This chapter should be cited as follows:
Haamid FW, Al Nazer T, Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.418313
The Continuous Textbook of Women’s Medicine Series – Gynecology Module
Volume 2
Adolescent gynecology
Volume Editor: Professor Judith Simms-Cendan, University of Miami, USA
Chapter
Heavy Menstrual Bleeding in Adolescents
First published: June 2023
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
BACKGROUND
The menstrual cycle is a normal physiologic process. Menstrual health is defined as a state of complete physical, mental, and social well-being and is not limited to the absence of disease or impairment, in relation to the menstrual cycle.1 Except in the case of reproductive congenital differences of development, most individuals biologically female at birth menstruate and will experience an estimate of 400–450 episodes of menstruation during their lifetime, many of which may not be abnormal or pathologic.2 Globally, the public and medical community have engaged in increased efforts to reclaim the menstrual cycle as a normal bodily function.3 As a result of this evolving cultural shift, providers are cautioned not to over medicalize the menstrual cycle and instead engage in practices that empower and educate young females about optimal menstrual health and advocate for biologically accurate health education.4
Abnormal uterine bleeding (AUB) is a broad term that describes any deviation in menstrual bleeding or the menstrual cycle, which may include frequency (how often), duration (how long), regularity (pattern), or volume (how much).5 AUB is costly and impacts approximately one third of women across their lifespan.6 As of 2007, international experts have advised the medical community to abandon prior confusing and inadequately defined terminology such as dysfunctional uterine bleeding, menorrhagia, metrorrhagia, and menometrorrhagia.7,8 AUB subsequently became the preferred general term, which can be further characterized by terms that describe whether a woman is experiencing heavy menstrual bleeding (HMB) or spontaneous bleeding between menstrual periods referred to as intermenstrual bleeding9 (Figure 1).
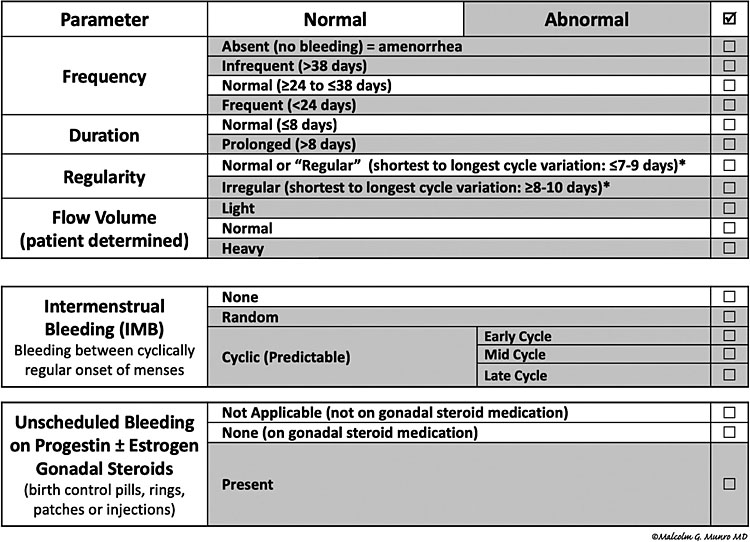
1
FIGO abnormal uterine bleeding system. Nomenclature and definitions of AUB symptoms.9
EPIDEMIOLOGY
Abnormal uterine bleeding (AUB) is a common condition that affects adolescents. In a population-based study of approximately 1000 adolescents and young adults aged 15–20 years, nearly 40 percent reported heavy menses.10 AUB has been associated with medical and psychosocial consequences, which include iron deficiency (ID) with and without anemia, frequent medical visits, and hospitalization.11 AUB negatively impacts the quality of life in adolescents in the areas of school, athletic, and vocational performance.12,13 Mental health effects are also reported in this already vulnerable population.14
PERIOD POVERTY
The growing international menstrual management movement, which includes “period poverty,” addresses this often overlooked adolescent public health concern. Providers should be aware that while no standardized tool exists to assess menstrual poverty, adolescents may experience difficulty with access to and affordability of safe menstrual products. Data from a study entitled, State of the Period 2021, which included 1,010 high school students in the US, revealed more than half had worn menstrual products longer than recommended and approximately 1 in 4 struggled to afford them. In addition, limited access to facilities to care for menstrual needs and clean water as addressed by the global community is particularly concerning in school-aged children.15,16 Adolescents with AUB who experience lengthy or frequent menstrual bleeding may be disproportionately impacted by these challenges to menstrual management.
CAUSES OF HEAVY MENSTRUAL BLEEDING
The International Federation of Obstetrics Gynecologists (FIGO) devised a widely used nine-category PALM-COEIN classification system (pronounced “palm-koin”) to categorize the causes of AUB in non-pregnant persons of reproductive age17 (Figure 2). As such, FIGO outlines the structural causes of AUB, polyp; adenomyosis; leiomyoma; malignancy and hyperplasia and the non-structural causes: coagulopathy; ovulatory dysfunction; endometrial disorders, and Iatrogenic. Non-structural causes of AUB predominate in adolescents. Ovulatory dysfunction is the most common cause of AUB in adolescents.18 Moreover, anovulatory cycles due to an immature hypothalamic-pituitary-ovarian (H-P-O) axis are normal within the first few years of menarche.18 Providers should also consider other anovulatory conditions such as hyperandrogenism, thyroid dysfunction, or hyperprolactinemia where the personal or family history is suggestive of such causes.19
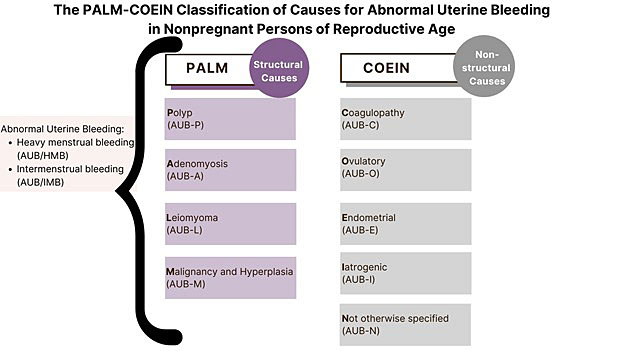
2
PALM-COEIN classification of causes of AUB.
Another aspect worth considering in a patient presenting with AUB is history of bleeding disorder or a history of anemia. Approximately 20% of adolescent girls who present for abnormal uterine bleeding evaluation and almost 33% of those hospitalized for heavy menstrual bleeding have an underlying bleeding disorder.20,21 Careful history taking is the first step to evaluate the underlying reason for AUB.
HISTORY
A detailed history is the most important first step in making the diagnosis of AUB. Unfortunately, the unnecessary stigma associated with menses and the menstrual cycle persists.22 Thus, providers should normalize discussing menstrual history with patients and their families. The American College of Obstetrics and Gynecology and the American Academy of Pediatrics recommend the menstrual cycle be regarded as a vital sign; they state once menarche (the first menses) is achieved, the menstrual cycle should be discussed at every preventative care or comprehensive visit.18 Components of a thorough history include (1) age of menarche, (2) date of last menstrual period, (3) how often menses occur, (4) how long menses lasts, and (5) number and/or frequency of menstrual products used on heaviest days of menses. Providers should assess the patient and family’s ability to access menstrual products and engage in adequate menstrual management (Table 1).
Heavy menstrual bleeding (HMB) is excessive menstrual blood loss, regardless of duration, which interferes with well-being and quality of life as reported by the menstruator. HMB is defined as more than 80 mL of menstrual blood loss in one menstrual cycle. Warner et al. utilized a logistic regression model to describe factors that predicted greater than 80 mL of menstrual blood loss per menstrual cycle.23 These three key features include rate of menstrual product change, passing clots larger than 2.5 cm or one inch in diameter, and low ferritin levels (Figure 3). The statistically significant rate of menstrual product change consistent with HMB was every one to two hours, which correlated with an odds ratio (OR) of 1, however when changed more often than hourly the OR was 3.21.
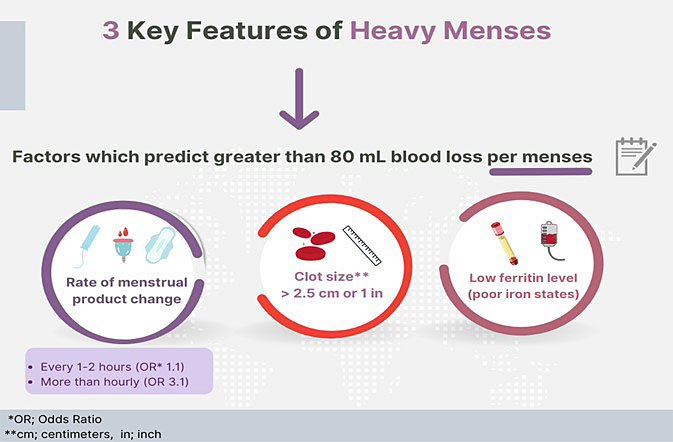
3
Three factors that predict heavy menses.
1
Menstrual history red flags.
Often changes a soaked product more than once an hour for a few hours |
Menses duration >8 days |
Wears 2 or more menstrual products at once |
Often soils clothes during daytime |
Requires a change of menstrual products overnight |
Collects menstrual flow with something other than a menstrual product |
Unable to afford or get menstrual products |
HMB in adolescents can be caused by bleeding disorders such as von Willebrand disease, platelet function defects, hemophilia, other clotting factor deficiencies, immune thrombocytopenia. Bleeding disorders may be present in patients who endorse any of the following: family history of bleeding disorder; prolonged bleeding from trivial wounds; heavy, prolonged, or recurrent bleeding after surgery or dental procedures; impressive bruising; reproductive tract bleeding including heavy menses especially if associated with iron deficiency and postpartum hemorrhage; nosebleeds (epistaxis), which last longer than ten minutes or require medical attention; and bleeding from the gastrointestinal tract that is unexplained or requires medical attention24 (Figure 4).
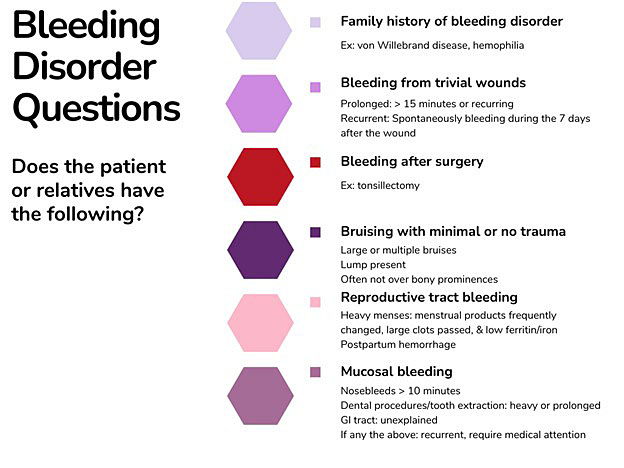
4
Bleeding disorder historical question.
Bleeding assessment tools, many of which are invalidated in adolescents, may provide key information about the patient’s menstrual bleeding. The Pictorial Bleeding Assessment Chart (PBAC) or the ISTH-BAT tools may be used though are often limited by patient recall as they are not typically collected in real time.25 Adolescents prefer menstrual calendar apps via their mobile devices compared to paper tracking, thus additional studies are needed to validate paired assessment tool-tracking app combinations in this population.26
Hypermobile Ehlers-Danlos and benign joint hypermobility syndrome are collagen disorders, which have been associated with various bleeding abnormalities, and although the etiology is not completely clear, it may be caused by changes in blood vessel architecture.27 Therefore, a patient who has a history of HMB and joint hyperflexibility, joint dislocations, hyperextensible skin, or abnormal scarring may warrant additional evaluation for a connective tissue disorder as well as a bleeding disorder.28
PHYSICAL
A physical exam provides crucial information and should be thorough and focused based on the history obtained by the provider. The provider should inform the patient and person(s) accompanying the patient that the menstrual cycle is affected by many body systems and a complete physical exam will help target the best diagnostic and treatment approaches. Adolescents should be involved in decisions about how the physical exam proceeds and emphasis should be placed on putting the adolescent at ease. For example, a patient may want a parent, guardian, caretaker, or other trusted person present during the exam. Providers should have a medical chaperone present per patient request and/or for sensitive exams including breast or genital exams.
Vital signs should be reviewed first and should include heart rate and blood pressure as abnormal blood loss may lead to hypovolemia and subsequent hemodynamic instability. Weight, height, and body mass index (BMI) are also useful tools. Providers should document the patient's general appearance, which includes skin pallor (pale skin). Conjunctival and tongue pallor are often signs of anemia. A thorough skin examination where possible will detect significant ecchymosis (bruising), petechiae (pinpoint rash), odd wound healing, and other signs of a potential hematologic cause of AUB. A careful exam of the neck for signs of thyroid disease such as goiter is important. The heart should be auscultated for tachycardia and flow murmurs as signs of anemia. An abdominal exam should involve inspection, auscultation, and palpation for tenderness and masses. Genital exams should be determined by history, performed by skilled providers, and may be warranted if there is a concern for non-menstrual bleeding such as bleeding from vaginal laceration or cervicitis. Speculum exams should be reserved for sexually active patients in select cases or scenarios.
If the history is suggestive of hyperandrogenism, providers should assess for a deepened voice, acne, and hirsutism (excessive hair in androgen sensitive areas). Other metabolic signs are elevated BMI, acanthosis nigricans, xanthomas, and striae.
In patients with HMB and very flexible joints, providers may document a Beighton score, the most widely regarded tool to assess generalized joint hypermobility.29 A positive Beighton score uses a cut-off of greater than or equal to five points out of nine and along with heavy menstrual bleeding may indicate the need for referral to hematology to test for a bleeding disorder30 (Table 2). Multiple systems are affected and often require medical attention.
2
Beighton score for joint hypermobility.*
Right | Left | |
Passively dorsiflex the fifth metacarpophalangeal joint by at least 90 degrees | 1 point | 1point |
Oppose the thumb to the volar aspect of the ipsilateral forearm | 1 point | 1 point |
Hyperextend the elbow by at least 10 degrees | 1 point | 1 point |
Hyperextend the knee by at least 10 degrees | 1 point | 1 point |
Place the hands flat on the floor without bending the knees | 1 point | |
*A total score greater than or equal to 5 points out of 9 is a positive screen.
DIAGNOSTIC APPROACH
A stepwise diagnostic approach is recommended to evaluate AUB after a thorough history and physical exam. (Figure 5). This organized approach should be guided by the clinical scenario and thoughtfully considered to minimize the emotional and financial burden to the patient. The first step of testing involves reasonable initial laboratory tests in most patients, should rule out pregnancy, conditions that are common, easily corrected, and/or life threatening as in the case of severe anemia. The second step expands the diagnostic work up to include conditions specific to endocrine dysfunction like thyroid disease, more detailed bleeding disorder evaluation such as von Willebrand disease labs, and manifestations of sexually transmitted infections such as cervicitis when applicable. The third step includes more specialized tests such as those that assess for platelet dysfunction. Tests on this last level are often indicated when prior diagnostic workup is inconclusive, in patients who do not appropriately respond to adequate therapeutic regimens and may be performed by specialists such as hematologists.
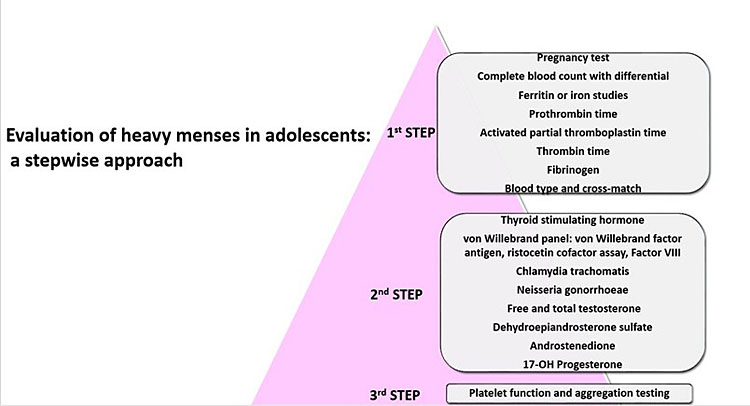
5
Evaluation of heavy menses in adolescents: a stepwise approach.
The decision to perform imaging should be based on the clinical judgement of the healthcare provider. While pelvic ultrasonography should not be obtained routinely in the work up of adolescents with heavy menstrual bleeding; imaging should be considered in patients who do not respond well to initial management or have inconclusive initial work up.31 Providers may need to add other diagnostic tests unique to their patient’s situation.
TREATMENT
The treatment of heavy menstrual bleeding in adolescents should be guided by principles of patient-centered care (Figure 6). Imminent life-threatening conditions can present many challenges to the provider–patient relationship. Nonetheless, culturally sensitive care, which respects the patient and/or family’s wishes, should be prioritized. In addition, shared decision making should be utilized to encourage patient autonomy and increase the likelihood that the patient will adhere to the treatment plan.
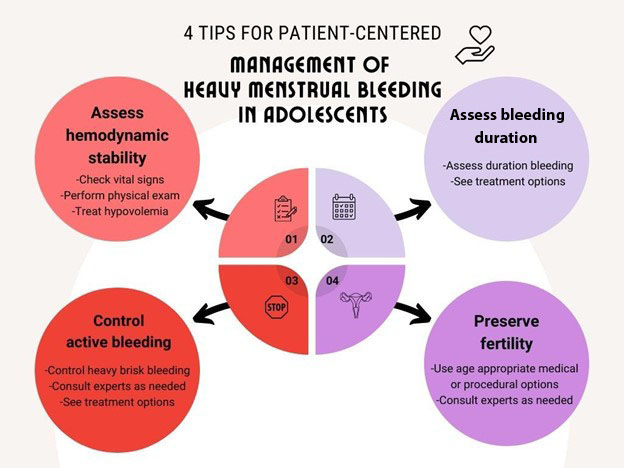
6
4 Tips for patient-centered management of heavy menstrual bleeding in adolescents.
The provider must first assess the patient’s hemodynamic stability. Vital sign compromise such as tachycardia, severe or orthostatic hypotension, or other signs of hypovolemia should be addressed with volume expansion including blood transfusions where appropriate.
The next steps are to determine whether bleeding is acute or chronic as this will heavily influence the treatment course. It is essential to control brisk or heavy bleeding with medical or procedural options, which are age appropriate and preserve fertility. It is crucial to promptly consult experts where appropriate to maximize efficiency and minimize morbidity.
HORMONAL TREATMENT
A variety of treatment options exist based on acuity of bleeding, estrogen contraindications, patient preference, and contraceptive needs.32 All available hormonal options should be discussed with patients and caregivers, which appropriately includes risks, benefits, and alternatives (Figure 7). Providers should consider the mechanisms of action of the proposed hormonal medication and be attuned to how it will impact the endometrium and thus produce the desired effect. Hormonal treatments mainly exert their effect via endometrial receptors and may be categorized as (1) combined hormonal medications, which contain estrogen and progesterone and (2) progesterone-only medications, (3) estrogen-only medications.33
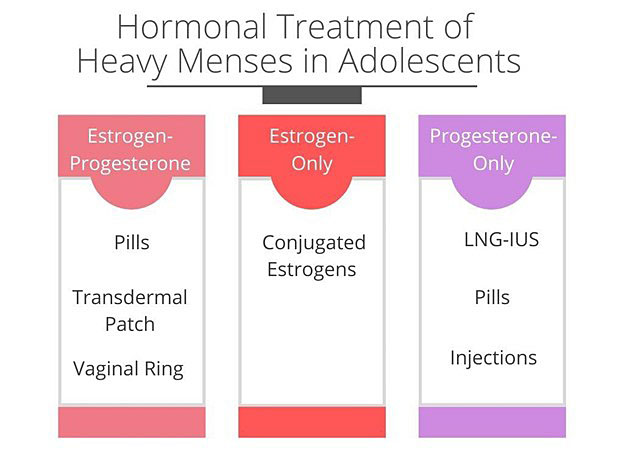
7
Hormonal treatment of heavy menses in adolescents.
Combined hormonal medications suppress ovulation and the proliferative effect of estrogen on the endometrium.34 These medications do not always necessarily address the underlying cause of bleeding. Nonetheless, combined hormonal oral contraceptive pills (OCPs) remain the most widely used treatment options for adolescents regardless of contraceptive need. OCPs offer the ability to adjust doses, avoid procedures, and may be more easily accessed. OCP dosing commonly depends on the acuity of bleeding. Tapered doses are often used to control heavy, brisk, or prolonged bleeding.35 Norethindrone acetate and medroxyprogesterone are progesterone-only oral medications that may be used in patients who have estrogen contraindications such as migraine with aura, venous thromboembolism, and uncontrolled hypertension. Patients should be counseled about the possibility of intermenstrual bleeding with hormonal treatment.
Progesterone-only options include oral medications, injections, and levonorgestrel-releasing intrauterine systems (LNG-IUS). Oral medications are effective treatment for both acute and chronic AUB. 52 mg LNG-IUS have been approved to treat AUB for over a decade. Adolescents may use LNG-IUS as first-line AUB treatment and need not be multiparous or fail other treatment options before LNG-IUS are offered by a trained provider. Medroxyprogesterone acetate administered through intramuscular or subcutaneous routes has been used to treat chronic AUB. The levonorgestrel (ENG) subcutaneous arm implant may alter the menstrual bleeding pattern of some menstruators. Thus, it is generally not regarded as first-line treatment of AUB. Patients who desire the ENG implant for contraception and AUB treatment should be counseled about potential menstrual bleeding changes and providers may proceed if patients are able to make an informed decision.
In certain cases, it may be necessary to intravenously administer conjugated estrogens at a dose of 25 mg every 6 hours and taper over 24–48 hours. This dose should be followed by a progesterone-containing medication, typically via oral route, to stabilize the endometrium.
NONHORMONAL TREATMENT
Nonhormonal treatment options should be discussed with patients and families if appropriate. Antifibrinolytic medications deactivate key points in the hemostasis pathways and thus diminish heavy menstrual flow. Tranexamic acid, an antifibrinolytic, which has been available for over a decade, successfully treats heavy menstrual bleeding in adolescents.36 It is dosed as 1300 mg by mouth three times daily for a maximum of 5 days and is taken only during menses. Lukes et al. demonstrated a 40 percent decrease in mean menstrual blood loss (MBL) as compared to placebo.37 Tranexamic acid may be an attractive treatment option in patients who do not want to take a daily medication for the entire month, have fairly regular menses, and who do not need their heavy menstrual treatment option to meet contraceptive needs. Tranexamic acid has few absolute contraindications and is well tolerated by adolescents.38
Aminocaproic acid is another antifibrinolytic agent used mostly in patients with bleeding disorders or in acute life-threatening blood loss. It can be given orally or intravenously. Gastrointestinal side effects have been documented.
Prostaglandin production is elevated in those with excessive menstrual bleeding and helps expel menstrual blood flow via contraction of the muscular outer layer of the uterus, known as the myometrium. This mechanism may explain how nonsteroidal anti-inflammatory drugs (NSAIDs), which inhibit prostaglandins help diminish MBL. A Cochrane database of systematic reviews of low to moderate evidence studies concluded NSAIDs were more effective as compared to placebo in decreasing MBL and less effective than tranexamic acid and LNG-IUS.39 There is no evidence to suggest the superiority of naproxen as compared to mefenamic acid. Oral salicylic acid and NSAIDs, particularly those that inhibit cyclooxygenase 1, are generally avoided in patients with moderate to severe bleeding disorders or those being evaluated for a bleeding disorder.
INTRAUTERINE BALLOON TAMPONADE
Intrauterine balloon tamponade has been used to control acute severe uterine bleeding although studies do not routinely include adolescents and mainly focus on postpartum hemorrhage in adults. This procedure should be reserved for skilled providers. A 30-cc Foley balloon may reasonably be used to tamponade the adolescent uterus as a stabilizing mechanical measure when medical options are ineffective.40
IRON DEFICIENCY WITH OR WITHOUT ANEMIA
AUB is the most common cause of iron deficiency in adolescents. Iron deficiency occurs on a spectrum with iron deficiency anemia (IDA) being the most severe form. Providers should correct anemia and iron deficiency and be aware that the latter may require a longer treatment course. Oral iron is the mainstay of iron deficiency treatment though it is often limited by patient adherence and gastrointestinal side effects such as upset stomach, vomiting, or constipation. Multiple divided doses of oral iron are less effectively absorbed in women with iron deficiency and anemia as compared to single or alternate daily doses.41 Low-dose single daily dosing of iron is increasingly recommended particularly in pediatric populations because it provides adequate treatment for most patients.42 65 mg elemental oral iron once daily is advised to treat iron deficiency with or without anemia and should be continued for 3 months to restore iron reserves. Hemoglobin and ferritin should be obtained 4 weeks after treatment begins. Ferritin may be used to monitor treatment response though target ferritin levels vary based on patient characteristics.43 In general, levels greater than 30 μg/mL have been suggested.
Patients who experience treatment failure of oral iron may be considered for intravenous iron infusions when available.44 The safety profile of these injectable iron formulations has steadily improved over the last two decades and anaphylaxis rarely occurs. Hematologists typically determine which patients are eligible for this treatment, which should be administered by trained personnel. In many cases, a single infusion may be administered over a relatively short time, therefore, adolescents and their caregivers may find intravenous iron infusions desirable.
TRANSFUSIONS
In general, transfusions in adolescents with heavy menstrual bleeding are guided by the hemodynamic stability and presenting symptoms of the patient, e.g., those patients with severe anemia symptoms such as tachycardia, tachypnea, and syncope.45 According to expert opinion, if blood transfusion is deemed necessary, one unit of packed red blood cells (RBCs) should be administered, and reassessment of hemodynamic status should be done before administering further blood units.45 RBC transfusions should be administered in small aliquots over several hours to minimize volume overload and its consequences. Adolescents typically respond well to hormonal management and iron transfusion even with a hemoglobin of less than 7 mg/dl. Therefore, transfusion practices should be restricted to necessary cases to minimize the risk of complications of allogenic transfusions and the theoretical risk of hemolytic disease in future pregnancies that may ensue with red blood cell antigen exposure.46
REFERRAL TO SPECIALISTS
Many manifestations of AUB including heavy menses are adequately managed without referral to a specialist. However, when possible, providers should promptly refer those with diagnostic or treatment challenges. Patients with endocrine disorders, which impact their menstrual cycles, should be managed by endocrinologists who can treat their underlying conditions. Patients with suspected or confirmed bleeding disorders should be referred to a hematologist.47 Bleeding disorders impact many other facets of a patient’s life and thus should be properly diagnosed and managed by hematologists. Where possible, persons with bleeding disorders should be treated with an interdisciplinary approach to care, which includes but is not limited to experts in the arena of reproductive health, mental health, social services, and hematology. This interdisciplinary care may be best delivered in-person or via telehealth or as dictated by individual circumstances. The comprehensive care essential to patients with HMB and bleeding disorders are increasingly being addressed through established interdisciplinary clinics, which offer consolidated centralized care, which may be appealing to adolescents and their families.48
PRACTICE RECOMMENDATIONS
- Abnormal uterine bleeding (AUB) is a broad term that describes any deviation in menstrual bleeding or the menstrual cycle, which may include frequency, duration, regularity, or volume. This general term can further be characterized as heavy menstrual bleeding (HMB) and as intermenstrual bleeding (IMB).
- Abnormal uterine bleeding (AUB) and heavy menstrual bleeding (HMB) are common conditions during adolescence. These conditions have been associated with significant medical and psychological consequences in the adolescent population.
- History taking and physical exam are the first steps that health care providers should use in assessment of AUB while exploring the most common causes in adolescent such as anovulation and bleeding disorders. Therefore, providers should strive to normalize discussion of menstrual history with patients and their families.
- Ovulatory dysfunction is the most common cause of AUB in adolescents. Anovulatory cycles due to an immature hypothalamic-pituitary-ovarian axis (H-P-O) are normal within the first few years of menarche. Providers should also consider other anovulatory conditions such as hyperandrogenism and thyroid dysfunction.
- Heavy menstrual bleeding (HMB) may be the first presentation of an underlying bleeding disorder in adolescents. Bleeding disorders work up should be performed in those with suggestive histories.
- Menstrual blood loss is the most common cause of iron deficiency in adolescents, with or without anemia. Providers should correct anemia and iron deficiency and be aware that the latter may require a longer treatment course.
- Treatment of HMB in adolescents should be guided by the principle of patient centered care. Treatment options are both medical and non-medical. Medical treatments can be hormonal and nonhormonal.
- Global and individual efforts should be targeted to address the root causes and possible solutions for the public health concern, that is period poverty.
CONFLICTS OF INTEREST
The author(s) of this chapter declare that they have no interests that conflict with the contents of the chapter.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Hennegan J, Winkler IT, Bobel C, et al. Menstrual health: a definition for policy, practice, and research. Sex Reprod Health Matters [internet] 2021;29(1):1911618. Available from: Menstrual health: a definition for policy, practice, and research – PMC (nih.gov). DOI: 10.1080/26410397.2021.1911618. PMID: 33910492; PMCID: PMC8098749. | |
Critchley HOD, Babayev E, Bulun SE, et al. Menstruation: science and society. Am J Obstet Gynecol [internet] 2020;223(5):624–664. Available from: https://www.sciencedirect.com/science/article/pii/S0002937820306190. DOI: 10.1016/j.ajog.2020.06.004. PMID: 32707266; PMCID: PMC7661839. | |
The Lancet Child & Adolescent Health. Normalizing menstruation, empowering girls. The Lancet Child & Adolescent Health [internet] 2018;2(6):379. Available from: https://www.sciencedirect.com/science/article/pii/S2352464218301433. DOI: https://doi.org/10.1016/S2352-4642(18)30143-3. | |
Starrs AM, Ezeh AC, Barker G, et al. Accelerate progress – sexual and reproductive health and rights for all: report of the Guttmacher–Lancet Commission, The Lancet [internet] 2018;391(10140):2642–92 Available from: https://www.sciencedirect.com/science/article/pii/S0140673618302939. DOI: https://doi.org/10.1016/S0140-6736(18)30293-9. | |
Munro MG, Critchley HOD, Fraser IS; FIGO Menstrual Disorders Committee. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet [internet] 2018;143(3):393–408. Available from: The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions – Munro – 2018 – International Journal of Gynecology & Obstetrics – Wiley Online Library. DOI: 10.1002/ijgo.12666. Epub 2018 Oct 10. Erratum in: Int J Gynaecol Obstet 2019;144(2):237. PMID: 30198563. | |
Liu Z, Doan QV, Blumenthal P, et al. A systematic review evaluating health-related quality of life, work impairment, and healthcare costs and utilization in abnormal uterine bleeding. Value Health [internet] 2007;10(3):183–94. Available from: A Systematic Review Evaluating Health-Related Quality of Life, Work Impairment, and Health-Care Costs and Utilization in Abnormal Uterine Bleeding – ScienceDirect. DOI: 10.1111/j.1524-4733.2007.00168.x. PMID: 17532811. | |
Fraser IS, Critchley HO, Munro MG. Abnormal uterine bleeding: getting our terminology straight. Curr Opin Obstet Gynecol [internet] 2007;19(6):591–5. Available from: Abnormal uterine bleeding: getting our terminology straight : Current Opinion in Obstetrics and Gynecology (lww.com). DOI: 10.1097/01.aids.0000299801.42415.8a. PMID: 18007139. | |
Fraser IS, Critchley HO, Munro MG. Abnormal uterine bleeding: getting our terminology straight. Curr Opin Obstet Gynecol [internet] 2007;19(6):591–5. Available from: Abnormal uterine bleeding: getting our terminology straight : Current Opinion in Obstetrics and Gynecology (lww.com). DOI: 10.1097/01.aids.0000299801.42415.8a. PMID: 18007139. | |
Munro MG, Critchley HOD, Fraser IS; FIGO Menstrual Disorders Committee. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet [internet] 2018;143 (3):393–408. Available from: The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions – Munro – 2018 – International Journal of Gynecology & Obstetrics – Wiley Online Library. DOI: 10.1002/ijgo.12666. Epub 2018 Oct 10. Erratum in: Int J Gynaecol Obstet 2019;144(2):237. PMID: 30198563. | |
Friberg B, Ornö AK, Lindgren A, et al. Bleeding disorders among young women: population-based prevalence study. Acta Obstet Gynecol Scand 2006;85(2):200–6. DOI: 10.1080/00016340500342912. PMID: 16532915. | |
Haamid F, Sass AE, Dietrich JE. Heavy Menstrual Bleeding in Adolescents. J Pediatr Adolesc Gynecol [internet] 2017;30(3):335–40. Available from: Heavy Menstrual Bleeding in Adolescents – ScienceDirect. DOI: 10.1016/j.jpag.2017.01.002. Epub 2017 Jan 17. Erratum in: J Pediatr Adolesc Gynecol 2017;30(6):665. PMID: 28108214. | |
Kendel NE, Haamid FW, Christian-Rancy M, et al. Characterizing adolescents with heavy menstrual bleeding and generalized joint hypermobility. Pediatr Blood Cancer [internet] 2019;66:e27675. Available form: Characterizing adolescents with heavy menstrual bleeding and generalized joint hypermobility – Kendel – 2019 – Pediatric Blood & Cancer – Wiley Online Library. DOI: https://doi.org/10.1002/pbc.27675. | |
Nur Azurah AG, Sanci L, Moore E, et al. The quality of life of adolescents with menstrual problems. J Pediatr Adolesc Gynecol [internet] 2013;26(2):102–8. Available from: The Quality of Life of Adolescents with Menstrual Problems – ScienceDirect. DOI: 10.1016/j.jpag.2012.11.004. | |
Dietrich JE, Yee DL, Santos XM, et al. Assessment of an Electronic Intervention in Young Women with Heavy Menstrual Bleeding. J Pediatr Adolesc Gynecol [Internet] 2017;30(2):243–6. Available from: Assessment of an Electronic Intervention in Young Women with Heavy Menstrual Bleeding – ScienceDirect. DOI: 10.1016/j.jpag.2016.10.006. Epub 2016 Oct 15. PMID: 27751907. | |
Sommer M, Caruso BA, Sahin M, et al. A Time for Global Action: Addressing Girls' Menstrual Hygiene Management Needs in Schools. PLoS Med [internet] 2016;23;13(2): e1001962. Available from: A Time for Global Action: Addressing Girls’ Menstrual Hygiene Management Needs in Schools | PLOS Medicine. DOI: 10.1371/journal.pmed.1001962. PMID: 26908274; PMCID: PMC4764363. | |
Critchley HOD, Babayev E, Bulun SE, et al. Menstruation: science and society. Am J Obstet Gynecol [internet] 2020;223(5):624–64. Available from: Menstruation: science and society (nih.gov). DOI: 10.1016/j.ajog.2020.06.004. PMID: 32707266. | |
Munro MG, Critchley HOD, Fraser IS FIGO Menstrual Disorders Committee. The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions. Int J Gynaecol Obstet [internet] 2018;143(3):393–408. Available from: The two FIGO systems for normal and abnormal uterine bleeding symptoms and classification of causes of abnormal uterine bleeding in the reproductive years: 2018 revisions – Munro – 2018 – International Journal of Gynecology & Obstetrics – Wiley Online Library. DOI: 10.1002/ijgo.12666. Epub 2018 Oct 10. Erratum in: Int J Gynaecol Obstet 2019;144(2):237. PMID: 30198563. | |
Screening and Management of Bleeding Disorders in Adolescents with Heavy Menstrual Bleeding: ACOG COMMITTEE OPINION, Number 785. Obstet Gynecol 2019;134(3):e71–83. DOI:10.1097/AOG.0000000000003411. PMID: 31441825. | |
Borzutzky C, Jaffray J. Diagnosis and Management of Heavy Menstrual Bleeding and Bleeding Disorders in Adolescents. JAMA Pediatr [internet] 2020;174(2):186–94. Available from: Diagnosis and Management of Heavy Menstrual Bleeding and Bleeding Disorders in Adolescents | Adolescent Medicine | JAMA Pediatrics | JAMA Network. DOI: 10.1001/jamapediatrics.2019.5040. | |
Haamid F, Sass AE, Dietrich JE. Heavy menstrual bleeding in adolescents. J Pediatr Adolesc Gynecol [internet] 2017;30(3):335–40. 5. Available from: https://www.sciencedirect.com/science/article/pii/S1083318816302534. DOI: https://doi.org/10.1016/j.jpag.2017.01.002. | |
Smith YR, Quint EH, Hertzberg RB. Menorrhagia in adolescents requiring hospitalization. J Pediatr Adolesc Gynecol [internet] 1998;11(1):13–5. Available from: Menorrhagia in Adolescents Requiring Hospitalization – ScienceDirect. DOI: 10.1016/s1083-3188(98)70101-9. PMID: 9526820. | |
Gül Yücel, Mustafa Kendirci, Ülkü Gül. Menstrual Characteristics and Related Problems in 9- to 18-Year-Old Turkish School Girls. J Pediatr Adolesc Gynecol [Internet] 2018;31(4):350–5. ISSN 1083–3188. Available from: https://www.sciencedirect.com/science/article/pii/S108331881830175X. DOI: https://doi.org/10.1016/j.jpag.2018.03.002. | |
Warner PE, Critchley HO, Lumsden MA, et al. Menorrhagia II: is the 80-mL blood loss criterion useful in management of complaint of menorrhagia? Am J Obstet Gynecol [internet] 2004;190(5):1224–9. Available from: Menorrhagia II: is the 80-mL blood loss criterion useful in management of complaint of menorrhagia? – ScienceDirect. DOI: 10.1016/j.ajog.2003.11.016. PMID: 15167822. | |
James AH, Kouides PA, Abdul-Kadir R, et al. Von Willebrand disease and other bleeding disorders in women: consensus on diagnosis and management from an international expert panel. Am J Obstet Gynecol [internet] 2009;201(1):12.e1–8. ISSN 0002–9378, Available from: https://www.sciencedirect.com/science/article/pii/S0002937809004104. DOI: https://doi.org/10.1016/j.ajog.2009.04.024. | |
Sanchez J, Andrabi S, Bercaw JL, et al. Quantifying the PBAC in a pediatric and adolescent gynecology population. Pediatr Hematol Oncol [internet] 2012;29(5):479–84. Available from: Full article: Quantifying the PBAC in a Pediatric and Adolescent Gynecology Population (tandfonline.com). DOI: 10.3109/08880018.2012.699165. PMID: 22866673. | |
Jacobson AE, Vesely SK, Haamid F, et al. Mobile Application vs. Paper Pictorial Blood Assessment Chart to Track Menses in Young Women: A Randomized Cross-over Design. J Pediatr Adolesc Gynecol [internet] 2018. Available from: https://linkinghub.elsevier.com/retrieve/pii/S1083-3188 (17)30266-8. DOI: 10.1016/j.jpag.2017.09.009. Epub 2017 Oct 10. PMID: 29030160. | |
Malfait F, Francomano C, Byers P, et al. The 2017 international classification of the Ehlers-Danlos syndromes. Am J Med Genet C Semin Med Genet [internet] 2017;175(1):8–26. Available from: The 2017 international classification of the Ehlers–Danlos syndromes – Malfait – 2017 – American Journal of Medical Genetics Part C: Seminars in Medical Genetics – Wiley Online Library. DOI: 10.1002/ajmg.c.31552. PMID: 28306229. | |
Kendel NE, Haamid FW, Christian-Rancy M, et al. Characterizing adolescents with heavy menstrual bleeding and generalized joint hypermobility. Pediatr Blood Cancer [internet] 2019;66:e27675. Available form: Characterizing adolescents with heavy menstrual bleeding and generalized joint hypermobility – Kendel – 2019 – Pediatric Blood & Cancer – Wiley Online Library. DOI: https://doi.org/10.1002/pbc.27675. | |
The Ehlers-Danlos Society. Assessing joint hypermobility. https://www.ehlers-danlos.com/assessing-joint-hypermobility/. Accessed May 20, 2022. | |
Kendel NE, Haamid FW, Christian-Rancy M, et al. Characterizing adolescents with heavy menstrual bleeding and generalized joint hypermobility. Pediatr Blood Cancer [internet] 2019;66:e27675. Available form: Characterizing adolescents with heavy menstrual bleeding and generalized joint hypermobility – Kendel – 2019 – Pediatric Blood & Cancer – Wiley Online Library. DOI: https://doi.org/10.1002/pbc.27675. | |
ACOG committee opinion no. 557: Management of acute abnormal uterine bleeding in nonpregnant reproductive-aged women. Obstet Gynecol [internet] 2013;121(4):891–6. Available from: Committee Opinion No. 557: Management of Acute Abnormal Uter... : Obstetrics & Gynecology (lww.com). DOI: 10.1097/01.AOG.0000428646.67925.9a. PMID: 23635706. | |
Borzutzky C, Jaffray J. Diagnosis and Management of Heavy Menstrual Bleeding and Bleeding Disorders in Adolescents. JAMA Pediatr [internet] 2020;174(2):186–94. Available from: Diagnosis and Management of Heavy Menstrual Bleeding and Bleeding Disorders in Adolescents | Adolescent Medicine | JAMA Pediatrics | JAMA Network. DOI: 10.1001/jamapediatrics.2019.5040. | |
Jain V, Chodankar RR, Maybin JA, et al. Uterine bleeding: how understanding endometrial physiology underpins menstrual health. Nat Rev Endocrinol [internet] 2022;18:290–308. Available from: Uterine bleeding: how understanding endometrial physiology underpins menstrual health | Nature Reviews Endocrinology. DOI: https://doi.org/10.1038/s41574-021-00629-4. | |
Jain V, Chodankar RR, Maybin JA, et al. Uterine bleeding: how understanding endometrial physiology underpins menstrual health. Nat Rev Endocrinol [internet] 2022;18:290–308. Available from: Uterine bleeding: how understanding endometrial physiology underpins menstrual health | Nature Reviews Endocrinology. DOI: https://doi.org/10.1038/s41574-021-00629-4. | |
Emans, Laufer, Goldstein’s. Pediatric and Adolescent Gynecology, 7th edn. Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins. 7th edn, 2019. | |
O'Brien SH, Saini S, Ziegler H, et al. An Open-Label, Single-Arm, Efficacy Study of Tranexamic Acid in Adolescents with Heavy Menstrual Bleeding. J Pediatr Adolesc Gynecol [internet] 2019;32(3):305–11. Available from: An Open-Label, Single-Arm, Efficacy Study of Tranexamic Acid in Adolescents with Heavy Menstrual Bleeding – ScienceDirect. DOI: 10.1016/j.jpag.2019.01.009. Epub 2019 Feb 5. PMID: 30731217. | |
Lukes AS, Baker J, Eder S, et al. Daily menstrual blood loss and quality of life in women with heavy menstrual bleeding. Women’s Health (Lond) [internet] 2012;8(5):503–11. Available from: Daily Menstrual Blood Loss and Quality of Life in Women with Heavy Menstrual Bleeding – Andrea S Lukes, Jeffrey Baker, Scott Eder, Tammie L Adomako, 2012 (sagepub.com). DOI: 10.2217/whe.12.36. PMID: 22934724. | |
O'Brien SH, Saini S, Ziegler H, et al. An Open-Label, Single-Arm, Efficacy Study of Tranexamic Acid in Adolescents with Heavy Menstrual Bleeding. J Pediatr Adolesc Gynecol [internet] 2019;32(3):305–11. Available from: An Open-Label, Single-Arm, Efficacy Study of Tranexamic Acid in Adolescents with Heavy Menstrual Bleeding – ScienceDirect. DOI: 10.1016/j.jpag.2019.01.009. Epub 2019 Feb 5. PMID: 30731217. | |
Bofill Rodriguez M, Lethaby A, Farquhar C. Non-steroidal anti-inflammatory drugs for heavy menstrual bleeding. Cochrane Database Syst Rev [internet] 2019;9(9):CD000400. Available from: Non‐steroidal anti‐inflammatory drugs for heavy menstrual bleeding – Bofill Rodriguez, M – 2019 | Cochrane Library. DOI: 10.1002/14651858.CD000400.pub4. | |
James AH, Kouides PA, Abdul-Kadir R, et al. Evaluation and management of acute menorrhagia in women with and without underlying bleeding disorders: consensus from an international expert panel. Eur J Obstet Gynecol Reprod Biol [internet] 2011;158(2):124–34. Available from: Evaluation and management of acute menorrhagia in women with and without underlying bleeding disorders: consensus from an international expert panel – ScienceDirect. DOI: 10.1016/j.ejogrb.2011.04.025. Epub 2011 Jun 1. PMID: 21632169. | |
Stoffel NU, Zeder C, Brittenham GM, et al. Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient anemic women. Haematologica [internet] 2020;105(5):1232–9. Available from: Iron absorption from supplements is greater with alternate day than with consecutive day dosing in iron-deficient anemic women | Haematologica. DOI: 10.3324/haematol.2019.220830. Epub 2019 Aug 14. PMID: 31413088; PMCID: PMC7193469. | |
Powers, JM, O'Brien, SH. How I approach iron deficiency with and without anemia. Pediatr Blood Cancer 2019;66(3):e27544. Available from: How I approach iron deficiency with and without anemia – Powers – 2019 – Pediatric Blood & Cancer – Wiley Online Library. DOI: https://doi.org/10.1002/pbc.27544. | |
Powers JM, Thompson DI. The Development of Ironchild: A Web-Based Intervention to Improve Adherence in Children with Iron Deficiency Anemia. Blood 2019;134(1):2163. Available from: The Development of Ironchild: A Web-Based Intervention to Improve Adherence in Children with Iron Deficiency Anemia | Blood | American Society of Hematology (ashpublications.org). DOI: https://doi.org/10.1182/blood-2019-124181. | |
Powers JM, O'Brien SH. How I approach iron deficiency with and without anemia. Pediatr Blood Cancer 2019;66(3):e27544. Available from: How I approach iron deficiency with and without anemia – Powers – 2019 – Pediatric Blood & Cancer – Wiley Online Library. DOI: https://doi.org/10.1002/pbc.27544. | |
Screening and Management of Bleeding Disorders in Adolescents With Heavy Menstrual Bleeding: ACOG COMMITTEE OPINION, Number 785. Obstet Gynecol [internet] 2019;134(3):e71–83. Available from: Screening and Management of Bleeding Disorders in Adolescent... : Obstetrics & Gynecology (lww.com). DOI: 10.1097/AOG.0000000000003411. PMID: 31441825. | |
Napolitano LM, Kurek S, Luchette FA, et al. Clinical practice guideline: red blood cell transfusion in adult trauma and critical care. EAST Practice Management Workgroup, American College of Critical Care Medicine (ACCM), Taskforce of the Society of Critical Care Medicine (SCCM). J Trauma 2009;67:1439–42. | |
O'Brien SH. Evaluation and management of heavy menstrual bleeding in adolescents: the role of the hematologist. Hematology Am Soc Hematol Educ Program [internet] 2018;2018(1):390–8. Available from: Evaluation and management of heavy menstrual bleeding in adolescents: the role of the hematologist (nih.gov). DOI: 10.1182/asheducation-2018.1.390. PMID: 30504337; PMCID: PMC6246024. | |
Zia A, Lau M, Journeycake J, et al. Developing a multidisciplinary Young Women's Blood Disorders Program: a single-centre approach with guidance for other centres. Haemophilia [internet] 2016;22(2):199–207. Available from: Developing a multidisciplinary Young Women's Blood Disorders Program: a single‐centre approach with guidance for other centres – Zia – 2016 – Haemophilia – Wiley Online Library. DOI: 10.1111/hae.12836. Epub 2016 Jan 29. PMID: 26822547. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards program CLICK HERE)
