This chapter should be cited as follows:
Pérez-Wulff JA, Márquez D, et al., Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.415493
The Continuous Textbook of Women’s Medicine Series – Obstetrics Module
Volume 13
Obstetric emergencies
Volume Editor: Dr María Fernanda Escobar Vidarte, Fundación Valle del Lili, Cali, Colombia
Chapter
Epidemiology of Extreme Maternal Morbidity and Maternal Mortality
First published: June 2021
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
During the past three decades, multiple institutions have been actively dedicated in a global effort to reduce maternal mortality (MM) and its sequelae. The International Federation of Gynecology and Obstetrics (FIGO), in its mission manifest, shows a commitment with health advertising, human rights and all women well-being, especially from those with increased risk of death and disability associated to maternity, promoting interventions based on the evidence to reduce the incidence of maternal mortalitiy (MM).1 Multiples institutions have joined this initiative at a global level, including the 190 countries that form the United Nations (UN), which are committed to achieving the Millennium Development Goals (MDGs) in which highlighted the goal of reducing MM by 75% by 2015.
Maternal Mortality Cause (MMC) has turned into the most used tool for obstetric care surveillance as a country’s basic indicator of quality. This marker has registered a decrease of 44% in the past 25 years, from a rate of 385 per 100,000 born alive in 1990 to 216 per 100,000 born alive in 2015. On other hand, the annual number of maternal deaths has been reduced by 43.9% in the same period of time from approximately 532,000 to 303,000.2 This leads to a continuous annual reduction of 2.3% slower than expected.
It is believed that there is a maternal death every minute, which represents between 500,000 and 600,000 deaths of women in fertile ages per year.3 Having this and other challenges, UN members, with a great numbers of the civil society, proclaimed a Sustainable Development agenda, which has 17 objectives to accomplish from 2015 to 2030, in which highlights the intention of reducing the MM rate to less than 70 per 100,000 born alive.3
Nowadays, MM besides constituting an indicator of the country’s human development, inequality and gender inequality, is a public health problem, where the local findings may cover variations between countries. The biggest local decrease occurred in Eastern Asia during the 1990–2015 period with a continuous annual decrease rate of 5%, and the lowest occurred in the Caribbean which was of 1.8%.4 The local MMC for 2015 varied between 12 deaths per 100,000 live births (80% IC 11–14) for developed regions and 546 (511–652) in Sub-Saharan Africa.5 In this way, the death risk related to pregnancy, birth and puerperium is 36 times higher compared to that registered in developed countries.6 The progression to a maternal death is related to the type of event, with social and demographic factors, health providers’ quality and the patient’s attitude to the sanitary system.7,8,9 Providing evidence of the achievements and individual failures related to the health of each country, provides practical orientation an inspiration in order to perform interventions destined to reduce maternal mortality, which also leads to a better comprehension of the main risk factors and possible solutions.4
1
International statistical Classification of Diseases and related health problems (ICD 10) – WHO.10
Maternal death (MD) | Any death that occurs due to pregnancy, abortion, childbirth and/or the puerperium up to 42 days after the end of the obstetric event, regardless of the duration and location of the pregnancy, due to any cause related or aggravated by the pregnancy or its management, but not due to accidental or incidental causes |
Direct maternal death | Deaths that result from obstetric complications of the gravity state (pregnancy, labor and puerperium), from interventions, omissions, incorrect treatment, or the chain of events that led to any of the above mentioned |
Indirect maternal death | Deaths that derive from a previously existing disease or disease that appeared during pregnancy and that was not due to direct obstetric causes, but that was aggravated by the physiological effects of pregnancy |
Late maternal death | Death of a woman due to direct or indirect causes more than 42 days later, but within 1 year of termination of the pregnancy |
Extreme maternal morbidity (EMM) or "near miss" | Serious maternal morbidity is that presented by a woman who almost dies but survives a complication that occurs during pregnancy, childbirth or within 42 days after the end of the pregnancy |
Maternal mortality rate | Number of maternal deaths for each 100,000 live births |
Maternal mortality ratio (MMR) | Maternal mortality ratio (MMR) |
For most women, pregnancy and birth is equal to a positive, satisfactory and without complication experience; however, maternal death is a possible result if a risk factor is not treated efficiently and at a proper time. Between these scenarios, there can be found the potentially dangerous conditions for life or extreme maternal morbidity (EMM) which could generate maternal death if it is not treated on time.5,6,7
Approximately 20 years ago, related to the decrease of MM in developed countries, the EMM was suggested as a better indicator of women’s health care during pregnancy time, birth and puerperium. Maternal morbidity and near risk for obstetrics death analysis allows a more comprehensive vision of the possible failures related to perinatal care and its epidemiologic surveillance. The World Health Organization (WHO) and the Federación Latinoamericana de Sociedades de Obstetricia y Ginecología (FLASOG) define EMM as ‘’a severe complication which occurs during pregnancy, birth or inside the 42 days after the finalization of the pregnancy, with survival due to an urgent medical intervention at the proper time’’.8,9,11 Nowadays, there is not a consensus about the total definition of the EMM diagnosis criteria, which change according to geographic region and the sanitary resources availability of each country.
In this way, during the practice of obstetric attention, most of women have adequate and free of adverse effects attention, whilst some patients die and some have a high risk of death, but survive.12,13 The study of this last group of women uses the term near-miss, which translates in to Spanish as ‘’extreme morbidity’’, serious intense maternal complications’’ or ‘’almost loss’’.14,15 The term near-miss was proposed by Stones in 1991, and it refers to an unplanned event which does not end up in death, but that could have happened, in other words, an event which put in risk the patient’s life, without causing him or her the death.16
In this way, given that the incidence of the EMM is substantially higher than the maternal deaths, its analysis and tracking give stronger evidence for the interpretation and improvement of the quality of the attention, providing a promising strategy to reduce MM. In 2009, WHO, developed a group of criteria which allow the identification of the EMM cases based on the organic insufficiency and the clinic criteria, when the laboratory and other complementary diagnosis elements are not available6,12,13 (Table 2).
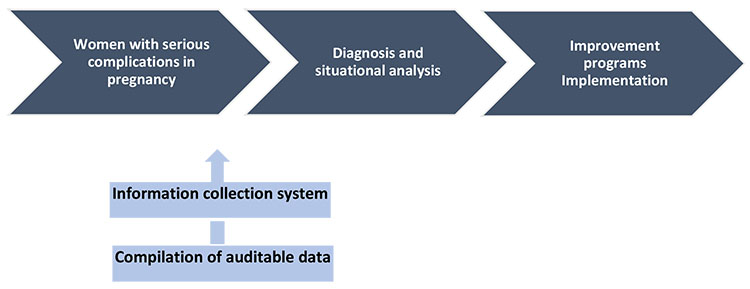
It proposes the identification and continuous tracking of the EMM and MM cases as an evaluation tool of the quality of the obstetric and perinatal attention, to subsequently lead and implement the strategies of intervention in three stages: (1) base evaluation, (2) situational analysis, and (3) intervention implementations in order to improve cares (Table 2; Figure 1).
2
Criteria for severe maternal morbidity (near miss).
System committed | Clinical criteria | Laboratory | Criteria based on Interventions |
Cardiovascular | Shock Cardiac arrest | Severe hypoperfusion (lactate >5 mmol/l or >45 mg/dl) Severe acidosis (pH <7.1) | Continuous administration of vasoactive agents. Cardiopulmonary resuscitation |
Respiratory | Acute cyanosis Panting breath Severe tachypnea (breathing frequency >40 rpm) Severe bradypnea (breathing frequency <6 rpm) | Severe hypoxemia (oxygen saturation <90% for 60 minutes or PaO2/FiO2 <200) | Intubation and ventilation no related to anesthesia |
Renal | Oliguria resistant to fluids or diuretics | Severe acute azotemia (creatinine 300 mol/l or 3.5 mg/dl) | Dialysis by acute kidney failure |
Hematological/ | Coagulation disorders | Severe acute thrombocytopenia (<50,000 platelets/ml) | Massive blood/red blood cell transfusion (3 units) |
Hepatic | Jaundice in the presence of pre-eclampsia | Severe acute hyperbilirubinemia (bilirubin >100 mol/l or >6.0 mg/dl) | Acute hyperbilirubinemia severe (bilirubin >100 mol/l or >6.0 mg/dl) |
Neurological | Prolonged unconsciousness (>12 hours)/ stroke, uncontrollable epileptic seizures/ epilepticus status. Generalized paralysis | ||
Uterine dysfunction | Infection or bleeding that lead to hysterectomy |
1
Evaluation of the quality of obstetric and perinatal care. Staged intervention strategies.
MATERNAL MORTALITY
Causes
The main action for the reduction of MM lies in the exhaustive knowledge of its causes. However, one of the difficulties in many countries is the lack of reliable vital records. The responsibility of the certified professional must also be recognized to provide accurate and useful information, improving epidemiological monitoring and establishing health policies with the best available evidence.
In a review highlighting the information provided by 115 countries and comprising 60,799 maternal deaths,9 the most affected regions are sub-Saharan Africa and South Asia, which include 83% of the MM, 73% of deaths are attributed to direct maternal causes and of these, the first etiology is obstetric hemorrhage (27% of cases). Hypertensive disorders of pregnancy rank second with 14% and obstetric sepsis ranks third with 7% of MM. It is important to highlight some specific regional variations, such as the high mortality from postpartum hemorrhage in North Africa (36%) and the dominance of hypertensive disorders of pregnancy as a direct cause of obstetric death in Latin America and the Caribbean, representing 22% of the MM in the region. The other causes of direct maternal death include abortion (12%); embolism (7%) and obstructed labor (2%). Indirect deaths represent 27% of cases worldwide and of these, 70% had a pre-existing disease. HIV represents 5% of global maternal mortality (Figure 2).17 Despite the fact that HIV infection is associated with a low number of deaths worldwide compared to other causes, increased antiretroviral coverage has led to reduced HIV-related mortality in sub-Saharan Africa and has been associated with a decrease in mortality in HIV positive pregnant women.18,19
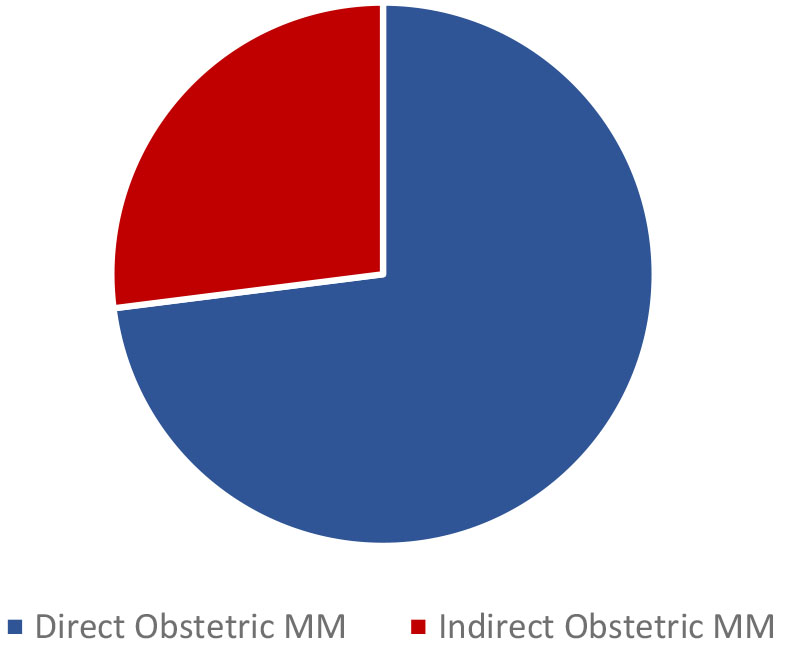
2
Maternal mortality.
The MMR has been decreased in the different age groups; however, it has been higher in the older group. MMR was highest in the oldest age groups and lowest in women aged 20–29 during 1990 and 2013. However, it decreased significantly between 1990 and 2013 for almost all age groups. Analyzing the age groups in that period of time, it was estimated that 9% of maternal deaths belong to the group aged 15–19 years, 43% in women aged 20–29 years, and 47% in those aged 30 years and over, and the rest occur in the 10–14 age group (Figure 3). Despite having higher mortality rates in older age groups, the total number of deaths is approximately the same before and after the age of 30 years. The RMM in mothers aged 15–19 years in 2013 was 1.5 times higher than in women aged 20–24 years, and 1.4 times higher than in the group aged 25–29 years.20
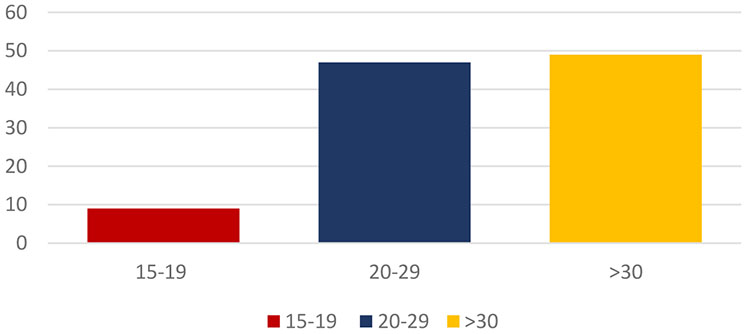
3
Maternal mortality by age.
RISK FACTORS
Within the context of maternal deaths (MM), there are different factors that can influence obstetric outcomes. Pregnancy as a physiological condition adds a risk to the pregnant woman which can be increased if previous pathologies coexist (high blood pressure, diabetes, heart disease, among others) or a body mass index greater than 30 kg/m2.21 Compared with pregnant women of normal weight, obese women have a higher risk of heart disease, sleep apnea, gestational and pregestational diabetes, pre-eclampsia, infection and deep vein thrombosis, all with high probability of complications and probable maternal death.22
Advanced maternal age (over 40 years) has also been considered as a risk factor with mortality rates 4–5 times higher than pregnant women at 20 years old,23 47% of maternal deaths occur in elderly pregnant women, for the year 2013, the MM worldwide was 9.5 times higher in women aged between 45 and 49 years when compared to pregnant women between 20 and 24 years.24
Race as a risk factor for maternal morbidity is considerable, mainly in the black women, who have 3–4 times more risk when compared to Caucasian, Asian and Hispanic.23,24,25 However, there are disparities in race and the most common causes of maternal morbidity (hemorrhage, sepsis, and hypertensive disorders), mainly in Hispanic women born in North America, where the main cause of maternal mortality in pulmonary thromboembolism, probably those differences are associated with low educational level, malnutrition, late prenatal control initiation, existing comorbidities, earlier maternal age, and late prenatal control initiation.24,25,26
The exponential and sustained increased cesarean birth rate in recent years brings with it an increase in the rate of complications inherent in surgical maneuvers postpartum hemorrhage, infection, venous thromboembolism, placenta previa and placental accretion, and death.21
There are risk factors that are assigned to each region or country, a study in Tanzania suggested that the distance between the health care center and the maternal home, as well as the quality of medical care, influenced the high rates of maternal mortality. Countries with high prevalence of HIV have improved the increase in retroviral therapy by reducing maternal mortality rates, as well as in areas of conflict, humanitarian crisis, post-conflict and natural disaster; these causes being avoidable.27
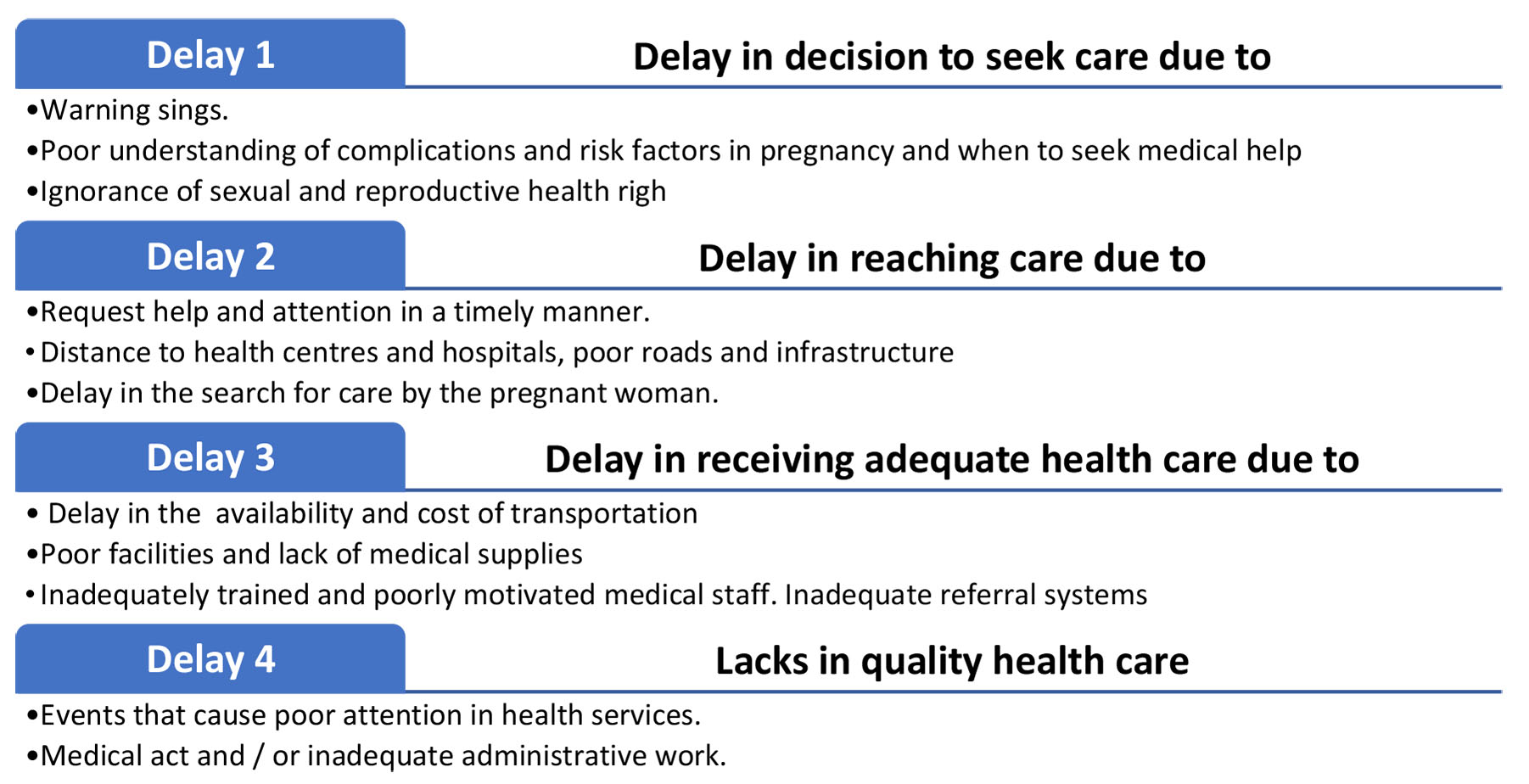
All of the aforementioned can be associated with the “three phases in the delay” of obstetric care described by Thaddeus et al.28 more than 20 years ago, that improve the care of complicated pregnant women (Figure 4).
4
Delays in the timely and adequate care of a pregnant woman according to the classification of the Pan American Health Organization.29
Taking all of the above into account, the mortality figures for each region have a multifactorial origin where the sum of them will increase the possibility of death of a pregnant woman
Causes and consequences of the extreme maternal morbidity
The importance of the study of the extreme maternal morbidity is that they are situations that do not cause a fatal repercussion in the patient’s life, they are not documented or reported, which may lead to the recurrence of the event in the future with consequences that entail to maternal death.3,13
For each maternal death, 100 cases of near miss or severe acute maternal morbidity occur. These events should be considered as an important public health problem.30,31 Globally, an extreme maternal morbidity rate of 4.8 per 1000 births has been reported, with postpartum hemorrhage and obstetric sepsis being the most common causes (Figure 5).32,33,34 In the United States of America, it is estimated that there are 50,000 cases per year, which is equivalent to 2% of all births.35 The countries of the American continent with the most cases of EMM, according to figures from WHO, are Brazil, Mexico and Cuba.36
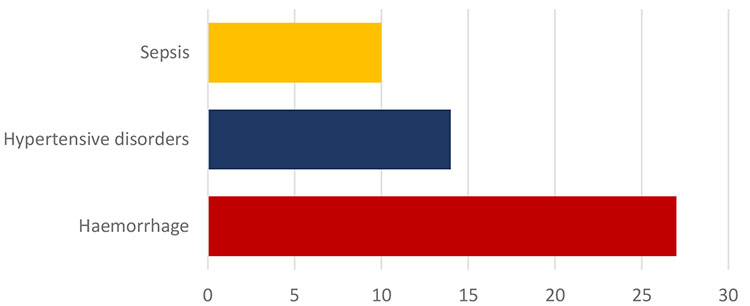
5
Main causes of maternal mortality.
The evaluation and recording of the EMM events often lack unified criteria, making diagnosis and follow-up difficult. In recent years, two European groups37,38 proposed a tool with 17 indicators, developed specifically for use in developed countries. Also, in the United States, the CDC published a list of 18 indicators, based on CIE-10, to facilitate the identification of EMM events.39 Organizations such as the American College of Obstetrics and Gynecology (ACOG) and the Society for Maternal Fetal Medicine (SMFM) recommend the use of two screening criteria: transfusion of four or more red blood cells packs and admission, during pregnancy or the puerperium, to the intensive care unit (ICU).40 Many studies have shown that the use of these criteria has a high sensitivity and specificity to identify women with EMM.41,42,43
The EMM is currently considered an important indicator of the hospital quality. Considering only the obstetrics mortality, the morbidity and other events capable of putting the patient’s life at risk without causing death are neglected, therefore, corrective actions may be insufficient.44 It is recommended an evaluation system for the quality of obstetrics health services be implemented in each hospital, in order to determine the frequency of maternal complications, cases of EMM and maternal death.45 The performance of health personnel is key to the prevention of serious complications related to birth, which will ultimately promote the implementation of programs to improve the quality of maternal care.46
There is a great advantage in the possibility of analyzing the case of a woman who survived life-threatening complications during pregnancy, childbirth or the puerperium, recognizing the obstacles and delays in receiving adequate care from basic clinical levels, the lack of local resources, poverty, social disadvantages and possible delays in the remission process.47,48 For this reason, a method used for the purpose of evaluating and achieving improvement in the care of pregnant patients is called the “path to survival”, adopted by WHO, PAHO and the United Nations Population Fund (UNFPA). The survival path is based on the fact that in order to reduce the EMM it is not enough that the health services work efficiently, but rather they should work on the barriers that generate delays for the patients to be able to access them (Figure 2).49,50
Fetal impact of the extreme maternal morbidity
The EMM not only puts the patient's life at risk, but the fetus or newborn may also suffer the consequences of the mother's extreme morbidity, such as increased risk of death, admission to the neonatal intensive care unit, preterm birth and intrauterine growth restriction. These findings reinforce the importance of carrying out preventive actions aimed at reducing the extreme maternal morbidity, since the potential benefits involve the maternal and fetal safety.46
Despite global efforts to decrease maternal mortality, it remains unacceptably high, especially in developing countries. In addition to the concern about maternal death numbers, there is a marked increase in cases of EMM, even in developed countries, with serious maternal, perinatal and social consequences.51 In order to reduce maternal morbidity and mortality, it is necessary to implement programs that allow for the timely identification of risk factors, carrying out interventions aimed at their prevention and control. Improving the effectiveness and quality of family planning, prenatal control and hospital obstetric care programs are essential measures to reduce cases of EMM.
PREVENTION STRATEGIES
The systematic review of the MM at a institutional level is unpredictable to improve the maternal results. At least 40% of the MM can be potentially preventable.52,53 Berg et al.53 showed in their study that 93% of deaths from postpartum hemorrhage, 89% of deaths are associated with chronic disease and 60% of deaths from gestational hypertension were avoidable by having in consideration that the most preventable risks factors, are those associated with de medical staff and the institution in comparation to those inherent in the pregnancy.
The prevention strategies of the maternal mortality must be orientated to the improvement of:
- Team work of the health care staff that leads to improved communication between them, improving the outcome of emergency situations. the continuous application of medical journals to prioritize situations and discuss adverse results, identifying near miss.
- The use of checklists in the daily practice, can be useful to remember all the critical steps in medical care in stressful situation. Achieving successful management in a fast, timely and coordinated manner.54,55
- Having institutional protocols to identify the many causes of maternal mortality as well as the interpretation of the different perinatal studies that guide the possible complications that may occur during labor (active management of the third period of labor, use of a partogram, fetal monitoring and a proper surgical technique.
- Simulation as a training method for the health care staff in the different management of obstetric emergencies to improve the outcome and with it the decrease in the maternal morbidity and mortality in association with continuous medical education for health care staff in emergency area.56
In the prevention strategies, the safety packages summarize the clinical practices that must be implemented in each maternity unit; organized by stages: preparation, recognition, prevention, response, reporting and learning of the system, adequate results are obtained in emergency situations that reduce maternal morbidity and mortality. One of the best examples, due to the incidence of pathology, is the package for obstetric bleeding, which has helped reduce the frequency of severe bleeding. Multi- and interdisciplinary use should be considered, as it is designed in this way to help establish a culture of safety by applying all the steps described therein.57
PRACTICE RECOMMENDATIONS
- Maternal death refers to any death that occurs due to pregnancy, abortion, childbirth and/or the puerperium up to 42 days after the end of the obstetric event, regardless of the duration and location of the pregnancy, due to any cause related or aggravated by the pregnancy or its management, but not due to accidental or incidental causes.
- Extreme maternal morbidity (EMM) or "near miss" Is a serious maternal morbidity is that presented by a woman who almost dies, but survives a complication that occurs during pregnancy, childbirth or within 42 days after the end of the pregnancy.
- The identification and continuous tracking of the EMM and MM cases as an evaluation tool of the quality of the obstetric and perinatal attention, to subsequently lead and implement the strategies of intervention in three stages: (1) base evaluation, (2) situational analysis: and (3) intervention implementation in order to improve care.
- The main causes of maternal deaths are attributed to direct maternal causes and, of these, the first etiology is obstetric hemorrhage. Hypertensive disorders of pregnancy rank second and obstetric sepsis ranks third.
- The prevention strategies, to reduce MM are the safety packages that summarize the clinical practices that must be implemented in each maternity unit. Organized by stages: preparation, recognition, prevention, response, reporting and learning of the system, adequate results are obtained in emergency situations that reduce maternal morbidity and mortality.
CONFLICTS OF INTEREST
The author(s) of this chapter declare that they have no interests that conflict with the contents of the chapter.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Federación Internacional de Ginecología y Obstetricia (FIGO). Misión y visión central de FIGO. Disponible en: https://especialidades.sld.cu/ginecobstetricia/2019/08/02/vision-central-y-mision-de-figo. | |
Bongaarts J. WHO, UNICEF, UNFPA, World Bank Group, and United Nations Population Division Trends in Maternal Mortality: 1990 to 2015 Geneva: World Health Organization, 2015. Population and Development Review 2016;42(4):726–29. | |
Transforming our World: The 2030 Agenda for Sustainable Development [Internet]. Unfpa.org. 2020 [cited 12 June 2020]. Available from: https://www.unfpa.org/resources/transforming-our-world-2030-agenda-sustainable development. | |
[Internet]. Countdown2015mnch.org. 2020 [cited 12 June 2020]. Available from: http://www.countdown2015mnch.org/documents/2015Report/Countdown_to_2015-A_Decade_of_Tracking_Progress_for_Maternal_Newborn_and_Child_Survival-The2015Report-Conference_Draft.pdf. | |
Geller SE, Rosenberg D, Cox SM, et al. The continuum of maternal morbidity and mortality: Factors associated with severity. Am J Obstet Gynecol 2016;191:939–44. | |
Say L, Souza JP, Pattinson RC; WHO working group on Maternal Mortality and Morbidity classifications. Maternal near miss-towards a standard tool for monitoring quality of maternal health care. Best Pract Res Clin Obstet Gynaecol 2009;23:287–96. | |
Cecatti JG, Souza JP, Neto AFO, et al. Prevalidation of the WHO organ dysfunction based criteria for identification of maternal near miss. Reprod Health [Internet]. BioMed Central Ltd 2018;8(1):22. | |
Kayem G, Kurinczuk J, Lewis G, et al. Risk factors for progression from severe maternal morbidity to death: a national cohort study. PLoS One 2011;6:e29077. | |
Ministerio de la Protección Social. República de Colombia. Plan de choque para la reducción de la mortalidad materna. Bogotá, 2003. Disponible en: www.0ssyr.org.ar/pdf/bibliografia/5.2.pdf. | |
WHO. The WHO application of IDC-10 to deaths during pregnancy, childbirth and the puerperium. Geneva: World Health Organization; 2012. Disponible en https://www.paho.org/clap/index.php?option=com_docman&view=download&category_slug=sip&alias=308-guia-de-la-oms-para-la-aplicacion-de-la-cie10-a-las-muertes-ocurridas-durante-el-embarazo-parto-y-puerperio-cie-mm-5&Itemid=219&lang=es. | |
Vigilancia epidemiológica de la morbilidad materna extrema. Una nueva estrategia para la reducción de la mortalidad materna en América Latina. Fondo Población Naciones Unidas (UNFPA), 2017. Disponible en: www.who.int.pmnch/events/2010/20100809_colombia.pdf. | |
World Health Organization. Evaluating the quality of care for severe pregnancy complications. The WHO near-miss approach for maternal health. Switzerland: 2019. Disponible en: http://www.who.int/about/licensing/copyright_form/en/index.html. | |
WHO, Unicef, UNFPA and The World Bank. Trends in Maternal Mortality: 1990 to 2015. Disponible en: apps. who.int/iris/bitstream/10665/44423/1/9789241500265_eng.pdf. | |
Franco YCE, Hernández PJA. Monitoreo de morbilidad materna extrema (near miss) como compromiso internacional para complementar la calidad de la atención en salud materna. Perinatol Reprod Hum 2016;30:31–8. | |
Galindo MN, Roig CN, Moreno CA, et al. Near-miss o casi pérdida en un hospital de referencia. Prog Obstet Ginecol 2017;53:399–402. | |
Stones W, Lim W, Al-Azzawi F, et al. An investigation of maternal morbidity with identification of life-threatening ‘near miss’ episodes. Health Trends 1991;23:13–5. | |
Say L, Chou D, Gemmill A, et al. Global causes of maternal death: a WHO systematic analysis. The Lancet Global Health 2014;2(6):e323–33. | |
Calvert C, Ronsmans C. The contribution of HIV to pregnancy-related mortality. AIDS 2013;27(10):1631–39. | |
Black V, Brooke S, Chersich M. Effect of Human Immunodeficiency Virus Treatment on Maternal Mortality at a Tertiary Center in South Africa. Obstetrics & Gynecology 2009;114(2, Part 1):292–9. | |
Kassebaum N, Bertozzi-Villa A, Coggeshall M, et al. Global, regional, and national levels and causes of maternal mortality during 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013. The Lancet 2014;384(9947):980–1004. | |
Hirshberg A, Srinivas S. Epidemiology of maternal morbidity and mortality. Seminars in Perinatology 2017;41(6):332–7. | |
American College of Obstetricians and Gynecologists. Practice Bulletin No 156. Obstetrics & Gynecology 2015;126(6):e112-e126. | |
Johnson T, Mulready-Ward C. Pregnancy-Related Mortality in the United States, 1998 to 2005. Obstetrics & Gynecology 2011;117(5):1229–30. | |
Creanga A, Berg C, Syverson C, et al. Pregnancy-Related Mortality in the United States, 2006–2010. Obstetrics & Gynecology 2015;125(1):5–12. | |
Creanga A, Bateman B, Kuklina E, et al. Racial and ethnic disparities in severe maternal morbidity: a multistate analysis, 2008–2010. American Journal of Obstetrics and Gynecology 2014;210(5):435.e1–435.e8. | |
Creanga A, Berg C, Syverson C, et al. Race, Ethnicity, and Nativity Differentials in Pregnancy-Related Mortality in the United States. Obstetrics & Gynecology 2012;120(2):261–68. | |
Alkema L, Chou D, Hogan D, et al. Global, regional, and national levels and trends in maternal mortality between 1990 and 2015, with scenario-based projections to 2030: a systematic analysis by the UN Maternal Mortality Estimation Inter-Agency Group. The Lancet 2016;387(10017):462–74. | |
Thaddeus S, Maine D. Too far to walk: Maternal mortality in context. Social Science & Medicine 1994;38(8):1091–110. | |
Acelas-Granados, David F; Orostegui, Andrea; Alarcón-Nivia, Miguel Ángel. Factores de riesgo para morbilidad materna extrema en gestantes sin demora en la atención médica según la estrategia camino para la supervivencia. Revista chilena de obstetricia y ginecología 2016;81(3):181–188. doi:10.4067/S0717-75262016000300003 | |
Costa OL, Ribeiro CA. Maternal near miss in the intensive care unit: clinical and epidemiological aspects. Rev Bras Ter Intensiv 2015;27:220–2. | |
Penney G, Brace V. Near miss audit in obstetrics. Curr Opin Obstet Gynecol 2007;19:145–50. | |
Kaye DK, Kakaire O, Osinde MO. Systematic review of the magnitude and case fatality ratio for severe maternal morbidity in sub-Saharan Africa between 1995 and 2010. BMC Pregnancy Childbirth 2011;11:65. | |
Van Roosmalen J, Zwart J. Severe acute maternal morbidity in high-income countries. Best Pract Res Clin Obstet Gynaecol 2009;23(3):297–304. | |
Jayaratnam S, Burton A, Connan KF, et al. Maternal ‘near miss’ at Royal Darwin Hospital: an analysis of severe maternal morbidity at an Australian regional tertiary maternity unit. Aust N Z J Obstet Gynaecol 2016;56:381–6. | |
Kilpatrick SJ, Abreo A, Gould J, et al. Confirmed severe maternal morbidity is associated with high rate of preterm delivery. Am J Obstet Gynecol 2016;215:233.e1–7. | |
Souza JP, Cecatti JG, Faundes A, et al. Maternal near miss and maternal death in the World Health Organization’s 2005 global survey on maternal and perinatal health. Bull World Health Organ 2010;88:113–9. | |
Deneux-Tharaux C, Bouvier-Colle MH, EPIMOMS Study Group. Severe acute maternal morbidity in France: the EPIMOMS population-based study. Am J Obstet Gynecol 2017;216:S345–6. | |
Geller SE, Koch AR, Garland CE, et al. A global view of severe maternal morbidity: moving beyond maternal mortality. Reprod Health 2018;15:98. | |
Centers for Disease Control and Prevention. Severe Maternal Morbidity Indicators and Corresponding ICD Codes during delivery hospitalization. 2017. Disponible en: https://www.cdc.gov/reproductivehealth/maternalinfanthealth/smm/severe-morbidity-ICD.html. | |
American College of Obstetricians and Gynecologists and the Society for Maternal–Fetal Medicine, Kilpatrick SK, Ecker JL. Severe maternal morbidity: screening and review. Am J Obstet Gynecol 2016;215:B17-B22. | |
Main EK, Abreo A, McNulty J, et al. Measuring severe maternal morbidity: validation of potential measures. Am J Obstet Gynecol 2016;214:643.e1–10. | |
Geller SE, Rosenberg D, Cox S, et al. A scoring system identified near-miss maternal morbidity during pregnancy. J Clin Epidemiol 2014;57:716–20. | |
You WB, Chandrasekaran S, Sullivan J, et al. Validation of a scoring system to identify women with near-miss maternal morbidity. Am J Perinatol 2013;30:21–4. | |
Moreno-Santillán A, Briones-Vega C, Díaz M, et al. Severe morbidity (near-miss) in obstetrics. Literature review. Rev Mex Anest 2020;43(1): 53–6. Doi: dx.doi.org/10.35366/CMA201. | |
Pattinson R, Say L, Souza JP, et al., WHO Working Group on Maternal Mortality and Morbidity Classifications. WHO maternal death and near-miss classifications. Bull World Health Organ 2009;87:734. | |
Pacagnella RC, Cecatti JG, Parpinelli MA, et al. Delays in receiving obstetric care and poor maternal outcomes: results from a national multicentre cross-sectional study. BMC Pregnancy Childbirth 2014;14:159. | |
Soni-Trinidad C, Gutiérrez-Mateos A, Santarosa-Moreno FJ, et al. Morbilidad y mortalidad materna y factores de riesgo asociados con una urgencia obstétrica [Maternal mortality and morbidity and risk factors associated with an obstetric emergency]. Ginecol Obstet Mex 2015;83(2):96–103. | |
González Ortiz L, Gómez Arias R, Vélez Álvarez G, et al. Characteristics of hospital care and its relationship to severe maternal morbidity in Medellín, Colombia. Rev Panam Salud Publica 2014;35:15–22. | |
Beyond the numbers: reviewing maternal deaths and complications to make pregnancy safer. Br Med Bull 2004;67(830):27–37. | |
Learning from ‘near-miss’ cases to end maternal death. 2019. Disponible en: https://eeca.unfpa.org/en/news/learning-near-miss-cases-end-maternal-death. | |
Bello Alvarez L, Vásquez Dielafoaut D, Rojas Suárez JA, et al. Extreme maternal morbidity indicators university clinic in third level of complexity. A retrospective evaluation. Rev Cienc Biomed 2012; 3(2):291–9. | |
Clark S, Belfort M, Dildy G, et al. Maternal death in the 21st century: causes, prevention, and relationship to cesarean delivery. American Journal of Obstetrics and Gynecology 2008;199(1):36.e1–36.e5. | |
Berg C, Harper M, Atkinson S, et al. Preventability of Pregnancy-Related Deaths. Obstetrics & Gynecology 2005;106(6):1228–34. | |
Palleja M, Solari C, Ramirez M. Listas de chequeo: Crisis en Obstetricia. Anest Analg Reanim 2017;30(2):13–35. | |
Hepner D, Rubio J, Vasco-Ramírez M, et al. Listas de chequeo de la Sociedad Colombiana de Anestesiología y Reanimación (S.C.A.R.E.) para el manejo de eventos críticos en salas de cirugía: traducción y actualización basada en la evidencia. Revista Colombiana de Anestesiología 2017;45(3):182–99. | |
Perez-Wulff J, Márquez D, González F, et al. Simulation training as a learning strategy in the management of obstetric emergencies. Latin Perinat 2017;20(2). | |
Main E, Goffman D, Scavone B, et al. National Partnership for Maternal Safety. Obstetrics & Gynecology 2015;126(1):155–62. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards program CLICK HERE)
