A comprehensive discussion of all the physiologic changes that occur in the gastrointestinal tract during pregnancy is beyond the scope of this chapter. However, many basic physiologic alterations need to be discussed so that the physician dealing with gastrointestinal symptoms can better understand symptoms and their significance.
Esophagus and Stomach
Given the common symptoms of nausea, vomiting, and dyspepsia that occur, it is not surprising that the upper gastrointestinal tract is affected by pregnancy. The enlarging uterus displaces the stomach and may anatomically alter the pressure gradient between the abdomen and thorax. Increased pressure within the stomach allows for reflux of the gastric contents into the esophagus, which lies in the negative pressure of the intrathoracic cavity. The pressure gradient may even accentuate a hiatal hernia contributing to gastroesophageal reflux.2 It is for these reasons that the symptoms of heartburn increase as term approaches. Contributing to the increased incidence of gastroesophageal reflux are the motility changes that also occur with pregnancy. Lower esophageal sphincter tone is decreased secondary to increased progesterone levels and a decrease in the peptide hormone motilin.3 These changes may also delay gastric emptying and further aggravate the upper gastrointestinal symptoms associated with pregnancy.
Gastric emptying has been partially studied in pregnancy. Nondyspeptic asymptomatic women have normal solid gastric emptying in early pregnancy, and gastric emptying does not lengthen in the third trimester or postpartum.4,5 Patients, however, with hyperemesis gravidarum do demonstrate prolonged gastric emptying. Studies using gastric ultrasound and acetaminophen clearance in asymptomatic healthy pregnant women at term show normal gastric emptying.6 Electrogastrograms that transcutaneously record gastric myolectric activity have demonstrated abnormal gastric electric rhythms in symptomatic, nauseated pregnant women but not asymptomatic pregnant patients.7
Although alterations in the physiology of the upper gastrointestinal tract increase reflux symptoms, it has been shown that symptoms of peptic ulcer disease may actually decrease. Clark, studying 31 pregnant patients with peptic ulcer, showed that 44% of patients became asymptomatic, whereas another 44% had a reduction in their symptoms.8 During pregnancy the basal and stimulated gastric acid output is decreased secondary to increased levels of progesterone and the increased levels of histaminase produced by the placenta.8 This lower acid secretion coupled with increased protective gastric mucus secretion may cause an improvement in peptic ulcer symptoms.
Small Bowel
The small intestine exhibits decreased motility during pregnancy. Lawson noted that the mean small bowel transit time significantly increased during each trimester (first trimester, 125 ± 48 min; second trimester, 137 ± 58 min; third trimester, 75 ± 33 min) and decreased back to normal levels postpartum. This increased transit time is related to elevations in progesterone levels during normal pregnancy and may contribute to the increased symptoms of constipation in late pregnancy.9
Colon
The many changes that pregnancy exerts on the colon lead to increased symptoms of constipation. The colon may be subject to the same decreases in motility that affect the other portions of the gastrointestinal tract. Progesterone has been shown to alter colonic transit time in rats.10 This effect, however, has not been shown in humans, because many studies show conflicting data regarding progesterone's effect on colonic transit time. The functional changes that occur with the enlarging uterus may mechanically limit colonic emptying and probably is the main reason for symptomatic constipation in late term. There is also a significant increase in water and sodium absorption secondary to the increased aldosterone levels during pregnancy, leading to reduced stool volume and prolonged colonic transit time.
Gall Bladder
There is an increased risk of gall stone formation in pregnancy. The risk of gallstones is related to parity. Two pregnancies double the risk, and four quadruples the risk.11 In women followed-up throughout pregnancy, gall stones form in approximately 5%, and at least one third of these stones redissolve postpartum.12 Although many studies support the risk of cholelithiasis, it is still unclear why gallstones occur. Bile stasis within the gallbladder leading to the supersaturation of cholesterol and the nucleation of cholesterol crystals are important factors in the formation of gallstones. Pregnancy has been shown to effect biliary motility and cholesterol secretion. The fasting volume and residual volume in the gallbladder are increased during pregnancy, promoting bile stasis.13Gall bladder stasis progresses during the first 20 weeks of pregnancy and seems to level off until delivery, when gallbladder emptying normalizes. These effects are most likely secondary to high levels of progesterone during pregnancy. Although estrogens have not been shown to alter biliary motility, they do have a role in promoting gall stone disease. In a study looking at the effects of estrogen supplementation in a nonpregnant population, it was shown that biliary secretion of cholesterol was increased by 40%.13 Increased cholesterol creates a high lithogenic index, promoting formation of gall stones. In addition, pregnancy induces a down-regulation of contractile G proteins in gallbladder muscle, resulting in impaired gallbladder emptying.14
Nausea and Vomiting
Nausea and vomiting are common in the first trimester of pregnancy and may be the first sign of pregnancy. It usually peaks at approximately weeks 10 to 15 of gestation and resolves at approximately week 20.1 Nausea of pregnancy is more common among women who are primagravid, younger, less educated, and overweight. In general, first trimester vomiting is not deleterious to mother or fetus. When vomiting is prolonged, intractable, and interferes with nutrition and fluid intake, it is termed hyperemesis gravidarum (HG). Vomiting may be severe enough to cause weight loss, electrolyte abnormalities, and acid–base disturbances requiring hospitalization. While nausea and vomiting occur in 50% to 90% of all pregnancies, hyperemesis gravidarum is uncommon and has an incidence varying from .5 to10 per 1000 pregnancies.15 HG is more common in nulliparous patients, twin pregnancies, and women younger than 35.16 Nausea and vomiting in pregnancy can be secondary to other disease processes including appendicitis, pancreatitis, cholecystitis, and peptic ulcer disease. These disorders must not be overlooked because delay in diagnosis could be disastrous
The pathogenesis of nausea and vomiting in pregnancy is still undetermined, although many believe the hormonal changes that occur during pregnancy are most likely involved.17 Estrogen may play a key role, because patients with higher estrogen levels (nulliparous, obese, nonsmoking) have more nausea and vomiting. However, nausea and vomiting are more prevalent in the first trimester when estrogen levels are lower compared with the third trimester when estrogen levels are higher. Progesterone has also been implicated in slowing transit time in the bowel. The pathophysiologic significance of progesterone inducing nausea/vomiting is limited by the fact that symptoms improve as term approaches and progesterone levels increase. Another hormone, human chorionic gonadotropin (HCG), which is present in its highest concentrations during the first trimester, may be a more likely cause. The levels of HCG are increased during molar pregnancies, in which nausea and vomiting are common. There is, however, no clear relationship between levels of HCG in molar pregnancy and the presence of vomiting.15,16 Transient hyperthyroidism may be seen in 70% of pregnancies with HG.18 The increase in thyroid hormones is caused by high HCG concentrations or hypersensitive thyrotropin receptors in the thyroid gland.19
The relationship between Helicobacter pylori infection and hyperemesis has been extensively investigated in pregnancy, and results are inconclusive. Although some studies clearly indicate an increased seroprevalence of antibodies to H. pylori in symptomatic pregnant women, the findings have to be interpreted in the context of geography and socioeconomic status. The spread of this infection is clearly related to such factors as local levels of hygiene and public health support as well as socioeconomic status. These factors and the lack of correlation of infection with severity, duration, or type of symptoms make the relationship between H. pylori infection and HG suspect.20,21
The treatment of nausea and vomiting of pregnancy depends on the severity of the symptoms and ranges from changes in dietary habits to hospitalization with hyperalimentation and fluid resuscitation. For mild nausea and vomiting, a change in diet may be all that is needed. Conventionally, antiemetics have been avoided in the first trimester. Because of its relative safety, pyridoxine (vitamin B6) has been frequently used. Vitamin B6 administered at a dose of 25 mg orally every 8 hours improved severe nausea and decreased vomiting significantly in a double-blind placebo-controlled study.22 The explanation for this response is unknown, although it has been linked to many reports showing B6 deficiency in patients with HG. Once dehydration is corrected, the patient should be started on small frequent water feedings with a gradual advancement to frequent small volume carbohydrate meals. If symptoms are intractable, phenothiazines or metoclopramide may be used, because they have been shown to be safe in the second and third trimesters. Antihistamines such as promethazine, chlorpromazine, and meclizine may be helpful and are safe in pregnancy.23
Continuous intravenous droperidol and bolus diphenhydramine have been reported to be beneficial.24 Corticosteroids may be used for patients refractory to standard therapy. A short course of methylprednisolone at 16 mg three times daily for 2 weeks has been successful in terminating vomiting.25 Whereas medication may alleviate some of the symptoms, it is important to realize that the most important intervention is fluid and electrolyte replacement. It is the aggressive treatment of these disturbances that has greatly affected the decrease in mortality of hyperemesis gravidarum. Today, HG is rarely a cause of maternal mortality, compared with the 1930s when mortality was approximately 159 per million.26
Prolonged periods of hospitalization with total parenteral nutrition may be required when treatment with standard crystalloid solutions fail to maintain a normal metabolic state. Psychosocial factors may play a role in the pathogenesis of hyperemesis gravidarum, and many have advocated various psychotherapeutic strategies with some success (hypnotherapy, biofeedback).27 These therapeutic modalities can be a viable adjunct to fluid and nutritional therapy.
Gastroesophageal Reflux
Heartburn and regurgitation in pregnancy are almost ubiquitous symptoms, occurring in 50% to 90% of all pregnancies, but typically mild, becoming severe in only a small percentage of women.28 The peak incidence of heartburn is in the third trimester and resolves with delivery. The risk of symptomatic gastroesophageal reflux is related to increasing gestational age, presence of heartburn prepartum, and parity.29 Heartburn is not caused by reflux itself, but to the effect of the refluxed gastric contents on the distal esophageal mucosa. Endoscopically, the esophagus may appear normal in a patient with severe pyrosis; this disparity has been explained by subtle histologic changes, perhaps allowing exposure of submucosal nerves to irritating gastric contents.
The pathophysiology of gastroesophageal reflux is a complex interplay between the lower esophageal sphincter (LES), the esophagogastric angle, and the esophageal clearance of acid. LES pressure decreases and remains low during pregnancy, reaching its nadir at 36 weeks, and returning to normal after delivery.30 Ambulatory 24-hour pH monitoring demonstrates frequent episodes of supine and upright reflux during pregnancy that resolve postpartum.31 The LES responds to various physical, chemical, pharmacologic, and hormonal agents. For example, the LES is increased by cholinergic stimulation, cisapride, metoclopramide hydrochloride, and gastrin, and it is decreased by smoking, chocolate, anticholinergics, and secretin. The LES response to physiologic stimuli is also affected by pregnancy, and hormonal changes may be very important. The LES responses to stimulation by acetylcholine and gastrin are blunted by estrogen and progesterone in the experimental animal,32 and the administration of estrogen and progesterone to normal menstruating women significantly decreases LES pressure.33
Progesterone seems to mediate LES relaxation, but estrogen is a necessary primer.34 An expanding uterus and increased intraabdominal pressure have been assumed to be important factors in promoting gastroesophageal reflux, especially late in pregnancy. Although the expanding uterus may play some role in displacing or altering the esophagogastric angle, the role for increased abdominal pressure as an important factor in promoting reflux has been refuted. Studies in men with cirrhosis with tense ascites show that increased abdominal pressure actually causes a compensatory increase in LES pressure.35 This compensatory response may be lost in women with preexisting gastroesophageal reflux who were minimally symptomatic before pregnancy.
Reflux symptoms are limited to the duration of pregnancy and have no adverse effect on the mother or fetus. Complications caused by gastroesophageal reflux such as peptic stricture or bleeding are rare during and after pregnancy. Although subtle histologic changes may be noted on esophageal biopsy, visible mucosal damage is rarely noted on endoscopy.36
Diagnosis of gastroesophageal reflux is based on clinical symptoms and endoscopy, although rarely necessary, is the diagnostic procedure of choice. The safety of endoscopy is discussed more fully in a subsequent section of this chapter.
Lifestyle modifications certainly have a role to play in treating gastroesophageal reflux. Dietary measures such as limiting oral intake within 3 hours of bedtime, increasing frequency and reducing volume of meals, reducing dietary fat, and eliminating caffeine, chocolate, and mints are measures that have some effect in controlling the symptoms of gastroesophageal reflux. Alcohol and smoking should be eliminated. Elevation of the head of the bed and avoiding prolonged recumbency are additional lifestyle measures of some benefit.
If lifestyle modifications do not control symptoms, the next step would be the use of systemic oral antacids. These agents are safe in pregnancy and should be used in appropriate dosing (e.g., two tablets or 30 mL 1 and 3 hours after meals). Potential adverse effects are rare but do include reduced iron absorption, sodium and fluid retention, and the potential for metabolic alkalosis in the mother and fetus.37 Magnesium-containing oral antacids should be avoided in the last trimester of pregnancy in view of the theoretic possibility of magnesium induced slowing of labor.
Sucralfate is not absorbed and appears to be quite safe in pregnancy, without any teratogenic or impaired reproductive effects in rodents, and has successfully controlled symptoms of gastroesophageal reflux in pregnant patients.38 Each gram of sucralfate contains 207 mg of aluminum, but absorption of this orally administered drug is negligible and needs to be avoided only in pregnant patients with renal failure in whom the potential for aluminum toxicity exists.
Histamine H2-receptor antagonists are the mainstay of treatment in gastroesophageal reflux in pregnant patients whose symptoms do not respond to lifestyle measures or oral antacids. Teratogenic studies in animal have shown no adverse effects with cimetidine, ranitidine, or famotidine and all are FDA category B during pregnancy. No increase in congenital malformations was noted in a cohort of 178 pregnant women who used H2-receptor antagonists during the first trimester of pregnancy.39 Most patients used ranitidine (71%), although cimetidine (16%), famotidine (8%), and nizatidine (5%) were also used. H2-receptor antagonists do cross the placenta and are excreted in breast milk40,41 but are probably safe to use during breastfeeding. Studies in rodents showed some antiandrogenic activity of cimetidine to male offspring. This effect was not seen with ranitidine.42 Famotidine has the lowest concentration in breast mild and may be the preferred agent. Nizatidine was associated with growth retardation in rat pups reared by lactating rates administered nizatidine.43,44
Proton pump inhibitors are very potent suppressors of gastric acid and have made a major impact in the treatment and healing of severe peptic esophagitis, but their use in pregnancy has not been as extensive as H2-receptor antagonists. Omeprazole has some potential for teratogenicity, causing dose-related embryo toxicity (used in doses 17–172-times the usual human dose!) in animals44 and is categorized as a class C drug by the FDA. A multicenter prospective controlled trial in 113 pregnant women, however, showed no increased risk of fetal malformations or poor pregnancy outcome with the use of omeprazole.45 The other proton pump inhibitors are class B drugs and a meta-analysis has confirmed their safety in pregnancy.46 Although proton pump inhibitors seem quite safe they should be used primarily in patients with gastroesophageal reflux disease not responsive to H2-receptor antagonists. Many patients with gastroesophageal reflux will respond to standard antisecretory doses of H2-receptor antagonists, but some patients will continue to experience symptoms unless acid suppression is very substantial. Acid suppression approaching the level achieved with proton pump inhibition can be achieved by increasing the dosage of an agent such as ranitidine (e.g., ranitidine 300 mg twice daily), which does not have any clear dose-related toxicity. Continued use of H2-receptor antagonists may induce tachyphylaxis and require progressive escalation of dosage to maintain therapeutic effect.
Promotility agents may have a limited role to play in symptomatic gastroesophageal reflux and could be added if acid suppression alone does not work. Metoclopramide does cross the placenta but does not harm the fetus47 and probably can be used during pregnancy, although its therapeutic efficacy is modest.
Peptic Ulcer Disease
Peptic ulcer disease is no more common in pregnancy than in other normal populations and older epidemiologic studies suggest a decreased incidence in pregnancy.48 In fact, there is evidence to suggest that pregnancy ameliorates the symptoms of peptic ulcer. Clark interviewed 313 pregnant patients with peptic ulcer and noted that 44% became asymptomatic, 44% had improved dyspepsia, and 75% had recurrent symptoms postpartum.49 Many physiologists believe that increased levels of progesterone reduce both basal and stimulated acid production, thus decreasing acid related symptoms. It is also believed that increased levels of histaminase produced by the placenta also contribute to the decreased acid secretion. Gastric secretory data are scarce, however, and Van Thiel reported no difference in basal and peak acid production at various stages of pregnancy in four women with a previous history of peptic ulcer.30
Now that it is clear that H. pylori plays a pivotal role in peptic ulcer disease, the relationship of H. pylori and pregnancy continues to be investigated. Infection with H. pylori is quite high in patients from the nonindustrialized world and among women of less advantaged socioeconomic classes. Overall, however, the incidence of H. pylori infection is decreasing and the seroprevalence in pregnant French women decreased from 19% in 1990 to 11% in 1999.50 Nonetheless, more than 90% of ulcer disease in patients not using nonsteroidal antiinflammatory drugs (NSAIDs) occur in patients with chronic active gastritis caused by H. pylori.51 Given the importance of this bacterium in ulcer pathogenesis, testing for this organism should be performed in all patients with peptic ulcer. This can be performed noninvasively through serologic testing, urease breath testing, and stool antigen analysis, as well as through histology and rapid urease testing during endoscopy. Once H. pylori is found, antibiotic eradication therapy will cure patients with peptic ulcer. Pregnant patients with peptic ulcer who test positive for H. pylori present a difficult problem because the eradication regimens have not been studied during pregnancy. These regimens consist of triple and double antibiotics in combination with proton pump inhibitors. Given the perceived risks of treatment eradication therapy probably should be postponed until after delivery. Maintenance H2 receptor antagonists or proton pump inhibitors will prevent recurrent ulcer in most patients until eradication therapy can be performed postpartum. If ulcer disease is complicated or unresponsive to antisecretory therapy, metronidazole and amoxicillin have been shown to be safe in pregnancy and are categorized as class B drugs in pregnancy and can be combined with a proton pump inhibitor for a 14-day course to eradicate H. pylori. Other antibiotics effective in eradicating H. pylori such as clarithromycin (class C) and tetracycline (class D) should probably be avoided in pregnancy except in extraordinary circumstances.
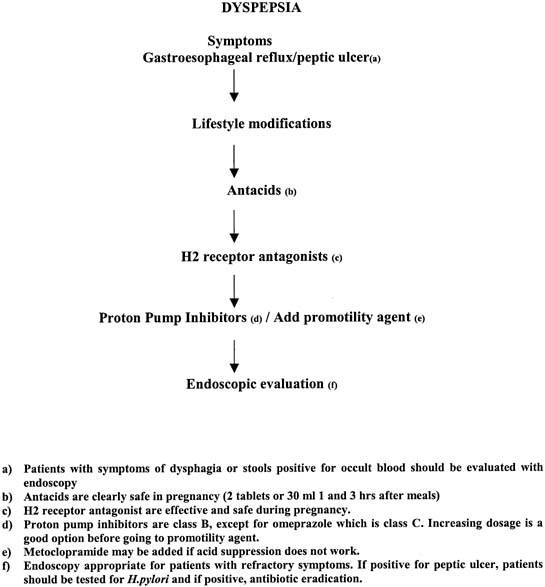
The mainstay of treatment is lifestyle modification and avoidance of medical intervention. If the patient is infected with H. pylori treatment should ultimately be directed to eradicate this infection. Dyspeptic symptoms may be caused by essential dyspepsia, peptic ulcer disease, or gastroesophageal reflux. Aggressive diagnostic testing in uncomplicated cases is unwarranted and empiric therapy to control symptoms is the appropriate approach. The patient should be advised to abstain from smoking, alcohol, aspirin and NSAIDs. As these symptoms may be difficult to differentiate from gastroesophageal reflux much of the same advice is given (small meals, no late-night snacks, and avoidance of fatty foods, acidic citrus drinks, caffeine, chocolate). The comments regarding treatment modalities in gastroesophageal reflux in pregnancy noted earlier apply to the treatment of peptic ulcer and dyspepsia as well. If symptoms fail to resolve with these conservative measures, antacids may be used safely. Sucralfate, a sulfated polysaccharide complex with aluminum oxide is safe and effective in pregnancy. It binds to the proteinaceous surface of an ulcer. If symptoms persist H2 blockers can be used. All H2 receptor blockers (cimetidine, ranitidine, famotidine, nizatidine) are rated as category B drugs during pregnancy. Studies in rates suggest that cimetidine has some potential for fetal antiandrogenic effects.52,50 A large surveillance study of 229,000 pregnant Michigan Medicaid recipients did not reveal any significant teratogenic effects in newborns exposed to cimetidine, ranitidine, or famotidine.53,49 Proton pump inhibitors very effectively suppress gastric acid secretion through inhibition of the H+K+-ATPase pump and can be used to control symptoms of peptic ulcer. Five are available (omeprazole, lansoprazole, pantoprazole, rabeprazole, and esomeprazole) and all are category B in pregnancy except for omeprazole, which is rated C. Misoprostol, a synthetic prostaglandin E1 analogue with antisecretory and cytoprotective properties, is category X and is an abortifacient. If the symptoms are refractory to the aforementioned interventions, then upper endoscopy is warranted to establish the diagnosis and rule out complications. Complications of PUD such as perforation and hemorrhage should be treated in the same fashion as those in a nonpregnant patient, because delays in diagnosis and treatment can pose an increased risk to the mother and fetus (Fig. 1).
Gastrointestinal Hemorrhage
As noted in the section dealing with peptic ulcer, symptomatic peptic ulcer is rare in pregnancy and gastrointestinal bleeding from ulcer is also rare. Many diseases responsible for overt, symptomatic gastrointestinal bleeding in the general population (e.g., malignancy, angiodysplasia, and diverticulosis) occur in older individuals and are rare in the pregnant woman. The most common form of upper gastrointestinal bleeding in the pregnant patient is the Mallory-Weiss syndrome.54 This lesion characterized by a mucosal laceration just below the gastroesophageal junction is a result of increased abdominal pressure and emetic shearing forces on the distal esophagus during vomiting.
The most common cause of lower gastrointestinal bleeding is hemorrhoids. Hemorrhoids may be caused by a prolapse of anal canal cushions, which are rich in blood vessels. The increased circulating blood volume, increased abdominal pressure, and venous stasis caused by the enlarging uterus during pregnancy are contributing factors. It is not surprising that bleeding may occur with straining at defecation. Coupled with the frequent constipation of late pregnancy, this can be quite distressing. External hemorrhoids occur distal to the anal dentate line and rarely bleed unless thrombosed. Internal hemorrhoids are classified by degree: first-degree hemorrhoids bleed but do not prolapse beyond dentate line; second-degree hemorrhoids protrude beyond the dentate line with straining but retract; third-degree hemorrhoids are prolapsed continuously but can be reduced manually; fourth-degree hemorrhoids are permanently prolapsed.55 If suppositories, sitz baths, and increased fiber of stool softeners are not effective, removal of hemorrhoids with thermal application or elastic ligatures may be necessary.
Inflammatory bowel disease, particularly ulcerative colitis, account for lower gastrointestinal bleeding in some women. Patients with mild ulcerative colitis often pass blood and mucous with normal stools. As the colitis becomes more severe and spreads proximally, diarrhea occurs. Profuse hemorrhage is one of the complications of ulcerative or Crohn's colitis and may lead to emergency colectomy. Regional enteritis of the small intestine rarely causes profuse hemorrhage but may cause iron deficiency anemia. In young people, hemorrhage from a Meckel's diverticulum in the small intestine can occur and may be diagnosed with a technetium-labeled nuclear scan if the bleeding is severe enough to justify this modest radiation exposure.
Inflammatory Bowel Disease
The term inflammatory bowel disease (IBD) is frequently used to describe two entities, ulcerative colitis and Crohn's disease. Ulcerative colitis is a chronic recurrent disease that is characterized by diffuse mucosal inflammation occurring in the colon. The disease usually begins in the rectum and spreads continuously throughout the colon. Crohn's disease is also a chronic recurrent inflammatory disease, which may affect the whole alimentary canal. The inflammation is transmural with a patchy distribution characterized by “skip lesions.” The incidence of Crohn's disease is 5 per 100,000, whereas ulcerative colitis is slightly more common with a rate of approximately 15 per 100,000. The peak age of onset for both is during the childbearing years ranging from approximately 15 to 30 years of age. Questions have been raised about infertility in women with IBD. Female fertility is not reduced in ulcerative colitis and pregnancy rates of 90% have been documented.56 However, Hudson showed that infertility increased from 7% to 25% in women who had undergone colectomy.57 Involuntary infertility may be more common in Crohn's disease.58 Studies show a decrease in the number of children born after the diagnosis of Crohn's disease.59 This infertility may be multifactorial and related to inflammatory involvement of the ovaries and fallopian tubes, dyspareunia, perianal disease, debility, and decreased libido. The role that fear plays cannot be discounted, because many patients are erroneously discouraged from becoming pregnant.
The outcome of pregnancy in inflammatory bowel disease, as well as the influence of pregnancy on inflammatory bowel disease, has been extensively studied. Many large studies have shown that most women with ulcerative colitis and Crohn's disease will proceed to have normal, full-term pregnancies. The level of activity of IBD at conception may affect pregnancy outcome. Ulcerative colitis patients with quiescent disease at conception can be expected to complete a full-term pregnancy 90% of the time.56 In patients with active disease at conception a slightly lower success rate has been documented.57 In Crohn's disease the same pattern is revealed. Patients with quiescent disease do very well, while the success rate in active disease is slightly lower, especially in women with Crohn's disease. Although there is no clear evidence to show what constitutes an appropriately safe period of quiescent IBD before planned conception, most experienced physicians suggest that 3 months of inactive disease is good rule of thumb. Severe exacerbations that require surgery or intensification of medical therapy will lead to higher rates of fetal mortality. It is for these reasons that patients should be counseled to attempt conception during remission. The main priority is to maintain IBD in remission. A healthy mother will have a straightforward pregnancy and a healthy baby. Medical regimens that control and maintain IBD are for the most part safe in pregnancy and postpartum and should be continued without fear.
The effect of pregnancy on the course of IBD has also been well documented. Patients with inactive ulcerative colitis will most likely remain asymptomatic and proceed with a normal pregnancy. The relapse rate of 34% is similar to nonpregnant patients.60 Relapse tends to occur more commonly in the first trimester. In patients with active disease at onset of conception the outlook is not as promising and ulcerative colitis will worsen in approximately 45% and continue in approximately 26%. This increased activity will likely reduce the chances of progressing with a normal term delivery unless medical therapy is intensified. Similar to ulcerative colitis, inactive Crohn's disease will have a relapse rate of 27%, which is very close to the relapse rate of nonpregnant patients.60 In contrast to ulcerative colitis the relapses usually occur in the third trimester and postpartum. Active Crohn's disease will remain active throughout pregnancy and may worsen, also decreasing the chances of a normal pregnancy. As stated previously it is important for patients to plan their pregnancy during disease remission.
The treatment of IBD should be broken down into treatment of quiescent disease and active disease. The critical factor needed to insure a good outcome for mother and fetus is maintenance of remission at conception and during pregnancy. Active disease, not the medications used to treat IBD, poses the greatest threat. Medications that maintain IBD remission should be continued. A number of medicines for IBD have been given safely in pregnancy and this makes the decision to treat IBD quite palatable. Sulfasalazine has an excellent safety record in pregnancy.61 The fact that it readily crosses the placenta and may displace bilirubin during the third trimester causes it to be considered a risk for poor outcome. There is no indication to stop sulfasalazine during pregnancy because disease in remission may flare with discontinuation of the medication. Supplemental folic acid (2 mg daily) should be administered because sulfasalazine inhibits folate conjugase, interfering with folate absorption.
5-Aminosalicylic acid is considered a first-line treatment in IBD. Mesalamine has been shown to be safe during pregnancy. Diav-Citrin reported on a prospective, controlled cohort study of 165 pregnant women exposed to mesalamine during pregnancy without significant differences in rates of live births, miscarriages, terminations, or fetal distress.62
Even though they are associated with congenital malformations in animals, corticosteroids have been shown to be associated with minimal risk. Steroids are very effective in inducing remission in active inflammatory bowel disease and the risk of not using them in active disease is greater than their negligible teratogenic effect. Patients in remission should have the dose tapered to the lowest possible dose that allows maintenance of inactivity.
There are no clear data linking azathioprine or 6-MP with fetal abnormalities. In a retrospective review of 16 pregnancies in 14 patients with IBD receiving azathioprine, no congenital abnormalities were found.63 Many other studies including data from renal transplant patients on azathioprine for immunosuppressive therapy are also encouraging. If azathioprine is currently being used to maintain remission it might be prudent to stop it and alter therapy before conception. If this is not possible, azathioprine can be continued, but the risks and benefits have to be discussed with the patient. Recent observations have raised the issue of the effects of immunomodulator therapy in fathers and the outcome of pregnancy. In a small and retrospective analysis, two spontaneous abortions and two congenital anomalies were noted in a group of 13 pregnancies when the father had used 6-MP within 3 months of conception.64
Cyclosporine is generally considered to be dangerous for use during pregnancy; however, there have been recent case reports documenting its safety and efficacy in pregnancy. The literature regarding its use in pregnancy comes mainly from the transplant literature in which there seems to be a low rate of neonatal complications.65 Currently, it may be indicated for acute steroid refractory disease as an alternative to surgery when the risk for mother and fetus are quite high. Other potent immunomodulators including tacrolimus and mycophenolate mofetil have been used in refractory IBD but there are no data on safety in pregnancy. The data on their use in pregnant transplant patients are favorable.66
Methotrexate is an abortifacient and causes congenital anomalies and should not be used during pregnancy.
Biologic agents such as infliximab have been very helpful in Crohn's disease. This mouse chimeric antibody to tumor necrosis factor successfully heals fistulizing Crohn's disease and induces and maintains disease-free status in many patient with complicated Crohn's diseases. Its use in pregnancy is very limited and more information is needed before firm recommendation can be made. In 34 women followed-up after infliximab infusions for either Crohn's disease or rheumatoid arthritis, 26 live births occurred with one congenital anomaly.67
Metronidazole and ciprofloxacin are the most frequently used antibiotics in IBD. Short courses of these drugs are probably safe in pregnancy.
Most exacerbations can be managed safely with careful monitoring, hydration, nutritional support, and medication. In mild or moderate ulcerative colitis, aminosalicylates, orally or rectally, can be used safely. If the disease does not respond, or if disease is severe, corticosteroids should be used. Depending on the distribution of the disease, either oral or rectal corticosteroid preparations can be used. If the disease does not respond to oral steroids, or becomes severe, hospitalization is required. All oral intake should be discontinued and aggressive hydration should be instituted. Steroids should be administered intravenously in four divided doses of solumedrol 60 mg. Plain films of the abdomen should be obtained to rule out toxic megacolon, and the surgical service should be consulted. If disease does not respond, cyclosporine therapy may be attempted to avoid surgery. Surgery is associated with a significant risk of spontaneous abortion; however, in severe disease it may be the only option for maternal survival.
Crohn's disease is also initially managed with supportive care. Treatment for mild, moderate, and severe disease is similar to the aforementioned treatment for ulcerative colitis. There are some novel treatment options for disease that does not respond to antiinflammatory medications. Elemental diets have been shown to be as effective as steroids in mild to moderate disease. Teahon reported successful treatment of four pregnant patients with active Crohn's disease. All four responded to treatment and delivered healthy infants.68 Oral fish oil preparations have been used in IBD to decrease inflammation and are probably safe during pregnancy, although there are no data. Patients with perianal disease related to Crohn's disease also need special consideration. Cesarean section should be considered for patients with active perianal disease, because some data suggest vaginal delivery, and episiotomy may exacerbate perianal disease and prevent healing.69 Excluding active perianal Crohn's disease, operative delivery should be reserved for obstetric indications.
Endoscopic evaluations are safe in pregnancy and are indicated in the evaluation of IBD in pregnancy. Flexible sigmoidoscopy is usually all that is required and does not put the fetus at risk secondary to the need for sedation. If a full colonoscopy is required conscious sedation seems to be safe, although this is poorly studied. It does seem that meperidine is safer than both diazepam and midazolam.70
Intestinal Obstruction
Intestinal obstruction is relatively rare in pregnancy but is the second most common nonobstetric abdominal emergency. The incidence is 1 in 1500 pregnancies.71 It is extremely rare in early pregnancy but begins to increase between the fourth and fifth month of gestation when the uterus changes from a pelvic organ to an abdominal organ. The peak incidence of bowel obstruction occurs in the eighth month when the fetal head descends in to the pelvis, but it may also occur during delivery or the puerperium when a sudden change in uterine size may shift abdominal anatomic relationships. There is no relation between maternal age or parity and the risk of intestinal obstruction.
The causes of intestinal obstruction parallel the nonpregnant population in that previous abdominal surgery with resultant adhesions accounts for approximately 60% of cases whereas the remaining etiologies include volvulus, Crohn's disease, malignancy, and intussusception.58 Incarceration of hernias is relatively rare in pregnancy because the uterus displaces bowl loop from the inguinal and femoral rings as it enlarges.
Bowel obstruction must be considered in any patient with sever emesis, particularly when associated with cramping abdominal pain, distension, and the inability to defecate or pass flatus. Partial intestinal obstruction may cause intermittent cramping, which is relieved by borborygmi, passing flatus, or defecation. The diagnosis is confirmed by plain abdominal film demonstrating distended bowel loops and air-fluid levels, often with uneven fluid levels in a single loop as a result of pressure. Despite the concern regarding x-rays during pregnancy, the identification of intestinal obstruction needs to be prompt and effective and radiological studies should not be delayed.
Treatment of intestinal obstruction frequently is surgical, and it is probably the delay in diagnosis and treatment that accounts for the overall maternal mortality rate of less than 6% and fetal loss of 20% to 30% noted in some studies.72 Surgical treatment should not be unnecessarily delayed, but occasionally conservative treatment with long, weighted, mercury balloon-filled decompression tubes may be appropriate. Colonic volvulus has been successfully treated with colonoscopy.
Irritable Bowel Syndrome, Constipation, and Diarrhea
The most common gastrointestinal disorder is clearly irritable bowel syndrome. This disorder accounts for nearly 50% of referrals to a gastroenterologist.73 and female patients outnumber male patients three-to-one. The diagnosis of irritable bowel syndrome (IBS) depends on the presence of specific symptoms. The Rome II criteria have a high accuracy in diagnosing this disorder. The presence of abdominal discomfort for 12 weeks or longer, which need not be continuous plus two of three of the following: (1) relief of discomfort with defecation; (2) association of discomfort with altered stool frequency; and (3) association of discomfort with altered stool form. Other manifestations included abdominal bloating, passage of rectal mucus, sense of incomplete evacuation, and temporary resolution of pain with bowel movements. Patients may demonstrate constipation predominant IBS or diarrhea predominant IBS or fluctuate between both. Fever, weight loss, and rectal bleeding are not manifestations of this disorder. There is often a close correlation with stress and symptoms are frequently exacerbated during menses.74
The pathophysiology of IBS is not clear, but disturbances in colonic motility and alteration in colonic emptying, although inconsistently related to symptoms, are noted frequently.75 There is also some evidence that irritable bowel patients may have “visceral hypersensitivity” making them more sensitive to motility induced intestinal spasm and distention.76 In addition, the central nervous system may be at fault with centrally directed changes in gut motor or sensory function. Using positron emission tomography (PET), patients with IBS demonstrate abnormal activation in various regions of the brain.77
IBS rarely begins during pregnancy and typically has been present for years. Functional bowel disease usually improves during pregnancy, especially after the first trimester. In those patients with dyspepsia and nausea, the hormonal changes creating nausea in pregnancy may trigger worsening of symptoms and even possibly lead to a picture resembling hyperemesis gravidarum. Abdominal bloating and constipation are frequent symptoms during pregnancy. The physiologic changes responsible for these symptoms are discussed in the section on gastrointestinal physiology. Approximately one third of women report constipation, particularly in the first and third trimesters.78 By strict definition, constipation refers to the character, not infrequency, of stools so that a hard, dry stool is constipation and a soft stool once per week is not. The average frequency of bowel movements ranges from three times per day to once every three days. Unfortunately, common usage defines constipation as infrequent bowel movements; thus, patients become concerned when their bowel fails to move after a certain number of days. A change in bowel habit often occurs in pregnancy and is usually within the accepted limits of normal.
Distinction should be made between irritable bowel syndrome and functional constipation of pregnancy. Constipation related to irritable bowel syndrome is accompanied by a sense of abdominal distension, bloating, and lower abdominal pain. Functional constipation relates to a number of factors, including both qualitative and quantitative changes in activity and diet. The pregnant woman may rest more and eat less because of the pressure of the expanding fetus within the abdomen. In addition, there is a certain amount of pressure against the colon, particularly toward the end of pregnancy, with decreased ability to exert intraabdominal pressure in defecation.
The concern over a change in bowel habit may lead to the use of laxatives, which could create problems for both IBS and functional constipation. Colonic contractions and spasm may be accentuated by the irritating effect of laxatives. Colonic musculature may become for atonic and ultimately respond only to cathartics. The best approach is the increased use of dietary fiber by regular use of bread, fruits, vegetables, and fruit juice. Nonstarch polysaccharide bulking agents such as psyllium, methylcellulose, or sterculia are quite safe in pregnancy because no systemic absorption occurs. Stool softeners containing docusate are safe but probably less effective than the bulking agents. Osmotic laxatives are recommended for constipation-predominant IBS patients whose symptoms do not respond to fiber. Osmotic laxatives include milk of magnesia, poorly absorbable sugars such as lactulose and sorbitol, and polyethylene glycol in powdered form. Stimulant laxatives should be reserved for relatively intractable cases of constipation. Of the anthraquinone laxative, senna is safe and effective in pregnancy.35 Castor oil has the potential for initiating premature labor. Mineral oil has the potential for interfering with maternal absorption of fat-soluble vitamins, leading to coagulopathy in the neonate. Sodium phosphate may promote salt retention in the mother but probably is safe to use. Magnesium-based laxatives and bisacodyl, as well as saline-based enemas, are safe but may lead to salt and water retention and should not be used in the long-term, because dependency may lead to colonic atony and inertia. Phenolphthalein was recently removed from the market, and bisacodyl is the only diphenylmethane laxative available and can be used orally or as a suppository. Glycerin suppositories are safe but should be used sparingly.
Antispasmodic drugs are the most commonly prescribed medications for IBS. The data supporting their benefit are modest but no studies have assessed their efficacy in pregnancy. Dicyclomine is rated category B and hyoscyamine is category C. Their use should be restricted for patients with refractory pain not responding to other measures. A metaanalysis of multiple randomized, controlled trials of peppermint oil reported some therapeutic success,79 and this agent seems safe in pregnancy.
There are no epidemiologic data on diarrhea in pregnancy. It seems that pregnancy predisposes to constipation and not diarrhea. Diarrhea may occur in pregnant women and the differential diagnosis is probably identical to that in nonpregnant women. Diarrhea may be a component of IBS. Peripherally acting opioid agents such as loperamide are the agents of choice to treat noninfectious diarrhea in pregnancy. Loperamide is safe,80 but diphenoxylate with atropine is associated with fetal anomalies in animals and is rated category C. Infectious diarrhea should be investigated with appropriate stool cultures. The natural history and duration of bacterial enteritis may not be influenced greatly with antibiotics and their use should be reserved for patients with prolonged or dramatic symptoms. Metronidazole (giardiasis, clostridium difficile), fluoroquinolones (effective for most enteric pathogens), erythromycin stearate (Campylobacter jejuni), cephalosporins (Shigella), and ampicillin (Salmonella) are effective and low-risk in pregnancy.
Acute Cholecystitis
Pregnancy increases the risk of gallstones. Gall bladder emptying and motility are decreased during pregnancy, providing the necessary environment of biliary stasis for gallstone formation. Along with these functional changes, the chemical components of bile change during pregnancy. Bile is more saturated with cholesterol and has a decreased bile acid content.81 This leads to an elevated lithogenic ratio, promoting the formation of gallstones.
It is surprising that even though the gall bladder is altered in so many ways, cholelithiasis and its complications are still uncommon during pregnancy. The incidence of gall bladder disease during pregnancy is approximately .02% to .03%, and does not exceed that in the nonpregnant female. Cholecystitis occurs in approximately 1 in 1000 pregnancies, and approximately one-third require surgical intervention.82 The clinical presentation is similar to that in the nonpregnant patient consisting of persistent right upper quadrant pain, nausea, vomiting, fever, and leukocytosis. Fortunately the diagnosis can be confirmed accurately and safely during pregnancy by abdominal ultrasound. Gallstones may also lead to pancreatitis, which occurs in approximately 1 in 2000 to 1 in 10,000 pregnancies. The diagnosis relies on the measurement of serum amylase and lipase in the context of the appropriate clinical scenario (see section on Acute Pancreatitis). The maternal and fetal mortality rates are significant in pancreatitis, ranging from 15% to 60% for the mother and approximately 60% for the fetus.
Biliary colic rarely requires operative intervention and is usually controlled symptomatically with pain medications. Cholecystitis initially can also be managed conservatively with pain medication such as Demerol, intravenous fluids, and antibiotics, with only 30% requiring surgical intervention. Cholecystectomy is postponed until after delivery unless complications arise in which the risk of the disease is higher than the risk of surgery. Early data suggested an increase in fetal loss with open cholecystectomy.83 More recent information is more favorable. McKeller reported nine cholecystectomies without perioperative fetal or maternal losses.84 McKeller showed that fetal loss and premature labor were affected by gestational age. In the first trimester, spontaneous abortion occurred in approximately 12%, with a decrease to 5.6% in the second trimester and 0% in the third trimester. Premature labor was 0% during the second trimester, and 40% in the third.84 If cholecystectomy is needed, it is most advantageous to perform the surgery during the second trimester. Cholecystectomy in the first trimester may be associated with fetal loss and in the third trimester with early labor. Pregnancy was at one time an absolute contraindication for laparoscopic cholecystectomy; however, this procedure is safe and may be the procedure of choice in treating cholecystitis in pregnancy.85 In a review of 23 publications consisting of 60 patients, Barry and Grace documented a fetal loss of 0% and a rate of premature labor of 0%.86 The treatment of pancreatitis and the role of ERCP in gallstone related disease is discussed in the next section.
Acute Pancreatitis
Pancreatitis is rare during pregnancy, usually occurring in the third trimester or postpartum. It is no more common than in the nonpregnant patient and has a similar clinical presentation. Diagnosis relies on clinical presentation and elevation of serum amylase and lipase. The presentation is not altered significantly by pregnancy. Classically, the patients present with midepigastric pain, which radiates to the back. Nausea and vomiting are usually prominent and may be the only symptoms. Serum amylase may be lowered during pregnancy secondary to increased renal clearance.
Although the incidence of pancreatitis during pregnancy is small, it does create significant problems when present. The fetal mortality has been reported to be as high as 60%, with maternal mortality ranging from 15% to 60%. The high mortality is related to the extreme fluid shifts that occur during acute pancreatitis and recent data has shown a decrease in mortality with improved intensive care treatment. Cholelithiasis is the most common cause of pancreatitis in pregnancy, accounting for 75% to 90% of cases, approximately twice the rate in the nonpregnant patient.82,83 Although the changes that occur in the gall bladder that promote cholelithiasis and gallstone pancreatitis are well known, there are little data regarding the physiology of the pancreas during pregnancy. There are limited data showing an increase in secretion of pancreatic enzymes and bicarbonate. Enhanced exocrine secretion may exacerbate pancreatitis regardless of its etiology. Triglycerides increase during pregnancy and may cause pancreatitis in patients with a preexisting hypertriglyceridemia. Alcohol is a rare cause, probably related to abstinence, which is practiced during pregnancy.
Management of pancreatitis during pregnancy is similar to the nonpregnant patient. Therapy revolves around meticulous fluid replacement as hypovolemia is the most common cause of mortality. By making sure that the patient takes nothing by mouth and prescribing antiemetics and analgesics that are appropriate in pregnancy this will control symptoms of nausea, vomiting, and pain. Typically pancreatitis resolves in a few days; however, approximately 10% have complicated disease. There should be a very low threshold for ICU admission given the high mortality for both mother and fetus. Patients whose diseases fail to improve with standard care need more diagnostic testing. Ultrasound, which is safe during pregnancy, is usually used in the initial workup and may help to rule out pseudocyst, abscess, or retained common bile duct stone. If cholangitis or biliary obstruction develops, endoscopic retrograde cholangiopancreatography (ERCP) has been shown to be safe during pregnancy and provides a favorable alternative to surgical common bile duct exploration, which has a high risk of fetal loss. Multiple reports document the safety and efficacy of ERCP during pregnancy.70 Fetal radiation can be limited by maternal lead shielding, dosimeters can be placed to measure radiation exposure, and fluoroscopy can be minimized. ERCP and common bile duct stone extraction can permit cholecystectomy to be performed electively after delivery. Open surgical treatment is reserved for complicated pancreatic disease such as septic necrosis, infected pseudocyst, and hemorrhage. Failure to use the appropriate intervention early is also a major cause of the increased mortality.
Appendicitis
Appendectomy is the most common nonobstetric surgical emergency in pregnancy, occurring in approximately 1 in 1000 pregnancies.87 Symptoms are similar to those in the nonpregnant patient; however, the location of the abdominal tenderness may be different depending on the size of the uterus. The enlarging uterus may shift the appendix from the right lower quadrant to the right upper quadrant, causing confusion in the diagnosis. In addition to the change in location other factors during pregnancy delay the diagnosis. The leukocytosis common during pregnancy decrease its diagnostic usefulness. Symptoms such as anorexia, nausea, and vomiting are common in pregnancy. Given the potential for ambiguous presentation, diagnostic imaging is important in helping diagnose appendicitis. Graded compression ultrasound has a sensitivity of approximately 86% for diagnosis appendicitis in nonpregnant patients.88 Although the sensitivity of spiral abdominal CT scan is 96%, ultrasound is safe during pregnancy and should be used early in the evaluation of abdominal pain during pregnancy.88
The outcome of pregnancy complicated by appendicitis is dependent on the timing of the diagnosis. Early noncomplicated appendicitis has a fetal mortality rate of less than 4% but increases after perforation and may be greater than 30%.89 Maternal mortality rate is approximately 5% in uncomplicated cases and approximately 20% with perforation.90 This increase in mortality compared with nonpregnant patients is probably related to the delay in diagnosis that occurs during pregnancy. If the clinical presentation is suspicious for appendicitis early surgical intervention is appropriate even if the rate of removal of normal appendices increase. The risk of surgery is negligible compared with the risk of waiting and allowing perforation to occur.