This chapter should be cited as follows:
Cárcamo W, Fescina R, et al., Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.416463
The Continuous Textbook of Women’s Medicine Series – Obstetrics Module
Volume 12
Operative obstetrics
Volume Editor: Professor Owen Montgomery, Thomas Jefferson University, Philadelphia, USA
Chapter
Special Considerations Related to Cesarean Delivery in Low- and Middle-Income Countries
First published: February 2022
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
The aim of cesarean delivery is to offer an alternative route to birth preventing damage and preserving the life of mother and child. This initially saving intervention has in recent years become a public health challenge due to the large increase in its incidence in many cases without justification.
The advancement of anesthetic, surgical and antibiotic techniques has greatly reduced morbidity and mortality, resulting in liberalization of cesarean delivery in recent decades reaching more than 50% in some countries. However, in poorer countries such as in sub-Saharan Africa, the frequency of cesarean delivery is below what is scientifically indicated, paradoxically not meeting the population needs where higher rate of pathologies such as obstructed labor require cesarean delivery.
At the end of the 20th century, the World Health Organization (WHO) based on an expert opinion meeting, recommended that the population prevalence of cesarean delivery should be equal to or less than 15% of all births. However, it has recently been observed that countries with cesarean section rates of 19% have the lowest maternal and perinatal mortality rates and by exceeding this limit no benefit was observed in terms of maternal and neonatal mortality. In contrast, in countries with rates below 10%, maternal and neonatal mortality increased.1,2
Unfortunately, cesarean delivery without any medical indication has increased to unacceptable numbers, leading to an increased risk of maternal morbidity such as uterine rupture, placental accretism, infection, and increased risk of mortality compared to vaginal delivery. In addition, cesarean delivery results in an increased risk for neonatal complications, including a greater number of resuscitation maneuvers, more respiratory complications, and delayed early breastfeeding.3
Not only has maternal and neonatal morbidity increased but cesarean delivery results in increased health costs due to greater days of hospitalization and increased rate of hospital readmissions.
The above concerns translate into a significant worldwide public health problem, for countries with over utilization of cesarean delivery (above the 19% rate), and for countries with underutilization of cesarean delivery (rates around 5%) due to lack of access to appropriate health services with qualified personnel.
Consequently, the approach to solutions for decreasing or increasing cesarean delivery rates should be done according to a detailed analysis of the population studied, with the understanding that the approach should be tailored to each country or groups of countries with similar epidemiological situations, access to health services and availability of trained professionals.
EPIDEMIOLOGY OF CESAREAN DELIVERY
Birth rates vary from country to country and the route of birth is greatly influenced by cultural traditions and access to health care.4,5,6,7,8 Over the past 50 years, due to significant improvement in health care systems, an increasing number of newborns have been given birth to in medically controlled settings, such as hospitals and small clinics. While these factors have contributed to a reduction in perinatal morbidity and mortality rates worldwide, some reports indicate that they have also led to unjustified overuse of procedures such as cesarean section,9 and consequently increased health care costs.10,11
Cesarean delivery constitutes a life-saving surgery for women and babies when complications occur such as labor hemorrhage, fetal distress, abnormal fetal presentation, hypertensive disease among others, and has become the most common surgical intervention in many countries. In recent years, the ideal cesarean delivery rate has been significantly debated due to the overall focus on quality of care, patient safety, the increasing numbers, and significant variations between countries, showing marked disparities: 2% in Chad, Burkina Faso, Ethiopia or Madagascar, 5% in Sub-Saharan Africa and above 50% in Southeastern Europe, China, Brazil, Egypt and the Dominican Republic.12,13
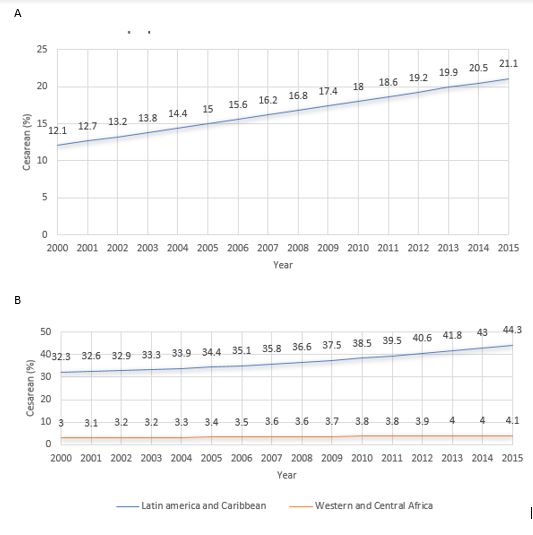
In 2015 worldwide, 29.7 million (21.1%, confidence interval 95% 19.9–22.4%) of a 140.6 million live births were born by cesarean delivery, an increase of 16.0 million compared to 2000 (Figure 1A).
Boerma and contributors14 in its 2018 publication, reported that the global annual average increase in cesarean delivery was 3.7% between 2000 to 2015. For this period, the rate of cesarean delivery varied greatly between the nine regions of the world: 4.1% (3.6–4.6%) in West and Central Africa, and 44.3% (41.3–47.4%) in the Americas and Caribbean region, this being the highest rate region (Figure 1B).
1
Estimated frequency and trends in cesarean section use, as a proportion of live births between 2000 and 2015. (A) Global data; (B) regional data. Modified from Boerma et al., 2018.14
Increases in the rate of cesarean delivery were observed in all world regions occurring more rapidly in Eastern Europe, Central Asia, South Asia, East Asia, Pacific regions (median annual change of 5.5%) compared to East, South Africa, West and Central Africa (2.1%).
Although cesarean rates above 20% appear to do more harm than benefit, rates of up to more than 50% have been reported.2,15,16
In 1985 the WHO first recommended a cesarean delivery rate of 10–15% and experts based on the evidence available at the time concluded "there is no justification for any region to have a cesarean section rate of more than 10–15%."1,17,18,19 In 2015, Molina et al. found that the lower rates of maternal and neonatal mortality occur with cesarean delivery rates around 19%, suggesting that the rate previously set by WHO is likely to be very low and proposing a new ideal cesarean delivery rate.2
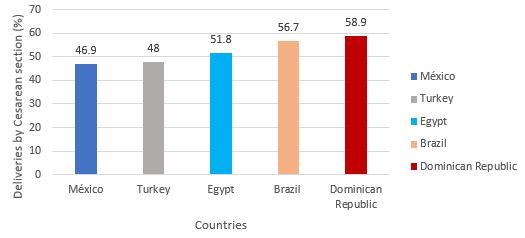
In the struggle for better quality and safety in health care, the cesarean delivery rate has been selected as one of the indicators for monitoring quality of care.20,21 Low-income countries (LICs) – especially in sub-Saharan Africa, have historically had very low cesarean delivery rates, probably reflecting inadequate availability, while high-income countries (HICs) generally have higher cesarean delivery rates, indicating overuse. The highest rates worldwide are seen in middle-income countries (MICs): Mexico (46.9%), Turkey (48.0%), Egypt (51.8%), Brazil (56.7%) and Dominican Republic (58.9%) (Figure 2).22
2
Country-specific cesarean section rates in middle-income countries.22
MATERNAL AND PERINATAL REPERCUSSIONS
As with any other surgery, cesarean delivery is associated with short- and long-term risks that can last for many years after surgery and affect the health of the mother, and the newborn, as well as the outcome of future pregnancies. These risks are greatest in women with little access to comprehensive obstetric care.
Women delivering by cesarean section are three to six times at greater risk of maternal mortality and amniotic fluid embolism compared to vaginal delivery, regardless of underlying medical conditions, pregnancy-related comorbidities, procedure indications or the urgency or elective nature of the procedure.23,24
A population retrospective cohort study based on the Canadian perinatal surveillance system, found that the frequency of severe adverse outcomes, defined as death, severe bleeding requiring transfusion or hysterectomy, uterine rupture, anesthetic complications, cardiac arrest, shock, acute renal failure, assisted ventilation, amniotic fluid embolism or venous thromboembolism, severe postpartum infection, dehiscence, surgical wound hematoma or both, was three times higher in women with cesarean delivery compared to women with vaginal delivery (2.7 and 0.9%, respectively).24
In women undergoing emergency cesarean delivery, there is a higher maternal mortality rate and higher morbidity rates, particularly for cardiac arrest, uterine rupture, hysterectomy hemorrhage, transfusion-requiring bleeding and hypovolemic shock than those undergoing elective cesarean delivery.24
Compared to newborns born by vaginal delivery, newborns born by elective cesarean section around term (from 37 weeks’ gestation onwards) have an increased risk of respiratory morbidity and the risk increases with decreasing gestational age.
Babies born by elective scheduled cesarean delivery have a significantly higher risk of respiratory morbidity at any gestational age compared to those delivered after 39 weeks, which is why elective cesarean delivery before 39 weeks’ gestation is not justified.25
The risks of iatrogenic preterm birth between 37 and 38 weeks are greater than the theoretical benefits (as long as the medical or obstetric indication makes it possible to defer delivery), such as in cases of possible macrosomia without maternal diabetes or history of a non-recurrent maternal or fetal complication in a previous pregnancy. Delivery is recommended at 39 weeks, rather than performing a fetal pulmonary maturity test at 37 to 38 weeks to justify early delivery.
In the long term, babies delivered by cesarean section compared to those born vaginally are at an increased risk of developing allergic upper respiratory tract disorders such as allergic rhinitis, asthma (more common in girls), celiac disease, diabetes mellitus and gastroenteritis.26,27
Mothers delivering by cesarean section can experience late complications such as uterine isthmocele, a defect in the myometrial wall secondary to the cesarean delivery scar, which can manifest clinically by abnormal or post-menstrual bleeding, chronic pelvic pain, infertility or in cases of future pregnancies can result in abnormal placentation, scar dehiscence, uterine rupture, and ectopic pregnancy localized in the cesarean section scar, increasing the risk of maternal death and extreme maternal morbidity in future pregnancies.28,29
CESAREAN DELIVERY – CAUSES AND SOLUTIONS CONSIDERING THE SCENARIO
In general, there is an excess of cesarean deliveries in almost all countries in Europe and America, representing an indicator of poor obstetric quality requiring efforts and interventions to reduce it. In contrast, there are other countries such as Haiti and sub-Saharan Africa where the frequency of cesarean delivery is very low, less than 5%. This difference represents one of the many paradoxes seen in medicine. To further highlight the disparities, the countries with the lowest cesarean delivery rates are the ones with the highest concentrations of at-risk populations resulting in a greater number of obstetric complications that would require cesarean delivery.30
As stated before in settings where the prevalence of cesarean delivery far exceeds 20% interventions aimed at reducing the cesarean rate are necessary. However, in scenarios where the rate is less than 10%, efforts are necessary to allow the safe performance of cesarean delivery to avoid maternal and neonatal complications.
Settings with high prevalence
The causes for high rates of cesarean delivery are not always scientifically proven, but in many cases are due to behaviors in health care professionals as well as in requests from patients.
The classic maternal, fetal, uterine or combination of indications for cesarean delivery, have increased surprisingly in the last few decades. In general, uterine causes have changed little, while some fetal and maternal indications have more than tripled compared to years past.
Cesarean delivery for non-reassuring fetal status has increased more than three times in the last decades without any logical explanation, in particular when the cesarean delivery results in a baby born vigorous with normal Apgar scores. This speaks of an over-diagnosis of non-reassuring fetal status often due to misinterpretation of electronic fetal monitoring tracings or confusion in interpretation of auscultation of early, late and variable decelerations prompting quick intervention by cesarean.
Breech presentation has become an absolute indication for cesarean delivery since Hannah's work demonstrated less fetal-neonatal morbidity when delivered by cesarean at term gestation.31 By extrapolation it has become standard practice to deliver all breeches, including preterm, by cesarean resulting in an increase of cesarean delivery, because at lower gestational age the incidence of breech presentation can be as high as 30% compared to 3–4% at term.31,32 This practice has also been extended, without any evidence, to multiple pregnancies, regardless of whether the presentation of the first fetus is breech or cephalic.
Failed induction as an indication for cesarean delivery has increased greatly, and it can be the result of an elective indication for induction. A recent publication of a retrospective study in Uruguay noted an increase in inductions at term (39–40 weeks) with low Bishop scores and without specific indications for the induction, increasing the risk of cesarean delivery by three times in particular for nulliparous women.33 The indication for elective induction at term should be discussed understanding the risks and benefits. This is different than offering induction for postdate pregnancies in particular when reaching 42 weeks with strict monitoring of fetal-maternal well-being.
Contrasting the experience in South America, a collaborative randomized multicenter study in the United States of induction of labor in nulliparous low-risk women at 39 weeks, showed a reduction in cesarean delivery in the induced group compared to the group of women managed expectantly: 18.6% versus 22.2% (RR 0.84 confidence interval 95% 0.76–0.93). Both groups had similar neonatal results.34
This conflicting information may in part be due to the different socioeconomic conditions between countries, medical attitudes and population sampling. The Uruguayan study is retrospective, but it involves all deliveries in the country. The USA study is a randomized controlled clinical trial, which gives greater weight to the evidence.
In 2011, the Pan American Health Organization (PAHO) began monitoring the “Action Plan to Accelerate the Reduction of Maternal Mortality and Severe Maternal Morbidity'” and among the multiple indicators used was the reduction of cesarean delivery by 20% by 2017 in countries where its rate was equal to or greater than 20%. During the implementation of the plan, a stable or slightly increased cesarean delivery rate was observed. 18 countries reported their cesarean delivery rate, and a slight increase was observed.35
Two other indications that have greatly increased the rate of cesarean delivery are the fear of malpractice litigation and socioeconomic and demographic factors. With regard to the former, the concern is that by not performing a cesarean delivery, it can result in adverse neonatal neurological outcome. As early as 1995 the lack of association between cesarean delivery and reduction of neonatal neurological problems was demonstrated.36
Socioeconomic and demographic factors represent a variety of elements that lead to an increase in cesarean delivery. It has been shown for more than 20 years that there is a direct and significant correlation between the patient’s family income and the indication for cesarean delivery, i.e., higher income, greater chance for cesarean delivery,37 also seen between patients with private insurance versus those in public hospitals.
The almost universal use of cesarean delivery has been documented in women with a high economic status in private health facilities such as in Brazil.38 It is important to mention in this group of Brazilian patients, the mother's preference to have her birth by cesarean. While in terms of rights, it is indisputable the right of the mother to request a cesarean delivery; however, if after a discussion of benefits and risks of cesarean delivery the patient still opts for an elective cesarean when there is no medical indication, the medical record should clearly state maternal request as the indication for surgery, and not using other medical indications to justify the surgery. This is important if there is a strategy in reducing the rate of cesarean delivery by reducing the payment for elective cesarean delivery secondary to maternal request. This will require a significant education campaign of the public.
Other factors responsible for the increase in cesarean delivery include decreased parity, women getting pregnant at a later age and obesity. However, without a doubt the most important factor that explains more than 30% of all cesarean deliveries, is a history of prior cesarean section. For this reason, it is extremely important to establish the reason for the primary section because it will determine the obstetric future of the gestant.
A trial of labor should always be offer to a patient with a history of a low transverse incision, because the old saying that “once a cesarean always a cesarean” is no longer a valid concept in obstetrics. The risk of rupture with a trial of labor is very small (less than 1%) and the chances of a successful trial of labor is high in particular for non-recurrent obstetric indications.
As previously discussed, cesarean delivery significantly increases maternal and neonatal risks and seriously compromise the reproductive future of the mother, increasing the chances of developing greater maternal and neonatal morbidity.
In high prevalence settings the following measures should be considered in an attempt to reduce the rate of cesarean delivery: The development of standard protocols for indications for cesarean delivery and its implementation; training of professionals in the care of normal labor and ability to perform a trial of labor after cesarean delivery; promote interventions to reduce pain; avoid primary cesarean using new definitions of the stages of labor, not limiting the latent phase and defining the active phase once 6 cm of cervical dilation is reached; diagnosing a lack of progression in dilation requiring at least 4 h of observation. The use of the partogram to monitor the progress of labor can be very useful not only for monitoring results but for teaching how a labor should be monitored.
It is also necessary to improve the physical infrastructure of obstetric triage and delivery rooms to increase the privacy and comfort of mothers and ensure that it is accompanied during labor by someone of their choice, including the use of doulas (proven to be an effective intervention to reduce cesarean delivery RR 0.75, 95% CI 0.64 to 0.88).39 Antenatal classes with preparation for labor and delivery classes should be offered.
Financial incentives should be considered for professionals and institutions recommending and performing vaginal delivery. Considering that surveillance of normal labor could last several hours, on average 8–10 h depending on parity, compared to cesarean delivery that on average takes 1 h to perform. Payment for vaginal delivery should be higher, preventing cesarean delivery from being performed simply for convenience and higher pay. Similarly, institutions with lower cesarean delivery rates can be rewarded for good management.
Institutions should be strictly monitored by observing the rates of cesarean delivery and its indications as a quality and safety measure and compared to other institutions. This last point is of paramount importance and usually one that most institutions avoid.
Settings with low prevalence
In regions with low cesarean delivery prevalence (less than 10%) measures should be implemented, in addition to previous interventions discussed above, to ensure universal coverage of health services, especially in vulnerable populations that lack access to obstetric care services and to ensure assistance by qualified personnel. Health services should have adequate infrastructure to ensure safe motherhood, including capability for performing cesarean; availability of anesthesia; infection control and safe blood transfusion.
An inadequate number of qualified personnel, insufficient training of providers, and/or absence of evidence-based care guidelines, constitute a significant problem even when some health infrastructure is present. Geographical, social (migrant or refugee status) and economic barriers can prevent women from accessing available care, resulting in large health disparities within countries where the burden of maternal morbidity and mortality is often concentrated among the most vulnerable people.
In many regions of sub-Saharan Africa, lack of access to health services and trained personnel result in many women having a home birth, without the slightest conditions to do so safely. It is not the same to deliver in a hut without drinking water, light and other basic facilities, compared to delivering in an environment with all possible services and amenities, including the possibility of rapid transfer to a hospital in case of need. This explains the tragedy of prolonged obstructed labor leading to stillbirth and serious maternal damage. Obstetric-trauma-related vesico-genital fistulas a rarity in developed countries, is unfortunately common in sub-Saharan Africa. Because of the need for surgical intervention, it results in pilgrimage of women for their repair with an increase in costs estimated at $40 million per year. These human and financial burdens will continue if access to quality health services with staff trained in the monitoring and conduct of childbirth is not solved.40
It should be noted that obstructed labor is a condition observed only in these scenarios and has disappeared as a cause of death and maternal morbidity in countries with a high rate of institutional births.
Many interventions have been proposed to solve the lack of appropriate cesarean delivery when needed, including training of non-medical personnel to perform cesarean sections and administration of anesthesia. This proposed solution needs to be strictly evaluated before its final and comprehensive implementation. This recommendation should be considered only as an intermediate step until an optimum level of care achieved by most developed countries can be reached, allowing all women regardless of socioeconomic status to have a safe maternal and neonatal outcome.
PRACTICE RECOMMENDATIONS
- The cesarean delivery rate is an indicator of obstetric quality and represents a public health challenge.
- The ideal 15% cesarean delivery rate set by WHO is controversial. A recent study suggests that above a rate of 19% there is no change in maternal or perinatal mortality and morbidity.
- Cesarean delivery is associated with three times greater risk for severe adverse outcome compared to a vaginal delivery.
- Neonates born by cesarean section have an increased risk for respiratory problems, admission to intensive care, and long-term allergic problems.
- Among the most common reasons in countries with high cesarean delivery rates are interventions without medical cause and patients of high economic conditions.
- Medical causes for cesarean delivery include the following: the common diagnosis of non-reassuring fetal heart rate tracing, dystocia, failed induction, breech presentation. Appropriate protocols and education of both providers and public is necessary.
- Repeat cesarean represents a common cause of cesarean delivery. Efforts should be aimed at reducing primary cesarean delivery.
- In low-income countries, the necessary infrastructure must be established to provide comprehensive obstetric care, including training appropriate staff in the event of need to proceed with cesarean delivery.
CONFLICTS OF INTEREST
The author(s) of this chapter declare that they have no interests that conflict with the contents of the chapter.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Appropriate technology for birth. Lancet 1985;2(8452):436–7. | |
Molina G, Weiser TG, Lipsitz SR, et al. Relationship Between Cesarean Delivery Rate and Maternal and Neonatal Mortality. JAMA 2015;314(21):2263–70. | |
American College of Obstetricians and Gynecologists. Obstetric care consensus no. 1: Safe prevention of the primary cesarean delivery. Obstetrics and Gynecology 2014;123(3):693–711. | |
Sandelowski M, Bustamante R. Cesarean birth outside the natural childbirth culture. Res Nurs Health 1986;9(2):81–8. | |
Chong ESY, Mongelli M. Attitudes of Singapore women toward cesarean and vaginal deliveries. Int J Gynecol Obstet 2003;80(2):189–94. | |
Fawcett J, Pollio N, Tully A. Women's perceptions of cesarean and vaginal delivery: another look. Res Nurs Health 1992;15(6):439–46. | |
McCourt C, Weaver J, Statham H, et al. Elective cesarean section and decision making: a critical review of the literature. Birth 2007;34(1):65–79. | |
Hou L, Li G, Zou L, et al. Cesarean delivery rate and indications in mainland China a cross sectional study in 2011. Zhonghua Fu Chan Ke Za Zhi 2014;49(10):728–35. | |
Mozes B, Schiff E, Modan B. Factors affecting inappropriate hospital stay. Int J Qual Health Care 1991;3(3):211–17. | |
McMichael AJ, McKee M, Shkolnikov V, et al. Mortality trends and setbacks: global convergence or divergence? The Lancet 2004;363(9415):1155–59. | |
Hsiao WC. The Chinese health care system: lessons for other nations. Soc Sci Med 1995;41(8):1047–55. | |
Biccard BM, Madiba TE, Kluyts HL, et al. African Surgical Outcomes Study (ASOS) investigators. Perioperative patient outcomes in the African Surgical Outcomes Study: a 7-day prospective observational cohort study. Lancet 2018;391(10130):1589–98. | |
Betran AP, Ye J, Moller AB, et al. The increasing trend in Caesarean section rates: global, regional and national estimates: 1990–2014. PLoS One 2016;11(2):e0148343. | |
Boerma T, Ronsmans C, Melesse DY, et al. Global epidemiology of use of and disparities in caesarean sections. Lancet 2018;392(10155):1341–8. | |
Nakamura-Pereira M, Leal MC, Esteves-Pereira AP, et al. "Use of Robson classification to assess cesarean section rate in Brazil: the role of source of payment for childbirth. Play Health 2016;13(Suppl 3):128. | |
Althabe F, Belizán JM. Caesarean section: the paradox. Lancet 2006;368(9546):1472–3. | |
East CE, Kane SC, Davey MA, et al. Protocol for a randomised controlled trial of fetal scalp blood lactate measurement to reduce caesarean sections during labour: The Flamingo trial [ACTRN12611000172909]. Bmc Pregnancy Childbirth 2015;15(1):285. | |
Betran AP, Torloni MR, Zhang JJ, Golmezoglu AM; WHO Working Group on Caesarean Section. WHO Statement on Caesarean Section Rates. BJOG 2016;123(5):667–70. | |
Appropriate technology for birth. Lancet 1985;2(8452):436–7. | |
Norum J, Heyd A, Hjelseth B, et al. Quality of obstetric care in the sparsely populated sub-arctic area of Norway 2009–2011. BMC Pregnancy and Childbirth 2013;13:175. | |
Norwegian Directorate of Health, Quality of Care Indicators, Norwegian Directorate of Health, Oslo, Norway, 2017. | |
Miller S, Abalos E, Chamillard M, et al. Beyond too little, too late and too much, too soon: a pathway towards evidence-based, respectful maternity care worldwide. Lancet 2016;388:2176–92. | |
Deneux-Tharaux C, Carmona E, Bouvier Colle MH. Postpartum Maternal Mortality and Cesarean Delivery. Obstet & Gynecol 2006;108(3 Pt 1):541–8. | |
Liu S, Liston RM, Joseph KS, et al.; Maternal Health Study Group of the Canadian Perinatal Surveillance System. Maternal mortality and severe morbidity associated with low-risk planned cesarean delivery versus planned vaginal delivery at term. CMAJ 2007;176(4):455–60. | |
Villar J, Carroli G, Zavaleta N, et al.; World Health Organization 2005 Global Survey on Maternal and Perinatal Health Research Group. Maternal and neonatal individual risks and benefits associated with caesarean delivery: multicentre prospective study. BMJ 2007;335(7628):1025. | |
Neu J, Rushing J. Cesarean versus vaginal delivery: long-term infant outcomes and the hygiene hypothesis. Clin Perinatol 2011;38(2):321–31. | |
Benedetti FO, Agudelo RC, Rodríguez RR, et al. Prevalence of isthmuscele at the Hospital de San José in Bogota, Colombia. Revi ChiL Obstet Gynecomol 2016;81(6):465–72. | |
Society for Maternal-Fetal Medicine (SMFM). Electronic address: pubs@smfm.org, Miller R, Timor-Tritsch IE, Gyamfi-Bannerman C. Society for Maternal-Fetal Medicine (SMFM) Consult Series #49: Cesarean scar pregnancy. Am J Obstet Gynecol 2020;222(5):B2–14. | |
Renz-Polster H, David MR, Buist AS, et al. Caesarean section delivery and the risk of allergic disorders in childhood. Clin Exp Allergy 2005;35(11):1466–72. | |
Betran AP, Merialdi M, Lauer JA, et al. Rates of caesarean section: analysis of global, regional and national estimates. Paediatr Perinat Epidemiologol 2007;21(2):98–113. | |
Hannah ME, Hannah WJ, Hewson SA, et al., for the Term Breech Trial Collaborative Group. Planned caesarean section versus planned vaginal birth for breech presentation at term: a randomised multicentre trial. Lancet 2000;356(9239):1375–83. | |
Thomas J, Paranjothy S. Clinical Effectiveness Support Unit. The National Sentinel Caesarean section Audit Report. RCOG 2001. | |
Sosa C, De Mucio B. Contribution of labor induction in the increasing of c-section rates. Ten years of experiences in a LAC country. Preliminary results. Published in PAHO/CLAP/Webinar “The way of being born and its impact in the short, médium and long term” November 18th 2020. Available in: https://www.paho.org/sites/default/files/ops_presentation_sosa.pdf). | |
Grobman WA, Rice MM, Reddy UM, et al.; Eunice Kennedy Shriver National Institute of Child Health and Human Development Maternal–Fetal Medicine Units Network. Labor Induction versus Expectant Management in Low-Risk Nulliparous Women. N Engl J Med 2018;379(6):513–23. | |
56° Consejo Directivo 70.a Sesión del comité regional de la OMS para las américas. Washington, DC, EUA, del 23 al 27 de septiembre del 2018. Punto 8.14 del orden del día provisional. Plan de acción para acelerar la reducción de la mortalidad materna y la morbilidad materna grave: informe final. CD56/INF/14. 2 de julio del 2018. | |
Lien JM, Towers CV, Quilligan EJ, et al. Term early-onset neonatal seizure: Obstetric characteristics, etiology classifications, and perinatal care. Obstet Gynecol 1995;85(2):163–9. | |
Fescina R, A incidência da Cesárea nas Américas. Jornal da Federacion Brasileira de Obstetricia y Ginecologia 2000;7(1). | |
Barros AJ, Santos IS, Matijasevich A, et al. Patterns of deliveries in a Brazilian birth cohort: almost universal cesarean sections for the better-off. Rev Saude Publica 2011;45:635–43. | |
Bohren MA, Hofmeyr GJ, Sakala C, et al. Continuous support for women during childbirth. Cochrane Database of Syst Rev 2017;7. Art. No.: CD003766. | |
Wall LL. Obstetric vesicovaginal fistula as an international public-health problem. Lancet 2006;368:1201. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards program CLICK HERE)