United States
A 1973 report from a prestigious medical journal described an adolescent admitted to a major Boston teaching hospital with what proved to be incomplete septic abortion. Uterine evacuation was not performed until several days after admission because this diagnosis was not initially entertained. The patient died despite massive antibiotic therapy and intensive medical management.3 Tragedies of this sort are now rare.
The most important public health effect of the legalization of abortion4 was the near elimination of deaths from illegal abortion in the United States. Illegal abortion deaths are disproportionately due to infection.4,5 In a 1994 U.S. review, 62% of illegal abortion deaths and 51% of spontaneous abortion deaths were from infection, whereas only 21% of legal abortion deaths were from infection.6 Risk of death from postabortion sepsis is greatest for younger women and unmarried women, and it is more likely with procedures that do not directly evacuate the uterine content.7 With more advanced gestations, the risk of perforation and retained tissue increases.7 Delay in treatment allows progress to bacteremia, pelvic abscess, septic pelvic thrombophlebitis, disseminated intravascular coagulopathy, septic shock, renal failure, and death.8
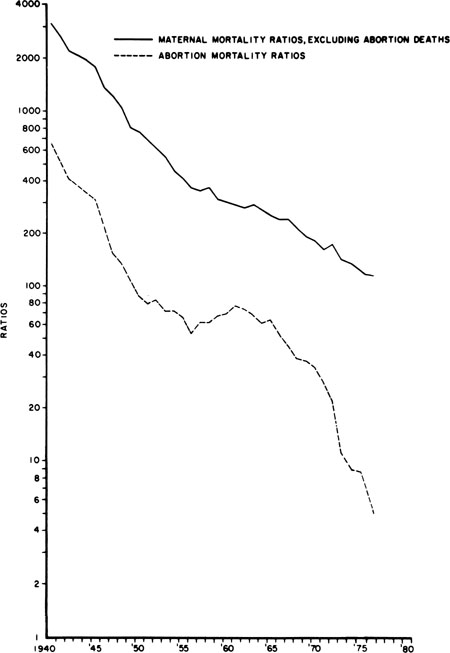
U.S. maternal deaths from all causes have declined rapidly since 1940.9 Nonabortion maternal mortality declined steadily. Abortion mortality exhibited three phases: an initial decline until 1950, a plateau from 1951 to 1965, and then a very rapid decline from 1965 to 1976 (more rapid than that of maternal mortality from other causes) as legal abortion became increasingly available (Fig. 1). In 1992, the last year for which complete data are available, 10 deaths were reported of 1,359,145 legal induced abortions, for a case-fatality rate of 0.7 per 100,000 legal abortions.6 By comparison, in the 1940s, over 1000 women per year were known to have died from abortion in the United States.5 The American Medical Association’s Council on Scientific Affairs has attributed the marked decline in abortion deaths in this century to the introduction of antibiotics to treat sepsis, the widespread use of effective contraception beginning in the 1960s, which reduced the numbers of unwanted pregnancies, and more recently, the shift from illegal to legal abortion.10
Serious complications have become rare as well. A large series from Planned Parenthood of New York City describes 170,000 abortions performed in outpatient settings by a small group of expert practitioners.11 No deaths occurred, and only 121 hospitalizations for complications occurred, 0.71 per 1000 abortions. Approximately 3.5 million unwanted pregnancies occur each year in our country,12 and with the continuing attack on legal abortion services13 and current barriers to access,14 the demand for abortion may lead to a resurgence in illegal abortion.
Western Europe and the Former Soviet Union
The experience in Western Europe has been very similar to that in the United States, with legal abortion becoming widely available and very low rates of abortion mortality currently reported.15 Overall, maternal mortality from legal abortion in Europe is less than 1 per 100,000 procedures. Death rates are somewhat higher in the former Soviet Union, where the special problem of illegal abortion with a markedly higher risk of death has emerged.16
The Third World
Abortion remains a major cause of maternal death in Third World countries. The World Health Organization (WHO) estimates that 80,000 deaths from unsafe abortion occur in the world every year, about 13% of all maternal deaths.17 Most of these maternal deaths occur in underdeveloped countries. A WHO working paper summarizing the world literature after 1960 lists almost 400 published reports of abortion morbidity and mortality and concludes that “unsafe abortion is one of the greatest neglected problems of health care in developing countries.”18 The proportion of maternal deaths that result from unsafe abortion is probably considerably larger. Where abortion is illegal, women and health care professionals are reluctant to report that abortion was induced.19 Private personal dialogue with women by trained, empathetic caseworkers reveals a higher proportion of induced abortions.20
The preventable morbidity and mortality from septic abortion are staggering and well documented.21 A 1992 report of Guinea, in West Africa, reported an investigation of all maternal deaths in the capital from July 1, 1989, to June 30, 1990.22 The most common causes were hypertensive diseases (20%), postpartum bleeding (19%), and abortion (17%). Eighty percent of the abortion deaths were known to be from induced abortion. Sepsis was the most common cause of death. A study from five hospitals in Kampala, Uganda, in East Africa, for the period 1980 to 1986 found 20% of maternal deaths to be abortion-related.23 A Nigerian study reported that 35% of hospital maternal mortality was from abortion, with sepsis the most common cause of death.24 A 7-year review of abortion at the University College Hospital in Ibadan, Nigeria, reported that abortion complications represented 76.7% of all emergency gynecologic admissions.25 A population-based survey in rural Bangladesh identified 387 maternal deaths from 1976 to 1985 (555 per 100,000 live births).26 Principal causes of death were postpartum hemorrhage (20%), abortion (18%), and toxemia/eclampsia (12%).
In 1990, 36 hospitals and medical schools from four Latin American countries participated in a multinational study of all women attended for abortion during a 6-month period.27 During this time, 14,501 abortion admissions were recorded and 8871 were investigated. At the same time 113,714 births occurred in the participating hospitals. Fifteen percent of the abortions were classified as septic on admission. Forty-three women of the 8871 required hysterectomy, and 36 women died, producing an abortion maternal mortality rate of 406 per 100,000 women admitted for abortion. Although hemorrhage was the most common abortion complication, 75% of the deaths were in women admitted as “septic.” The problem may actually be escalating in some areas. A 10-year review from Rio de Janeiro found maternal mortality to have increased almost fourfold from 1978 to 1987 (128 per 100,000 to 462 per 100,000). Abortion-related deaths accounted for 47% of the total mortality.28 As shown in all of these studies, abortion deaths are primarily from sepsis.
More recent reports from many countries echo the same dismal findings. A report of a 10-year study from rural India, published in 2001, found that 41.9% of all maternal deaths were from septic abortion, and the total maternal mortality rate was extraordinary (785 per 100,000 live births), approximately 100-fold greater than maternal mortality in developed countries.29