This chapter should be cited as follows:
Oikonomou M, Chandraharan E, Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.415143
The Continuous Textbook of Women’s Medicine Series – Obstetrics Module
Volume 11
Labor and delivery
Volume Editor: Dr Edwin Chandraharan, Director Global Academy of Medical Education and Training, London, UK
Chapter
Management of Second Stage of Labor
First published: February 2021
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
The second stage of labor refers to the period that elapses between the onset of full dilatation of the cervix and delivery of the fetus. It is further divided into a 'passive' phase which involves progressive descent and rotation of the presenting part, and an 'active' phase of maternal expulsive efforts.
The second stage of labor, while typically well-tolerated in uncomplicated deliveries, represents a critical period during which complications, if they arise, can contribute to increased maternal and perinatal morbidity and mortality. These risks are primarily related to the potential for the rapid onset of fetal hypoxic stress and maternal perineal trauma, both of which result from the mechanical forces exerted as the bony fetal head traverses the maternal soft tissues of the birth canal.
This chapter addresses the anatomy of the female pelvis, mechanism of labor, fetal monitoring specific to the second stage of labor, the conduct of operative vaginal birth and measures to avoid complications.
MATERNAL BIRTH PASSAGE AND MECHANISM OF LABOR
The maternal birth passage consists of a bony pelvis comprising the ilium, ischium and pubis, articulating with the sacrum and coccyx posteriorly, as well as soft tissues. The latter are composed of ligaments, muscles of the pelvic floor and of the pelvic sidewall, and muscles of the perineum covered by skin and subcutaneous tissue. It is important to appreciate that the pelvis is richly supplied by a network of blood vessels with significant anastomoses, as well as nerve fibers and nerve plexuses.
Unlike four-legged mammals, the human pelvis has undergone significant evolutionary changes relating to an erect posture. The female bony birth canal is no longer cylindrical, but has a narrower anteroposterior diameter at the level of the pelvic inlet due to the projection of the sacral promontory, to aid weight-bearing. In contrast, due to the projection of the large ischial tuberosities, as a result of the need to provide attachments to the powerful muscles of thigh which were essential for running and hunting, the pelvic outlet has developed a smaller transverse diameter (Figure 1).
.jpg?1636643)
1
Model of female human pelvis. Note the larger transverse diameter at the inlet (black arrow) as compared to the outlet (blue arrow).
The evolutionary changes in the diameters of the human pelvis have had a direct impact on the fetus during the second stage of labor. After having entered the maternal bony pelvis in either an oblique or transverse diameter, in view of the narrow anteroposterior diameter at the pelvic inlet, the human fetus has to undergo an internal rotation in the larger mid cavity of the maternal pelvis. This is to ensure that the fetal skull position changes from the transverse or oblique diameter to an anteroposterior diameter, to overcome the restricted space due to the large, laterally placed ischial tuberosities at the pelvic outlet (Figure 1). In addition, the fetus needs to traverse the J-shaped maternal birth passage, called the 'curve of Carus'.
The mechanisms adopted by the human fetus during second stage of labor (Table 1) are determined by the effectiveness of the uterine contractions (power), the size, position and presentation of the fetus (passenger) and the resistance offered by the bony and soft tissue parts of the maternal birth passage (passage).
The aim of optimizing the management of the second stage of labor is to understand and correct the relationship between the power, passenger and passage, so that maternal and perinatal morbidity and mortality can be avoided. It is important to appreciate that an emergency cesarean section during the second stage of labor is associated with significantly increased maternal and perinatal morbidity and mortality. Therefore, every attempt should be made to achieve a vaginal birth, provided it is safe to do so, after performing a thorough maternal and fetal assessment, and considering the overall clinical picture. Women should be appropriately supported throughout the second stage of labor, and should be provided with sufficient, evidence-based information to make informed decisions about their care.
1
Mechanisms of human labor during the second stage.
Mechanism | Definition |
Engagement | The widest diameter of the presenting part (i.e. the fetal biparietal diameter in vertex presentation and bitrochanteric diameter in a breech presentation) crosses the maternal pelvic brim |
Descent | Downward movement of the leading bony edge of the presenting part inside the maternal birth passage |
Flexion | Maximum movement of the fetal chin towards the fetal chest wall when the sinciput presses against the firm pelvic floor muscles due to ongoing uterine contractions, leading to the flexion of the fetal neck |
Internal rotation | Rotation of the fetal occiput (in a cephalic presentation) due to the wriggling contractions of the levator ani muscles (i.e. muscles of the pelvic floor) from a transverse or oblique diameter to an anteroposterior diameter |
Extension | Upward movement of the sinciput as the fetal head emerges from the resistance offered by the symphysis pubis |
Restitution | 'Restoration of anatomy' as the fetus attempts to correct twisting of the neck during internal rotation |
External rotation | Rotation of the occiput outside the mother’s birth passage, as the fetal shoulders undergo internal rotation |
Delivery of the shoulders and trunk | Once the delivery of the fetal head has occurred, and following the internal rotation of the shoulders, the second stage of labor is complete when the fetal shoulders, trunk, buttocks and legs are delivered |
Power
Uterine contractions have three properties: frequency, duration and strength, and optimum uterine contractions are essential to ensure descent, flexion, rotation of the presenting part and, ultimately, the delivery of the fetus. Sufficient time should be allowed between uterine contractions during the second stage of labor to enable the fetus to obtain fresh oxygen from the placenta and to excrete the carbon dioxide and metabolic by-products into the maternal circulation.
In the presence of perceived ineffective uterine activity, it is important to exclude mechanical causes of poor progress of labor during the second stage. These include bony and soft-tissue abnormalities of the maternal pelvis (for example, previous pelvic fractures, scarring within the birth passage due to previous soft tissue injuries) as well as relative cephalopelvic disproportion (CPD). Oxytocin should not be commenced during the second stage of labor in the presence of relative or absolute CPD. Injudicious use of oxytocin has been shown to be associated with hypoxic ischemic injury. In a multiparous woman, or in a woman with a uterine scar, injudicious use of oxytocin during second stage of labor may significantly increase the risk of uterine rupture. The uterine myometrium is maximally sensitive to oxytocin with increased oxytocin receptors during the second stage of labor.1,2,3 Therefore, oxytocin should be commenced only after excluding maternal bony abnormalities and relative CPD, beginning at the lowest dose. The second stage of labor should be carefully monitored after commencing oxytocin to determine the progress of labor as well as fetal wellbeing, in order to avoid serious maternal and fetal complications. If there is any evidence of uterine hyperstimulation or abnormal features on the cardiotocograph (CTG) trace, oxytocin infusion should be stopped immediately.
Passenger
The main problems involving the passenger during the second stage of labor include relative CPD, abnormal position or deflexion of the presenting part, which increases the diameters of the fetal skull, and abnormalities in fetal heart rate (FHR). Undiagnosed malpresentation (i.e. breech or brow presentation) may be associated with poor progress during second stage of labor.
If relative or absolute CPD has been excluded, ineffective uterine contractions may be managed with the judicious use of oxytocin infusion, accompanied by careful maternal and fetal monitoring, to promote fetal head flexion and facilitate rotation of the occiput, thereby correcting any malposition. However, if uterine contractions are deemed effective, operative vaginal delivery (vacuum or forceps) should be considered to address persistent deflexion and malrotation in order to achieve a vaginal birth.
Specially designed forceps, such as the Piper’s forceps (Figure 2), may be used to accomplish the delivery of the ‘after-coming' head during assisted vaginal breech birth. In the context of twin pregnancy, internal podalic version (IPV) can be performed by an experienced operator to correct the transverse lie of the second twin after the vaginal birth of the first twin.

2
Specially designed Piper’s forceps with long and curved shanks facilitate application to the ‘after-coming’ head in breech delivery.
Passage
Bony abnormalities of the pelvic inlet often result in non-engagement of the fetal head, typically accompanied by significant caput and molding during labor. These abnormalities should be recognized during the first stage of labor, as they may lead to failure of descent and cervical dilatation, necessitating an emergency cesarean section due to lack of progress. Bony abnormalities in the mid-cavity (i.e. prominent ischial spines) are rare, and, if present, would result in failure of internal rotation leading to fetal malposition.
If there is evidence of a bony abnormality in the pelvic outlet, such as a narrow subpubic arch (Figure 3), an operative vaginal birth should be avoided to prevent serious maternal perineal trauma and fetal injury. Careful and thorough clinical pelvimetry should be carried out to exclude bony abnormalities in the pelvic inlet, mid-cavity and the pelvic outlet prior to attempting any operative vaginal birth.
Soft tissue abnormalities at the pelvic outlet can be corrected by performing a generous episiotomy to overcome the resistance offered by taut perineal muscles.

3
Model of female human pelvis. Note bony pelvic outlet obstruction due to a narrow subpubic arch.
ASSESSING FETAL WELLBEING DURING SECOND STAGE OF LABOR
A fetus is exposed to maximum hypoxic stress during the second stage of labor, due to a combination of maternal expulsive efforts and their impact on the uteroplacental circulation, as well as repetitive and sustained compression of the umbilical cord and the fetal head.4 Table 2 illustrates the detrimental effects of active potential pushing on fetal wellbeing. Studies have shown that there is a significant increase in fetal lactate levels with prolonged active maternal pushing.5,6
2
Detrimental effects of active maternal pushing.4
Action | Impact |
Valsalva maneuver to aid expulsive efforts | Reduced venous return due to increased intrathoracic pressure resulting in reduced stroke volume and maternal cardiac output leading to a reduction in uteroplacental circulation |
Reduced maternal breathing during episodes of active maternal pushing | Reduced maternal oxygen saturation leading to reduced oxygenation of the fetus |
Impaction of the fetal head deep inside the maternal birth passage | Increased fetal intracranial pressure resulting in reduced circulation through the carotid arteries, potentially reducing cerebral circulation |
Lateral pressure of the fetal head on the uterine vessels | Reduced uteroplacental blood flow |
Increased intrauterine pressure due to a combination of strong uterine contractions and increased intra-abdominal pressure secondary to active maternal pushing | Repetitive and sustained compression of the umbilical cord resulting in a reduction in fetal oxygenation |
Intermittent auscultation
If intermittent auscultation is used during low-risk labor, the FHR should be auscultated at least once every 5 minutes, immediately after a uterine contraction, to detect a slow recovery of the FHR suggestive of chemoreceptor-mediated late decelerations. If any abnormality is detected, the frequency of auscultation should be increased, and the FHR should be assessed again during the next contraction rather than waiting for the next scheduled interval. If the observed abnormalities persist, arrangements should be made immediately for the commencement of continuous electronic FHR monitoring using CTG, unless an immediate vaginal birth is imminent. It is important to bear in mind that accelerations of the FHR immediately after a uterine contraction, when the fetal oxygen saturation is at its lowest level, are unlikely. Therefore, if accelerations are heard during intermittent auscultation, the FHR should be auscultated throughout the following uterine contractions to detect the presence of an atypical variable deceleration, immediately followed by an exaggerated fetal reflex response to increase the baseline heart rate ('overshoots'). This is because these overshoots represent the attempts by the fetus to normalize his/her blood pressure in view of ongoing fetal hypotension as a result of repetitive and sustained umbilical cord compression. The presence of overshoots may indicate ongoing excessive uterine activity, unrecognized oligohydramnios and/or thick meconium-stained amniotic fluid, all of which can predispose to sustained umbilical cord compression.
Therefore, if any abnormalities are detected during intermittent auscultation, such as decelerations with late recovery, repetitive accelerations or a rise in the baseline FHR compared to the previously observed baseline, particularly immediately after a uterine contraction and suggestive of a fetal catecholamine response, urgent action should be taken to prevent hypoxic-ischemic encephalopathy (HIE) and/or perinatal death.
If a vaginal birth is not imminent, the woman should be transferred immediately to an obstetric unit for the commencement of CTG monitoring and/or for expediting birth based on the abnormalities observed on the CTG trace.
Cardiotocography
In view of the detrimental effects of active maternal pushing highlighted in Table 2, it should be obvious to clinicians that standard 'CTG guidelines' used in labor wards are unlikely to be effective during the second stage of labor when fetal hypoxic stress evolves very rapidly. This is because a fetus would simply have insufficient time to mount a successful compensatory response to the rapidly evolving hypoxia after the commencement of active maternal pushing. It is important to recognize and diagnose the subacute hypoxic pattern during active second stage of labor.7 The time spent at the baseline (usually <30 seconds) is insufficient to dispose of the carbon dioxide and metabolic by-products accumulated during the 'deep and wide' decelerations (duration of more than 90 seconds), and to obtain sufficient oxygen from the placenta. It has been shown that due to this rapidly evolving hypoxia, the fetal pH drops at the rate of 0.01 units once in every 2–3 minutes during such a subacute hypoxic pattern (Figure 4) observed on the CTG trace.8
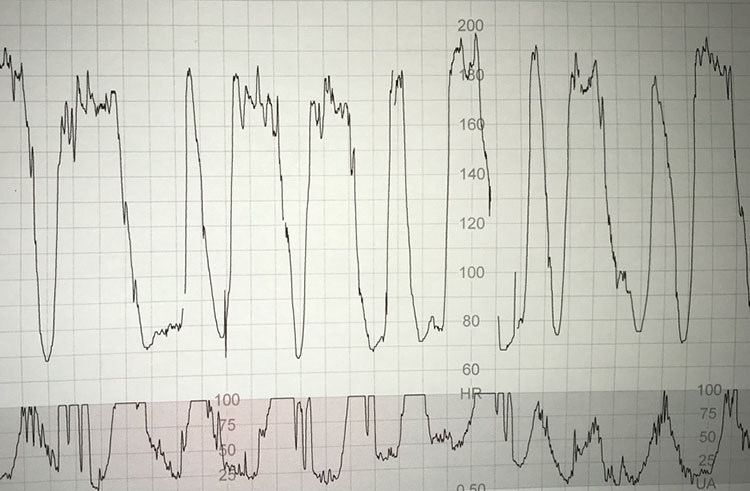
4
Subacute hypoxic pattern in which a fetus spends progressively less time at the baseline (<30 seconds) as compared to the time spent during the deceleration (>90 seconds).
Recently, it has been shown that during active maternal pushing, a rapidly evolving hypoxic process may be associated with a ‘zigzag’ pattern on the CTG trace, reflecting autonomic instability.9 The zigzag pattern (Figure 5) has been reported to be associated with poor perinatal outcomes and an increased risk of neonatal unit admission.⁹ Therefore, it is important to actively monitor for both subacute hypoxic patterns and the zigzag pattern on the CTG trace during the second stage of labor, beginning at the onset of active maternal pushing.
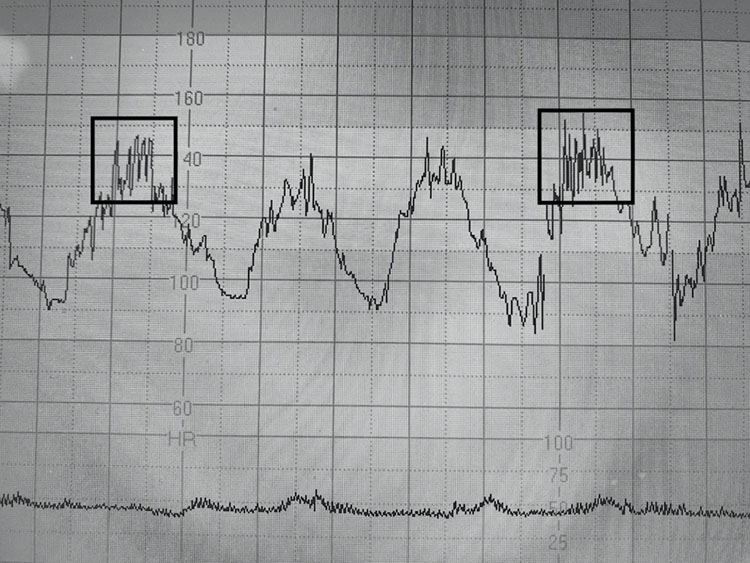
5
CTG trace shows ongoing subacute hypoxia with the 'zigzag' pattern in between the 'deep and wide' decelerations, during active maternal pushing.
Repetitive accelerations coinciding with uterine contractions on the CTG trace should always be considered as abnormal and unphysiological during the second stage of labor. Often, they are due to the erroneous recording of the maternal heart rate (which shows accelerations during contractions due to pain, anxiety and increased venous return) on the CTG trace. If such repetitive accelerations are observed during uterine contractions, then, the maternal pulse should be checked immediately in order to avoid poor perinatal outcomes secondary to missing ongoing abnormalities of FHR. A fetal scalp electrode (FSE) should be considered to optimize the signal quality, if appropriate.
RECOGNIZING FETAL COMPROMISE DURING SECOND STAGE OF LABOR
The vast majority of fetuses will be able to mount a successful compensatory response to the rapidly evolving hypoxia during the second stage of labor to avoid hypoxic-ischemic brain injury. However, depending on the individual fetal reserve, the intensity and rapidity of the hypoxic stress (i.e. induced or augmented labor), as well as the wider clinical picture (e.g. presence of meconium staining of amniotic fluid, maternal pyrexia or chorioamnionitis) some fetuses may be predisposed to intrapartum hypoxic injury during the second stage of labor.
In addition to the subacute hypoxic stress with a fetal catecholamine response (abrupt increase in the FHR compared to the original baseline) in between the decelerations and the zigzag pattern, clinicians should be aware of the progressive reduction in the baseline heart rate. This is because the end stage of ‘gradually evolving’ hypoxic stress is a progressive reduction in the baseline heart rate (the 'step ladder pattern to death') secondary to progressive myocardial lactic acidosis. In such cases, the catecholamine-induced increase in the baseline FHR will be followed by a reduction in baseline FHR variability suggestive of the onset of fetal metabolic acidosis.10
The presence of meconium in the amniotic fluid may be secondary to physiological maturation of the fetal gut.11 However, it must be appreciated that irrespective of its classification as significant or non-significant, meconium has both systemic and local effects on the fetus.12 Therefore, rapidly evolving hypoxic stress indicated by ongoing subacute hypoxic pattern or the zigzag pattern on the CTG may predispose to meconium aspiration syndrome. Maternal pyrexia increases maternal and fetal metabolic rates, and resultant increased oxygen consumption of tissues and organs. Therefore, if rapidly evolving intrapartum hypoxic stress during the second stage of labor is superimposed on maternal pyrexia, it can accelerate the onset of hypoxic injury. Recently, it has been shown that, in chorioamnionitis, loss of FHR cycling, absence of accelerations, the zigzag pattern and sinusoidal pattern are common.13 Therefore, these features should be actively scrutinized on the CTG trace during the second stage of labor.
OPERATIVE VAGINAL BIRTH
An operative vaginal birth (vacuum or forceps delivery) may become necessary for maternal (exhaustion, cardiorespiratory disorders or brain aneurysms which preclude active maternal pushing) or fetal (suspected or confirmed fetal compromise or malposition position) indications. It is important to understand the pelvic anatomy, the mechanisms of human labor and the anatomy of the fetal skull, including the important landmarks, prior to embarking on an operative vaginal birth. It is equally important to achieve competency and confidence prior to performing this procedure independently to avoid risks and complications as well as medicolegal pitfalls. The most important variables that ensure a successful vaginal birth with good maternal and perinatal outcomes are the knowledge, skills and competency of the operator. Chandraharan and Arulkumaran proposed the 'FORCEPS' checklist (Table 3) to ensure that all criteria are fulfilled prior to embarking on operative vaginal birth.
It is vital to remember that the primary aim of obstetric practice is to ensure a healthy, uninjured mother and baby at the end of pregnancy and childbirth. Therefore, operative vaginal birth should not be pursued at all costs, especially when it may lead to maternal or fetal trauma. Similarly, emergency cesarean section in the late second stage of labor is associated with significant maternal and perinatal morbidity and mortality due to the risks involved in dislodging a deeply engaged fetal head.15 According to the Early Notification Scheme Report published by NHS Resolution in 2019, failed instrumental deliveries and difficult delivery of the fetal head during cesarean section contributed to 11.5% and 18.4% of poor neonatal outcomes, respectively.16 This underscores the importance of ensuring that operative vaginal births are performed safely and competently, with attention to technical precision, to minimize maternal and fetal complications.
3
Modified 'FORCEPS' checklist for conducting operative vaginal birth.14
Before any operative vaginal birth, ensure that the indication is appropriate, the woman and the multidisciplinary team are fully informed, and an experienced and competent clinician is available to undertake or to directly supervise the procedure | |
F | Confirm that the cervix is Fully dilated |
O | Exclude any mechanical Obstruction (<1/5 of the fetal head palpable per abdomen) |
R | Membranes should be Ruptured; think 'Risk Management' |
C | Obtain informed Consent, and Catheterize the Bladder, check CTG |
E | Ensure Epidural (or pudendal) analgesia, choose the right Environment (operative theater vs delivery room), Exclude genital tract trauma |
P | Determine the Position, optimize the Power (effective uterine contractions), Pause (if there is no progress with traction) |
S | Determine the Station, ensure Situational Awareness & Scribe (clear documentation) |
Excessive traction and inappropriate force should be avoided whilst conducting both vacuum and forceps births. Clinicians should apply appropriate traction in the correct direction i.e., along the curve of Carus. When using forceps, performing Pajot’s maneuver to ensure traction at a 45° angle along the curve of Carus is essential. The vacuum cup should be placed correctly at the flexion point, which is an arbitrary area approximately 3 cm anterior to the posterior fontanelle along the sagittal suture (Figure 6). Failure to correctly place the center of the vacuum cup on the flexion point may result in serious maternal and fetal complications due to a combination of the increased diameters of the deflexed fetal head and the resultant inappropriate and excessive traction.
Malapplication of the vacuum cup can increase the likelihood of a failed operative vaginal delivery leading to an unnecessary emergency cesarean section during the second stage of labor.

6
Model of fetal skull showing flexion point, which is approximately 3 cm anterior to the posterior fontanelle along the sagittal suture.
Rotational forceps (Kielland’s) and vacuum deliveries should be performed by a skilled operator to avoid maternal and fetal trauma. In skilled hands, a rotational operative vaginal delivery during second stage of labor causes fewer complications as compared to an emergency cesarean section for a deeply engaged fetal head. Vacuum and forceps deliveries should be considered complementary rather than mutually exclusive techniques. Since vacuum delivery is not suitable in all cases, for example, in the presence of gross caput, preterm delivery or fetal bleeding disorders, every practising obstetrician has a duty of care to be competent in both vacuum and rotational forceps deliveries to ensure optimal outcomes for women and their babies during the second stage of labor.
DURATION OF SECOND STAGE OF LABOR
In view of the reported increase in fetal lactate levels after the onset of active maternal pushing,5,6 continued active pushing for more than 60 minutes should be avoided, unless a spontaneous vaginal birth is imminent and the CTG trace shows no evidence of ongoing fetal compromise.
There are differing schools of thought regarding the duration of the passive second stage of labor. Most obstetricians allow up to 2 hours of passive second stage in women with epidural analgesia. This is due to the potential interference with internal rotation caused by epidural-induced reduction in pelvic floor muscle tone. However, it should be remembered that prolonged pressure of the fetal head on the maternal pelvic floor and soft tissues may increase the risk of uterovaginal prolapse and urinary incontinence later in life. Therefore, care should be individualized, and a vaginal examination is recommended after 1 hour of passive second stage, even in women with an epidural.
If the fetal vertex is at or below the ischial spines and in an occipitoanterior position, active maternal pushing should be commenced after 1 hour. In cases of malposition, or if the fetal vertex is above the ischial spines, it is reasonable to allow more time to facilitate descent and internal rotation before initiating active pushing.
REDUCING RISKS DURING SECOND STAGE OF LABOR
Due to rapidly evolving fetal hypoxia and the need for clinicians to make quick decisions in a highly charged and dynamic environment, it is unsurprising that the second stage of labor is associated with a significant number of malpractice claims.17 A 5-year study conducted at a tertiary institution reported that the implementation of intensive, hands-on training in operative vaginal birth techniques led to a significant reduction in the incidence of failed operative vaginal births.18
Therefore, continuous and structured training in operative vaginal birth for obstetricians of all grades is essential. Equally important is the routine monitoring of outcomes using clinical governance tools such as the 'maternity dashboard'19 to help reduce adverse incidents and litigation during the second stage of labor.
Targeted training on the interpretation of CTG during the second stage of labor should also be mandatory for all midwives and obstetricians. This training should include recognition of erroneous maternal heart rate recordings,20 as well as an understanding of CTG features typically observed during operative vaginal birth, to optimize perinatal outcomes.21
PRACTICE RECOMMENDATIONS
- The second stage of labor represents the period of highest risk for both the mother and fetus, due to the rapid progression of fetal hypoxic stress and the mechanical effects of the descending fetal head on the maternal soft tissues.
- The effectiveness of the ‘power’, the roominess of the 'passage' and the wellbeing and the size, position and attitude of the 'passenger' should all be considered when making management decisions.
- Standard CTG guidelines are unlikely to be useful in the presence of rapidly evolving fetal hypoxic stress. Recognition of subacute hypoxia and the 'zigzag' pattern is essential.
- Accelerations detected during intermittent auscultation in the second stage of labor, particularly those coinciding with uterine contractions, are uncommon and may not reflect a physiological pattern.
- The 'FORCEPS' checklist is recommended to avoid errors during operative vaginal births that may result in maternal and perinatal complications.
- Risk management should include intensive hands-on training in performing operative vaginal births, and continuous monitoring of outcomes by using the 'maternity dashboard'.
CONFLICTS OF INTEREST
The author(s) of this chapter declare that they have no interests that conflict with the contents of the chapter.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Uvnäs-Moberg K, Ekström-Bergström A, Berg M. et al. Maternal plasma levels of oxytocin during physiological childbirth – a systematic review with implications for uterine contractions and central actions of oxytocin. BMC Pregnancy Childbirth 2019;19:285. https://doi.org/10.1186/s12884-019-2365-9. | |
Wathes DC, Borwick SC, Timmons PM, et al. Oxytocin receptor expression in human term and preterm gestational tissues prior to and following the onset of labour. J Endocrinol 1999;161(1):143–51. | |
Bukhari H, Chandraharan E. Physiopharmacology of Labour. In: Arulkumaran S, Arjun G, Penna LK. (eds.) The Management of Labour, 3rd edn. University Press, 2011. | |
McDonnell S, Chandraharan E. Fetal heart rate interpretation in the second stage of labour: pearls and pitfalls. British Journal of Medicine and Medical Research 2015;7:957–70. | |
Nordström L, Malcus P, Chua S, et al. Lactate and acid-base balance at delivery in relation to cardiotocography and T/QRS ratios in the second stage of labour. Eur J Obstet Gynecol Reprod Biol 1998;76(2):157–60. | |
Nordström L, Achanna S, Naka K, et al. Fetal and maternal lactate increase during active second stage of labour. BJOG 2001;108(3):263–8. | |
Chandraharan E, Arulkumaran S. Prevention of birth asphyxia: responding appropriately to cardiotocograph (CTG) traces. Best Pract Res Clin Obstet Gynaecol 2007;21(4):609–24. | |
Pinas A, Chandraharan E. Continuous cardiotocography during labour: Analysis, classification and management. Best Pract Res Clin Obstet Gynaecol 2016;30:33–47. | |
Gracia-Perez-Bonfils A, Vigneswaran K, Cuadras D, et al. Does the saltatory pattern on cardiotocograph (CTG) trace really exist? The ZigZag pattern as an alternative definition and its correlation with perinatal outcomes. J Matern Fetal Neonatal Med 2019:1–9. | |
Jia YJ, Chen X, Cui HY, et al. Physiological CTG interpretation: the significance of baseline fetal heart rate changes after the onset of decelerations and associated perinatal outcomes [published online ahead of print, 2019 Sep 18]. J Matern Fetal Neonatal Med 2019;1. doi: 10.1080/14767058.2019.1666819. Format: | |
Mitchell S, Chandraharan E. Meconium-stained amniotic fluid, Obstetrics, Gynaecology and Reproductive Medicine, 2018. https://doi.org/10.1016/j.ogrm.2018.02.004. | |
Bolten M, Chandraharan E. The Significance of ‘Non-Significant’ Meconium Stained Amniotic Fluid (MSAF): Colour versus Contents. Journal of Advances in Medicine and Medical Research 2019;30(5):1–7. | |
Galli L, Whelehan V, Archer A, et al. Perinatal outcomes in fetuses with cardiotocography (CTG) changes suggestive for chorioamnionitis. European Journal of Obstetrics and Gynecology and Reproductive Biology 2019:234:e4. | |
Chandraharan E, Arulkumaran S. Operative delivery, shoulder dystocia and episiotomy. In: Arulkumarn S, Penna LK, Bhaskar Rao K. (eds.) The Management of Labour, 2nd edn. Orient Longman, 2005. | |
Manning JB, Tolcher MC, Chandraharan E, et al. Delivery of an Impacted Fetal Head During Cesarean: A Literature Review and Proposed Management Algorithm. Obstet Gynecol Surv 2015;70(11):719–24. https://resolution.nhs.uk/wp-content/uploads/2019/09/NHS-Resolution-Early-Notification-report.pdf. | |
NHS Resolution. The Early Notification scheme progress report: collaboration and improved experience for families. September 2019 https://resolution.nhs.uk/wp-content/uploads/2019/09/NHS-Resolution-Early-Notification-report.pdf. | |
Chandraharan E, Arulkumaran S. Medico-legal Problems in Obstetrics. Obstetrics, Gynaecology and Reproductive Medicine 2006;16(4):206–10. | |
McDonnell S, Chandraharan E. Determinants and Outcomes of Emergency Caesarean Section following Failed Instrumental Delivery: 5-Year Observational Review at a Tertiary Referral Centre in London. J Pregnancy 2015;2015:627810. | |
Chandraharan E, Arulkumaran S. The role of clinical dashboards in improving patient care: experience with the 'Maternity Dashboard'. Ceylon Med J 2016;61(2):83–5. doi: 10.4038/cmj.v61i2.8291. | |
Nurani R, Chandraharan E, Lowe V, et al. Misidentification of maternal heart rate as fetal on cardiotocography during the second stage of labor: the role of the fetal electrocardiograph. Acta Obstet Gynecol Scand 2012;91(12):1428–32. | |
Xie W, Archer A, Li C, et al. Fetal heart rate changes observed on the CTG trace during instrumental vaginal delivery. J Matern Fetal Neonatal Med 2019;32(1):117–24. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards program CLICK HERE)

