCT can provide the above information, it can also be prognostic to an extent;15, 35 however, it is mainly a test of performance.
Griffith and Grimes36 and Oei et al.37 do not acknowledge the PCT as a test of performance, criticizing it as having poor validity, a lack of standard methodology, established definition of normal, an unknown rate of reproducibility, and poor predictive value. Also, current therapy for explained infertility most often includes IUI in combination with ovarian stimulation20 and IVF31 as treatment for oligspermia or unexplained infertility. Both therapies negate the necessity of cervical mucus evaluation. Thus many would conclude that routine postcoital38 testing is unnecessary in current practice and that its time has passed. Despite this criticism, if IUI, ovulation induction, and IVF are not readily available, then the postcoital test can be of benefit.39, 40 Since the primary role of the PCT is to evaluate the ability of sperm to penetrate the cervical mucus and eventually to migrate to the site of fertilization, it can play a role in the management of infertility. The limitations of the PCT must be recognized since fertilization is not an all-or-nothing phenomenon because sperm can be recover from the peritioneal cavity in patients with a negative PCT.41
REFERENCES
Speroff L, Glass RH, Kase NG: Investigation of the infertile couple. In Speroff L, Glass RH. Kase NG (eds): Clinical Gynecologic Endocrinology and Infertility, 4th ed. Baltimore. Williams and Wilkins, 1989 |
|
Davajan V: Postcoital testing. In Mitchell DR Jr. Davajan V. Lobo RA: Infertility, Contraception and Reproductive Endocrinology. 3rd ed. pp 599-61 I. Oxford. Blackwell Scientific Publications. 1991 |
|
Lunenfeld B, Insler V: Infertility, pp 90–104. Berlin. Springer-Verlag. 1978 |
|
Odeblad E: Physical properties of cervical mucus. Adv Exp Med Biol 89:215. 1977 |
|
Doehr SA, Moghissi KS: The mucin of human and bovine cervical mucus. In Blandau RJ, Moshissi KS (eds): The Biology of the Cervix, p 125. Chicago, University of Chicago Press. 1973 |
|
Flori F, Secciani F, Capone A, Paccagnini E, Caruso S, Ricci MG,Focarelli R: Menstrual cycle-related sialidase activity of the female cervical mucus is associated with exosome-like vesicles. Fertil Steril 2007;88:121-9. |
|
Sobrero AJ, MacLeod J: The immediate post-coital test. Fertil Steril 13:184. 1962 |
|
Davajan V, Nakamura RM, Kharma K: Spermatozoan transport in cervical mucus. Obstet Gynecol Surg, 25: 1, 1970. |
|
Gibor Y, Garcia CJ, Cohen MR, Scommegna A: The cyclic changes in the physical properties of the cervical mucus and the results of the postcoital test. Fertil Steril 21:20. 1970 |
|
Perloff H, Steinberger E: In vivo survival of spermatozoa in cervical mucus. Am J Obstet Gynecol 88: 439, 1964 |
|
Danezius J, Sujan S, Sobrero AJ: Evaluation of the post-coital text. Fertil Steril 13:559. 1962 |
|
Tredway DR: Dynamics of sperm transport in the mid-cycle human female reproductive tract. Thesis, University of Southern California. 1964 |
|
Tredway DR, Settnlage DSF, Nakamura R et al: Significance of timing for the postcoital evaluation of cervical mucus. Am J Obstet Gynecol 121:387. 1975 |
|
Tredway DR: The interpretation and the significance of the fractional postcoital text. Am J Obstet Gynecol 124:352. 1976 |
|
Drake TS, Tredway DR, Buchanan GC: A reassessment of the fractional postcoital test. Am J Obstet Gynecol 133:382. 1979 |
|
Corson G, Ghazi D, Kenmann E: Home urinary luteinizing hormone immunoassays: Clinical applications. Fertil Steril 53:591. 1990 |
|
Hall LL, Rice VM: Ovulation predictors and postcoital testing. Int Reprod Med Clin N Am 6: 179, 1995 |
|
Hamilton CTCM, Evers JLH, deHaan J: Ultrasound increases the prognostic value of the postcoital test. Gynecol Obstet Invest 21: 80, 1986 |
|
Kerin J, Quinn P: Washed intrauterine insemination in the treatment of oligospermia infertility. Semin Reprod Endocrinol 5: 23, 1987 |
|
Tredway D, Chan P, Henig I et al: The effectiveness of stimulated menstrual cycles and percoll sperm preparation in intrauterine insemination. J Reprod Med 35: 103. 1989 |
|
Dubin L, Amelar RD: Varicocelectomy as therapy in male infertility: A study of 504 cases. Fertil Steril 26:217. 1975 |
|
Gnarpe H, Friberg J: Mycoplasma and human reproductive failure. 1. The occurrence of different mycoplasmas in couples with reproductive failure. Am J Obstet Gynecol 14: 727, 1972 |
|
Tredway DR, Wortham JWE Jr, Condon-Mahoney M et al: Correlation of post coital evaluation with in vitro sperm. cervical mucus determinations and ureaplasma cultures. Fertil Steril 43:286. 1986 |
|
Battin DA, Barnes RB, Hoffman DI et al: Chlamydia trachomatis is not an important cause of abnormal postcoital test in ovulatory patients. Fertil Steril 42:233. 1984 |
|
Hass GG: The inhibitory effect of sperm-associated immunoglobulins on cervical mucus production. Fertil Steril 46:334. 1986 |
|
Mathur S, Williamson HO, Baker ME et al: Sperm motility on postcoital testing correlates with male autoimmunity to sperm. Fertil Steril 41: 81, 1984 |
|
Roumen FJME, Doesburn LWH, Rolland R: Treatment of infertile women with a deficient postcoital test with two antiestrogens: Clomiphene and tamoxifin. Fertil Steril 4:237. 1984 |
|
Dessole S, Cherchi PL, Buscarinu G et al: Postcoital test after vaginal washing with NaHCO3. Clin Exp Obstet Gynecol 12: 33, 1985 |
|
March CM: Improved pregnancy rate with monitoring of gonadotropin therapy in three modaltries. Am J Obstet Gynecol 156: 1473, 1987 |
|
Steures P, van der Steeg JW, Hompes PGA, Bossuyt PMM, Habbema JDF, Eijkemans MJC, Schols WA, Burggraaff JM, van der Veen F, Mol BWJ: Effectiveness of intruaterine insemination in subfertile couples with an isolated cervical factor: a randomized clinical trial. Fertil Steril 2007;88:1692-6. |
|
Jones HW Jr, Acosta A, Garcia J et al: On the transfer of conceptus from oocytes fertilized in vitro. Fertil Steril 39: 241, 1983 |
|
Allen NC, Herbert CM III, Maxson WS et al: Intrauterine insemination: A critical review. Fertil Steril 44: 569, 1985 |
|
Portuondo JA, Echanojauregui AD, Herran C, Agustin A: Prognostic value of postcoital test in unexplained infertility. Int Fertil 27:184. 1982 |
|
Samberg I, Martin-DuPan R, Bourrit B: The value of the postcoital test according to etiology and outcome on infertility. Acta Eur Fertil 16: 147, 1985 |
|
Tredway DR, Buchanan GS, Drake TS: Comparison of the fractional postcoital test and semen analysis. Am J Obstet Gynecol 130:647. 1978 |
|
Griffith CS, Grimes DA: The validity of the postcoital test. Am J Obstet Gynecol 162:615. 1990 |
|
Oei SG, Helmerhorst FM, Keirse MJ, When is the post-coital test normal? A critical appraisal, Hum Reprod 10:1711, 1955 |
|
Glazener CMA, Ford WCL, Hull MGR: The prognostic power of the post-coital test for natural conception depends on duration of infertility. Human Reproduction 15:1953-1957, 2000 |
|
Matson PL, Tuvile AI, O'Halloran F, Yovich JL: The value of the post-coital test in predicting the fertilization of human oocytes. J In Vitro Fert Embryo Transfer 3: 100, 1986 |
|
Eimers JM, te Velde ER, Geritse R, van Kooy RJ, Dremer J, Habbema JDF:The validity of the postcoital test for estimating the probability of conceiving. AM J Obstet Gynecol 1994;171:66-70 |
|
Stone SC: Peritoneal recovery of sperm in patients with infertility associated with inadequate cervical mucus. Fertil Steril 40:802. 1982 |