Hypothyroidism is defined as the constellation of symptoms and signs resulting from insufficient synthesis of thyroid hormone. The clinical spectrum of hypothyroidism varies from the subclinical form, in which clinical symptoms and signs are absent, to the severe form of myxedema. The term myxedema, often used as a synonym for hypothyroidism, has another connotation: the presence of mucinous edema that can be recognized clinically. Because many patients with hypothyroidism do not show such marked clinical changes, the term myxedema should be applied only to those with severe disease and specific tissue alterations.
Hypothyroidism may occur as a result of intrinsic disorders of the thyroid gland (primary hypothyroidism), lack of normal stimulation of the thyroid gland due to hypothalamic or pituitary disease (secondary hypothyroidism), or peripheral resistance to thyroid hormone, a rare but intriguing syndrome.1,2 More than 95% of cases of hypothyroidism are due to primary thyroid disease (Table 1). The diagnosis in most cases is readily available with the determination of serum thyroid-stimulating hormone (TSH) in the presence of low free thyroxine (FT4). Serum TSH is elevated in cases of primary hypothyroidism and within normal limits in patients with secondary hypothyroidism. Other causes of low FT4 in the presence of normal TSH (“euthyroid sick syndrome”) will be discussed briefly below.
TABLE 1. Etiology of Hypothyroidism
- Primary Hypothyroidism
- Destruction or loss of thyroid tissue
- Primary idiopathic hypothyroidism or primary thyroid atrophy
- Post-131I ablation
- Postsurgical ablation
- Postexternal radiation
- Congenital sporadic thyroid aplasia or dysplasia
- Primary idiopathic hypothyroidism or primary thyroid atrophy
- Thyroid hormone biosynthetic defects
- Iodine deficiency or excess
- Use of antithyroid drugs
- Inherited enzymatic defects
- Iodine deficiency or excess
- Goiter
- Chronic autoimmune (Hashimoto's) thyroiditis
- Endemic goiter
- Infiltrative disease
- Chronic autoimmune (Hashimoto's) thyroiditis
- Destruction or loss of thyroid tissue
- Secondary Hypothyroidism
- Pituitary disease
- Hypothalamic disease
- Pituitary disease
- Generalized thyroid hormone resistance
- Transient hypothyroidism
- Subacute thyroiditis
- Silent thyroiditis
- Postpartum thyroid dysfunction
- Drugs (lithium, iodine, amiodarone)
- Autoimmune chronic thyroiditis
- Subacute thyroiditis
Classification
PRIMARY HYPOTHYROIDISM.
Primary hypothyroidism may result from the destruction of thyroid tissue, biosynthetic defects in T4, or intrinsic disease of the thyroid gland with formation of goiter.3
SECONDARY HYPOTHYROIDISM. An impairment in TSH secretion produces decreased production of thyroid hormone. TSH deficiency is usually accompanied by hyposecretion of other pituitary hormones, such as adrenocorticotropic hormone (ACTH), follicle-stimulating hormone (FSH), luteinizing hormone (LH), and growth hormone (GH). Secondary hypothyroidism includes (1) pituitary hypothyroidism (e.g., pituitary tumor, postpartum pituitary necrosis); and (2) hypothalamic hypothyroidism (e.g., hypothalamic tumors, head injury, granulomatous disease, isolated TSH-releasing-hormone deficiency).
GENERALIZED THYROID HORMONE RESISTANCE.
A rare disorder characterized by reduced target tissue responsiveness to circulating free thyroid hormone (not discussed in this chapter).1,2
TRANSIENT HYPOTHYROIDISM SYNDROME.
Although most hypothyroid patients require thyroid replacement therapy for life, in the past few years the occurrence of transient hypothyroidism has been recognized. In this situation, the patient may experience a period of hypothyroidism in the course of an episode of subacute thyroiditis, painless thyroiditis, postpartum thyroid dysfunction, or following the discontinuation of thyroid therapy in euthyroid patients. Transient hypothyroidism also has been reported in some patients undergoing iodine or lithium therapy. There may be few or no clinical symptoms of hypothyroidism; the diagnosis can be confirmed with thyroid tests. In most of these patients, thyroid levels will return to normal spontaneously, and thyroid medication is not indicated unless the patient is symptomatic; however, patients with transient hypothyroidism should be followed closely because the hypothyroidism could recur and become permanent, such as in cases of postpartum thyroid dysfunction.4 Recently, resolution of hypothyroidism has been reported in a group of patients with chronic thyroiditis, as a result of the disappearance of TSH-receptor-blocking antibodies.5 This mechanism would also explain several reports of spontaneous hyperthyroidism in patients with longstanding hypothyroidism.6
Primary Hypothyroidism
The prevalence of hypothyroidism in women has been reported to be between 2% and 6% of the population in the United States and England. It is three to four times more common in women than in men, and the incidence increases with age.7 In the Framingham study, in persons aged 60 years or more, hypothyroidism was found in 5.9% of women and 2.4% of men.8,9
CLINICAL MANIFESTATIONS.
Chronic thyroid failure develops over a period of many months or years, and many of the initial manifestations (e.g., fatigue, constipation, dry skin, weight gain), are not specific for hypothyroidism, but are frequent complaints in the general population. Mental and physical fatigue are among the first symptoms of most patients with hypothyroidism; this may go unnoticed for some time or may be attributed to other reasons, such as aging.10 With progression of the disease, cold intolerance, slow speech, hoarseness, periorbital edema, and puffiness of the hands and feet become common complaints.
As is the case with hyperthyroidism, thyroid failure involves most organ systems. The degree of involvement depends on several factors, the most important perhaps being chronicity of the condition. Changes in the central nervous system are manifested by a decrease in mental activity, lethargy, and loss of mental concentration. Sleepiness at the end of the day, hearing loss, and mental depression may be prominent manifestations. Paresthesias of the fingers as a consequence of carpal tunnel syndrome may be the first and only manifestation in some hypothyroid patients. The relaxation phase of the deep tendon reflexes is delayed, and this has become a characteristic sign of the disease, although it is present only in patients with advanced symptoms. Hypothyroid patients may present with arthralgia and stiffness of the small joints of the hands, and muscle cramps are not infrequent complaints. On physical examination, the skin may be rough, scaly and thickened and cold to the touch. Hair becomes coarse and brittle, and loss of axillary, pubic, and scalp hair is not unusual in severe cases. Features of periorbital edema may be evident when previous pictures of the patient covering a span of several years are compared.
Bradycardia is noticed in some patients, and the electrocardiogram (ECG) may show a low voltage with nonspecific ST abnormalities. Occasionally a patient may suffer from cardiomegaly due to pericardial effusion or cardiomyopathy.
Gynecologic and obstetric abnormalities are not infrequent in hypothyroid women. Menorrhagia is commonly reported, although the true incidence is unknown. Anovulation is said to be common, although pregnancy with normal fetal outcome is not an uncommon event. If hypothyroidism is not promptly corrected, however, there is a higher risk of pregnancy-induced hypertension and premature delivery.11,12 Most women on thyroid therapy need an increase in dosage during pregnancy.13,14 TSH determinations are advisable in these women when pregnancy is diagnosed. It is strongly advisable to perform thyroid studies in patients with galactorrhea-amenorrhea because primary hypothyroidism is one of the causes of the syndrome.15
LABORATORY DIAGNOSIS.
A decrease in serum FT4 or its estimated FT4 index (FT4I) is characteristic of almost all forms of hypothyroidism, regardless of the cause. Serum TSH concentration is elevated in patients with primary hypothyroidism, and this measurement is the most sensitive test for the diagnosis of primary thyroid failure.16 Serum TSH levels may be elevated in patients with a normal FT4I, and this condition has been called “decreased thyroid reserve,” or subclinical hypothyroidism. It may represent the first indication of primary hypothyroidism in the majority of cases (see below).
A low serum FT4I in the presence of normal serum TSH concentrations is diagnostic of secondary hypothyroidism in ambulatory patients. In hospitalized patients with intercurrent illness, euthyroid sick syndrome must be ruled out.17
Other biochemical abnormalities seen in hypothyroid patients include elevations in serum cholesterol and triglycerides, elevations in serum creatinine phosphokinase, and nonspecific electrocardiographic abnormalities. It is helpful to obtain serum thyroid antibody concentrations to confirm the cause of hypothyroidism; they are elevated in most patients with chronic thyroiditis. Radioisotope studies are not indicated in evaluating hypothyroid patients.
SUBCLINICAL HYPOTHYROIDISM.
The syndrome of subclinical hypothyroidism is characterized by an asymptomatic state associated with normal free thyroid hormone concentrations in the presence of mild elevations in serum TSH levels (up to 20 to 25 mU/L).18 The most common causesare Hashimoto's thyroiditis and post-thyroid ablation (e.g., 131I therapy, surgery). Recognition of this entity is important because in a significant number of such patients, frank hypothyroidism can develop.19 The incidence is higher in women than in men, estimated at 15% to 20% of women older than 50 years.7 In more than 50% of these women, increased thyroid antibody titers are detected. Most patients are asymptomatic, but some present with complaints of fatigue, dry skin, and cold intolerance. Goiter is detected in approximately 30% to 60% of patients.
Subclinical hypothyroidism also may be diagnosed in patients taking insufficient thyroid replacement therapy for the treatment of overt hypothyroidism.20 Medications such as lithium, iodine, and those containing iodine (e.g., amiodarone) may cause mild thyroid dysfunction, particularly in patients with chronic autoimmune thyroid disease.
Some studies have shown subtle abnormalities of organ dysfunction in patients with subclinical hypothyroidism.21,22 Elevations in cholesterol and low-density lipoprotein cholesterol levels and decreases in high-density lipoprotein levels have been reported in some studies, correction being achieved after thyroid replacement therapy. Changes in left ventricular function have been reported as well. In one study,21 left ventricular ejection fraction improved with thyroid replacement therapy. In one double-blind randomized study, patients with subclinical hypothyroidism had fewer symptoms while receiving T4 therapy.23 Because most women are asymptomatic, treatment is controversial; however, because of the rate of progression to overt hypothyroidism in patients with positive antibodies (80% in a 4-year follow-up study19), it is advisable to start thyroid therapy in patients with subclinical hypothyroidism and positive thyroid antibodies.
SCREENING. Although screening for primary hypothyroidism cannot be recommended for every patient, there are patients that are at high risk for developing overt hypothyroidism. Currently, determinations of serum TSH is cost-effective for evaluating patients with the following high risk factors for development of hypothyroidism:
Autoimmune thyroiditis
Goiter
Previous treatment for hyperthyroidism (thyrotoxicosis, see below)
Previous high-dose neck radiation therapy
Current lithium or amiodarone therapy
Type I diabetes mellitus
Postpartum, particularly in combination with a goiter
Other autoimmune diseases (e.g., pernicious anemia, idiopathic thrombocytopenia).
Other risk factors include sleep apnea and hyperlipidemia in adults and failure to grow properly in children. Because the incidence of subclinical hypothyroidism is increased after the age of 50, particularly in women, a case can be made for screening all postmenopausal women (Fig. 1).
|
TREATMENT.
Before treatment is contemplated in hypothyroid patients, a proper diagnosis between primary and secondary hypothyroidism is imperative. In patients with secondary hypothyroidism, a complete evaluation of the hypothalamic-pituitary axis should be made to rule out involvement of other hormones. Isolated TSH deficiency is uncommon.
One of the most gratifying experiences in medicine for the patient as well as the physician is the treatment of hypothyroidism, because all symptoms due to thyroid deficiency resolve with appropriate therapy. Several preparations are available, but regardless of the type of thyroid medication to be used, several principles should be kept in mind before therapy is started:
- Most patients will need lifelong replacement therapy.
- Therapy should be started with a low dosage, especially in the elderly
and those with heart problems, and gradually increased to the full replacement
dosage.
- The goal of any treatment is to achieve euthyroidism, from both the clinical
and the biochemical point of view.
Because the hormonal content in synthetic levothyroxine is more reliably standardized than that of desiccated thyroid hormone, synthetic hormone preparations have replaced desiccated thyroid as the mainstay of thyroid therapy. With very few exceptions, there is no justification nowadays to treat hypothyroid patients with preparations other than levothyroxine. Thyroxine (T4) is deiodinated to triiodothyronine (T3) in extrathyroid tissues in humans; therefore T4 more closely simulates the physiology of normal subjects. It is well absorbed and tolerated and is given in a single daily dose.24 Its half-life is 6 days in normal persons and 8 to 11 days in hypothyroid patients. Some medications (e.g., ferrous sulfate, cholestyramine, sucrosulfate, aluminum hydroxide) have been reported to decrease thyroid absorption in the gastrointestinal tract if taken concomitant with thyroid therapy. Malabsorption and hypertrophic gastritis also may produce a decrease in T4 absorption by the gastrointestinal tract.
Normal serum TSH and FT4I concentrations are the goal of levothyroxine therapy. Studies in the last decade have shown that the amount of levothyroxine needed to produce normal tests is less than that previously recommended. Increased bioviability of levothyroxine preparations and more sensitive TSH measurements are responsible for this adjustment in the dosage. The recommended replacement dose is approximately 120 μg/day ± 40 or approximately 1.7 μg/kg body weight/day.25 The physician should be aware of the potential differences in the levothyroxine content among several generic thyroid preparations available today, although one study has indicated that most, but not all, of the generic brands contain the stated amount of levothyroxine.26
In young and healthy patients, therapy can be initiated with 0.05 to 0.075 mg levothyroxine daily; this amount can be increased every 2 to 6 weeks until the proper dose is achieved. For most patients, by the end of 6 to 8 weeks the full replacement dose is achieved. The serum TSH level is determined 4 to 6 weeks after therapy is initiated, and the dose is adjusted accordingly. Thereafter, patients should be seen at yearly intervals, at which time the dose may be adjusted depending on the thyroid tests results. It should also be kept in mind that as patients get older, they require smaller doses of levothyroxine.27
In older patients and those with heart disease, a more cautious approach is recommended; the initial dose should be 0.025 mg levothyroxine daily, and this dose should be increased every 4 to 8 weeks until full therapeutic effect or normalization of thyroid tests is obtained.28,29
MYXEDEMA COMA.
This is a rare clinical situation that constitutes a life-threatening emergency. Myxedema coma can occur in untreated patients with longstanding myxedema who are under stressful situations, particularly infection. Occasionally, the use of narcotics and analgesics can precipitate myxedema coma in patients with severe hypothyroidism. Clinically, patients present with progressive stupor and coma, seizures, hypotension, hypoventilation, and hypothermia. Respiratory acidosis and hyponatremia are also characteristic findings. Because the mortality is high, aggressive treatment is indicated: An initial dose of 0.3 mg IV levothyroxine is given, followed by an IV dosage of 0.05 to 0.1 mg/day, which is continued until the patient is able to take medication by mouth. Concomitant with levothyroxine administration, 100 mg hydrocortisone should be administered every 8 hours because many of these patients may present with relative adrenal insufficiency, or the hypothyroidism may be due to pituitary or hypothalamic disease. Assisted ventilation may be required, and fluid replacement should be given cautiously.30 A potential cause of hypothyroid coma is the discontinuation of thyroid therapy in hypothyroid patients on thyroid therapy who are admitted to the hospital for severe intercurrent disease. Lack of thyroid hormone for 2 weeks or longer can produce severe hypothyroidism.
PATIENTS ON LONG-TERM THYROID THERAPY.
Thyroid hormone preparations are among the most commonly prescribed drugs. In 1994, approximately 35 million prescriptions were written for thyroid tablets, about 92% for synthetic levothyroxine, and 8% for desiccated thyroid. Thyroid therapy is used for the treatment of hypothyroidism; it is also used for other conditions in euthyroid persons, such as nodular goiters, and empirically for the treatment of obesity, chronic fatigue, hypercholesterolemia, and infertility.28,29 It has been reported in the last few years that doses of thyroid hormones suppressing serum TSH, may produce subtle symptoms of hyperthyroidism such as nocturnal tachycardia, shortened systolic interval time, increased sodium excretion by the kidney, decreased total serum cholesterol, and alterations in liver enzymes.31,32 All the above abnormalities are reversed by normalizing thyroid tests.
One of the most significant clinical findings is the potentially deleterious effect of excessive thyroid therapy on bone metabolism. Hyperthyroidism due to intrinsic thyroid disease or excessive thyroid dosage affects bone resorption and bone formation.33,34 Patients with a history of hyperthyroidism are at an increased risk for bone fractures and tend to have fractures at an earlier age than persons who had never been hyperthyroid. Prompt treatment of thyrotoxicosis reverses bone mineral density. Most studies have shown significant decreases in bone mineral density in patients on thyroid therapy and low or suppressed serum TSH levels. Most of these studies, however, were cross-sectional and therefore confounding factors, such as race, obesity, menopausal status, drug therapy (e.g., calcium, estrogens, diuretics), and previous history of thyrotoxicosis, were not always evaluated. Therefore, although still a controversial issue and until prospective studies become available, it is recommended that women on thyroid therapy have serum TSH maintained within normal limits, thyroid function tests being assessed on a yearly basis.35 The exception are women who require suppressive thyroid therapy (serum TSH < 0.01 mU/L) after ablation therapy for treatment of thyroid carcinoma. In this situation, bone mass should be monitored at regular intervals. Recent evidence suggests that estrogen therapy36 or biphosphonates37 prevent the osteopenia induced by thyroid hormone therapy.
Finally, there are patients on thyroid medication for whom the original indication for thyroid therapy was not medically sound; in such situations and with the patients' consent, the physician may discontinue thyroid therapy for 4 to 6 weeks and repeat thyroid function tests. In cases of true primary hypothyroidism, serum TSH will be high and serum FT4 in the hypothyroid range at the end of this 4- to 6-week period; in euthyroid persons thyroid tests will return to normal limits.38 In some patients, however, it may take many weeks for the TSH to become elevated after being withdrawn from thyroid therapy; therefore it is prudent to repeat the serum TSH test in a few months before a final diagnosis of euthyroidism is confirmed.39
CHRONIC THYROIDITIS.
Hashimoto's thyroiditis (chronic or autoimmune) is one of the causes of goiter or hypothyroidism, or both. The diagnosis is confirmed by the clinical findings and by high titers of thyroid autoantibodies in serum. The disease is seen much more commonly in female patients than in males (4:1). The clinical picture is characterized by a goiter that is firm in consistency, has a tendency to be lobulated, and affects both lobes of the thyroid gland. The histologic changes consist of a combination of diffuse lymphocytic infiltrations, obliteration of thyroid follicles, and fibrosis. The natural course of the goiter is to remain unchanged or to enlarge gradually over many years if left untreated. Most patients develop hypothyroidism over several years. The use of iodine in patients with chronic thyroiditis may trigger the development of hypothyroidism or hyperthyroidism.40,41 Patients and their families have shown an increased incidence of other autoimmune diseases, such as pernicious anemia, insulin-dependent diabetes mellitus, vitiligo, Sjögren's syndrome, rheumatoid arthritis, chronic active hepatitis, and adrenal insufficiency.
Patients with chronic thyroiditis may develop transient thyroid dysfunction during pregnancy and in the postpartum period. They may have mild symptoms of hyperthyroidism 4 to 6 weeks postpartum, with enlargement of the thyroid gland and subsequent hypothyroidism at 3 to 5 months postpartum. These patients will return to the euthyroid state 5 to 10 months after delivery without undergoing specific treatment. It has been proposed that these changes are due to changes in the immune response during pregnancy.3,42
Treatment of chronic thyroiditis with thyroid hormone is used in euthyroid patients to decrease the size of the goiter, although this practice is controversial. In longstanding goiter that is firm on palpation, therapy is usually not effective in reducing its size because the gland is fibrotic. Otherwise, patients are followed yearly to detect any tendency toward hypothyroidism. These patients should be advised to have their thyroid tests checked during pregnancy and in the postpartum period because these are the times when they are at significant risk for development of thyroid dysfunction. Surgery is justified only in the unusual case of local pressure symptoms (e.g., dysphagia, cough, respiratory distress).
Subacute Thyroiditis.
Subacute thyroiditis is an acute, self-limiting viral infection affecting the thyroid gland. On pathologic examination, the gland is enlarged, with an inflammatory reaction involving the capsule. Polymorphs, lymphocytes, and foreign-body giant cells are recognized. Women are affected twice as often as men. The disease is preceded by a protracted phase of low-grade fever, malaise, and muscle aches for 2 to 3 weeks, followed by neck pain that often radiates to the angle of the jaw and to the ear on the involved side. Some patients may complain of dysphagia. The thyroid gland is tender to palpation and enlarged, and sometimes one of the lobes is as hard as stone. In a few days it returns to normal and the opposite side becomes enlarged and tender. Mild signs of hyperthyroidism may develop in some patients. The course of the disease varies from a few weeks to several months, with eventual spontaneous recovery. Patients may experience a period of hypothyroidism before final recovery.43
Diagnostic findings include elevation in serum FT4I and FT3I concentrations and, in most cases, suppression of TSH; there might be a slight elevation in the thyroid antibody titer. Diagnosis is confirmed by an elevation in the erythrocyte sedimentation rate and a low or depressed 24-hour radioiodine 131I thyroid uptake. In the early phase of the disease, treatment consists of analgesics. In patients in whom analgesic medication is ineffective, the use of corticosteroid (e.g., 30 to 40 mg prednisone daily in divided doses) is very effective in controlling symptoms, particularly neck pain. Prednisone dosage may be reduced after a few days and discontinued by 3 to 6 weeks in most cases. In some patients, however, symptoms recur when the amount of glucocorticoids is decreased and has to be increased again to control the pain. Sometimes symptoms may persist for several months. If a patient has significant hyperthyroid symptoms, 10 to 40 mg propranolol three times per day is effective in controlling the symptoms.
A similar clinical picture without thyroid pain has been described. This has been termed “painless thyroiditis,” or silent thyroiditis; its relationship to the classic subacute thyroiditis is not clear. Biopsies in patients with painless thyroiditis have shown lymphocytic infiltrations, rather than the typical histology of subacute thyroiditis. Clinically, more than 90% of patients with silent thyroiditis have manifestations of hyperthyroidism, with elevations in serum T4 and T3 concentrations and suppressed TSH. The 24-hour 131I thyroid uptake is low. The most common symptoms are palpitations, nervousness, weakness, and heat intolerance. Eye signs typical of Graves' disease are absent, although approximately one third have lid lag or lid retraction. The thyroid gland is enlarged and nontender.44 Recovery from hyperthyroidism usually takes 3 to 5 months. Many of these patients go through a period of transient hypothyroidism lasting a few weeks. The course is similar to patients with postpartum thyroid dysfunction.
Multinodular Goiter.
Multinodular goiter can be defined as an enlargement of the thyroid gland characterized by excessive growth and structural or functional transformation of one or several areas within the normal thyroid tissue. The pathogenesis of nodular transformation is not known, although chronic TSH stimulation in thyroid glands with abnormal follicular growth pattern plays an important role, as does iodine deficiency in endemic areas. However, the etiology of sporadic nodular goiter is unclear.45 The prevalence of nodular goiter is 4% to 8% in the adult US population and is more prevalent in women than in men (4:1).
The natural history of nontoxic goiter indicates that a diffuse enlargement of the thyroid may begin in adolescence with a gradual appearance of nodularities. These nodules grow slowly, over several decades, without producing significant clinical difficulties. They are seen more often in women and the elderly. Some goiters will remain quiet and stable, whereas others will keep growing steadily or may regress.46 In some patients, thyroid antibodies may be elevated, indicating that some of these goiters are related to chronic lymphocytic thyroiditis (Hashimoto's thyroiditis).
Most commonly, the diagnosis of nodular goiter is made during a routine physical examination. The patient may be unaware of the goiter. Very seldom, compression or local symptoms are the presenting complaint; occasionally, rapid growth of the nodule or sudden, acute pain indicating hemorrhage into a nodule causes the patient to seek help from the physician.
For the thyroid gland to be readily palpable, there must be a diffuse enlargement about two times the normal size.47 Inspection of the neck is an important part of the thyroid examination because nodules and asymmetry of the thyroid gland can be demonstrated easily in this way, particularly as the patient swallows gulps of water. The consistency of the nodules varies widely, from soft to hard. Thyroid tests are usually normal; however, if the sensitive TSH test is suppressed in the presence of normal FT4 and FT3 values, the possibility of an autonomous thyroid nodule should be entertained. 131I thyroid scanning is helpful in defining the presence of an autonomous or “hot” nodule within a multinodular goiter. Although no therapy is indicated, such patients should be followed closely for the development of hyperthyroidism.
Two complications in the natural history of multinodular goiter deserve discussion: (1) the development of thyrotoxicosis; and (2) the possible occurrence of malignancy in one of the nodules. Thyrotoxicosis in patients with multinodular goiters may develop insidiously, in which case it is difficult to recognize. Exposure to iodides (saturated solution of potassium iodide) therapy, iodine contrast materials, or amiodarone therapy may produce thyrotoxicosis in some patients. Therefore, patients with known nodular goiters should be followed, and thyroid tests should be performed at regular intervals because it may not always be possible to recognize this complication clinically. Ultrasound may be indicated to assess the size of the gland.
There is no evidence in the literature that nodular goiter predisposes the patient to the development of thyroid carcinoma. Carcinoma should be suspected when the thyroid scan shows hypofunctioning nodules, or if there has been a recent increase in the size of one of the nodules; needle aspiration biopsy should be used in such cases.
In some cases, levothyroxine therapy has proved effective in suppressing further goiter growth, although it is unusual to obtain complete regression. It should be kept in mind, however, that giving thyroid therapy to patients with multinodular goiter can lead to thyrotoxicosis in patients with autonomous nodules, in which case the serum TSH is low or suppressed. Therefore, thyroid therapy for multinodular goiter should be used only in patients with normal serum TSH values and only to decrease goiter size.
The indication for surgical therapy in multinodular goiter varies from center to center, but nearly everyone agrees that surgery should be performed only by highly trained surgeons and with facilities for intraoperative examination of frozen section. Surgery is indicated for a goiter producing symptoms, for a suspicion of malignancy, or for cosmetic reasons.48 In euthyroid patients who have scintigraphic evidence of one or several autonomous nodules, no therapy is indicated. These patients should be followed closely, however, because they are at increased risk for development of hyperthyroidism.
Solitary Nodule of the Thyroid Gland. As in the case of multinodular goiters, the finding of a single thyroid nodule is usually incidental during a routine physical examination. It has been estimated that the incidence of clinically detected thyroid nodules in the general population is approximately 4%, women having a fourfold higher incidence than that for men. For the nodule to be palpable, it should be more than 1 cm in diameter. Very seldom does the patient have local symptoms, such as dysphagia, hoarseness, and occasionally acute neck pain, due to bleeding into the nodule.
The discovery of a thyroid nodule always raises the possibility of malignancy. Several factors should be considered when evaluating such nodules. Young persons, particularly those less than 20 years old, have a higher incidence of malignancy. Benign nodules are much less common in men than in women, so nodules found in men, particularly those older than 50, are suggestive of malignancy. Family history is sometimes relevant: It has been reported that 6% of patients with thyroid cancer have a family history of malignant thyroid neoplasm. A nodule detected in a patient with a history of irradiation to the head or neck during infancy or childhood is suggestive of malignancy.49 Rapid nodule growth is an indication for more aggressive investigation.
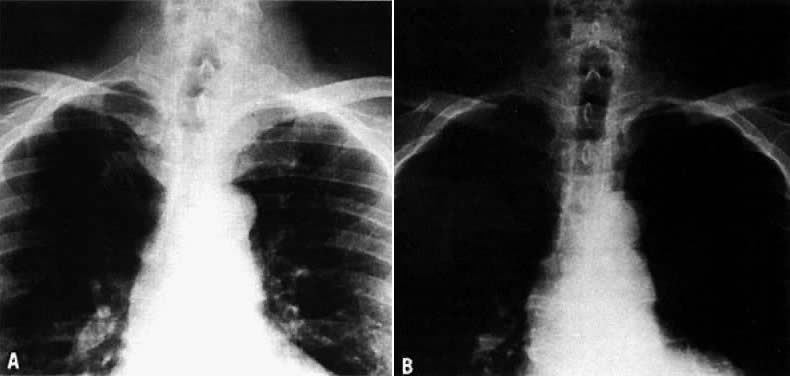
On physical examination, an asymptomatic neck mass is a presenting sign in more than 90% of patients. Cervical lymph nodes, cord paralysis, pain, or dysphagia may indicate thyroid carcinoma. Deviation of the trachea demonstrated on an x-ray is not always an indication of malignancy. A cystic lesion can produce a deviation of the trachea that resolves after aspiration of the fluid (Fig. 2). More than 90% of patients with thyroid nodules are clinically and chemically euthyroid. A little fewer than 10% may have an autonomous or hyperfunctioning nodule evident on a scintigraphic scan, in which case the patient may show symptoms of hyperthyroidism.50
The evaluation of a single thyroid nodule is controversial, and several approaches have been recommended.51,52 As an initial step, some authorities suggest the determination of thyroid tests with thyroid antibodies,51 because the presence of thyroid dysfunction in the presence of a single thyroid nodule is almost always an indication of a benign process, although exceptions occur particularly in “cold” nodules in the presence of Graves' disease.53 The next step suggested is a thyroid scan to determine whether the nodule is hypofunctioning (cold) or hyperfunctioning (warm, hot). Hyperfunctioning nodules rarely harbor cancer. Fine-needle aspiration biopsy of the nodule is indicated for hypofunctioning nodules. Experienced cytopathologists give a correct interpretation in approximately 80% of specimens, and the incidence of false-positive or false-negative results is between 5% and 6%. As suggested by Ingbar,54 “the reading should be performed by a cytopathologist especially interested and experienced in interpretation of the resulting specimens.” Improvement in the sensitivity and specificity of the cytological interpretation of a thyroid nodule has resulted in a higher rate of excision of cancerous nodules and a decline in surgical intervention for noncancerous nodules. In most series reported, 70% of the nodules are benign; approximately 4% to 10% are malignant, 10% indeterminate or suspicious, and 10% insufficient for analysis because of an inadequate biopsy.49
A different approach to the evaluation of thyroid nodules is preferred in some centers, fine-needle aspiration biopsy being the first test used in the presence of a single or predominant thyroid nodule.52,55 If the diagnosis is malignancy, surgical excision is indicated; the type of surgery (lobectomy vs subtotal or total thyroidectomy) depends on the experience and criteria of the surgeon, and a full discussion is beyond the scope of this review.56 After surgery, thyroid suppression with levothyroxine is recommended; surgery is followed by 131I therapy in the presence of either residual tumor detected by thyroid scan or persistent elevation of serum thyroglobulin, or both.57,58 Long-term prognosis for thyroid cancer patients depends on the type of tumor, presence of local or distant metastasis, and other factors.59,60 My own approach to the evaluation of single thyroid nodules is presented in Figure 3.
|
For lesions that are benign on cytologic examination, long-term thyroid suppression therapy has been classically recommended; however, recent observations appear to indicate that thyroid suppression therapy offers no benefit over placebo therapy in reducing the size of the nodule,61 but this issue is still controversial.62 It is my own practice to use thyroid suppression therapy for 3 to 6 months in benign nodules and to continue it if there has been a significant reduction in the size of the nodule. To avoid the potential complications of osteoporosis and subclinical hyperthyroidism, however, the serum TSH should be kept between 0.02 and 0.4 mU/L. After surgery for a benign thyroid nodule, thyroid therapy is indicated for patients in whom postsurgical hypothyroidism develops or for those who had received radiation therapy during childhood for benign conditions. In the latter group of patients, the recurrence rate of thyroid nodules has been reported to be 4.5 times higher in patients not treated with thyroxine therapy.63
Most malignant tumors of the thyroid are papillary or follicular carcinoma, although mixed lesions are not unusual. Undifferentiated carcinoma occurs in the elderly, and the prognosis is poor. Medullary thyroid carcinoma accounts for approximately 2% of thyroid cancer; it may occur alone or as part of the syndrome of multiple endocrine neoplasia in association with pheochromocytomas, parathyroid adenomas, and mucosal neuromas. In patients suspected of having this type of tumor, it is useful to measure serum calcitonin levels because they are characteristically elevated.64