This chapter should be cited as follows:
Huneeus A, Obach A, Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.418153
The Continuous Textbook of Women’s Medicine Series – Gynecology Module
Volume 2
Adolescent gynecology
Volume Editor: Professor Judith Simms-Cendan, University of Miami, USA
Chapter
Social Determinants of Health in Pediatric and Adolescent Gynecology
First published: October 2022
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
At the beginning of the 20th century Margaret Mead, from her ethnographic observations in Samoa,1 described the differences in childhood development according to the cultural contexts in which they were raised. The anthropologist said that the physiologic changes of this stage of life are not enough to explain the difficulties faced by this group in the western world, but what facilitates or hinders this transition must be attributed to the social and cultural framework in which young people develop. Mead's ideas were precursors in putting emphasis on social contexts when analyzing adolescents and young people sexuality. This perspective challenges the approach of much of the epidemiology, which seeks to identify individual risk factors of disease,2 and accounts that culture actually influences human health. Our way of life, our learned behavior, our techniques to adjusting to the environment, and our ways of feeling and believing, all influence our susceptibility to illness.3 The social determinants of health (SDH) focus on how social contexts affect health and also the pathways by which social conditions and environment translate into health effects.4 The SDH are based on the premise that health follows a social gradient: the higher the social position, the better the health and that the standard of health declines with every step down the social hierarchy.2
SDH are defined as “the conditions in which people are born, grow, live, work, and age”. These conditions or circumstances are shaped by families and communities and by the distribution of social position, gender, ethnicity, access to resources, and other social determinants at worldwide, national, and local levels.4 In the context of SDH, emerging evidence-based research suggests that in addition to medical care, nonmedical factors affect health and well-being of youth.5 Young people grow to adulthood within a complex web of family, peer, community, societal, and cultural influences that affect their well-being.4 Although adolescents and young people are considered a relatively healthy group, they are at greater risk of suffering morbidity and mortality in sexual and reproductive health issues, because they encounter difficulties in accessing sexual and reproductive healthcare and sex education.6 Globally adolescents are considered a priority group due to their vulnerability and the unfavorable conditions in which many of them live and develop. Factors such as low educational level, high rates of unplanned pregnancy, and other social determinants disfavor and socially exclude them, particularly in developing countries.7
Along with the above, there are dramatic gender inequities regarding the consequences of sexual and reproductive health risks for adolescent women:
- Adolescents account for 23% of the overall burden of disease because of pregnancy and childbirth;
- Early childbearing is associated with higher maternal mortality and morbidity rates and increased risk of induced abortions;
- Maternal causes constitute the leading cause of death among adolescent females;
- Gender-based violence in adolescents, especially girl and female genital mutilation/cutting are a significant and widespread problem;
- Globally, young women represent more than 60% of all young people living with HIV.8
The purpose of this chapter is to define the role that social and cultural factors have in the sexual and reproductive health of adolescent women, and to outline possibilities of intervention. Although the problems involved in sexual and reproductive health of young women are multiple and highly complex, we will address four specific outcomes: (i) teenage pregnancy, (ii) abortion, (iii) sexually transmitted infections, and (iv) contraceptive use. Awareness of the influence of SDH in adolescent women can help reduce health inequities experienced by them worldwide.
ADOLESCENT PREGNANCY
Adolescent pregnancy is a public health issue that affects the well-being of adolescents, their children, and society. It causes a set of negative consequences, especially for women, perpetuating social and gender inequities. While the estimated global adolescent-specific fertility rate has declined worldwide by 11.6% over the past 20 years, there are big differences in rates across the regions. According to the World Health Organization (WHO), every year, an estimated 21 million girls aged 15–19 years in the developing world become pregnant and approximately 12 million of them give birth.9 Even in developed countries, which present better global results in the reduction of adolescent pregnancy, marked variations exist across racial, ethnic, and geographic populations.10
The literature consistently shows that low socioeconomic status is significantly associated with adolescent pregnancy (Figure 1).11,12,13,14 Unsafe neighborhoods, low education levels and school desertion, having mothers who gave birth before their 20s, marginalization and poverty are conditions positively associated to early adolescent maternity.11,14 Pregnant adolescents tend to drop out of school early, even if they desired further education, thus perpetuating poverty.10,12,13
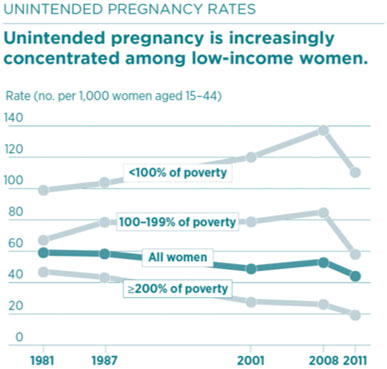
1
Unintended pregnancy rates in the United States
by socio-economic status (open access online https://www.guttmacher.org/fact-sheet/unintended-pregnancy-united-states).
The majority of teenage pregnancies are not planned nor is there a conscious decision making from adolescent mothers about their family planning.14,15,16 Nevertheless, in many low-income contexts, early pregnancy and motherhood has been described as a way to acquire a higher social status and respect from family and social surroundings.17,18,19,20
Regarding mental health, findings suggest that depression in adolescent girls acts as a risk factor for unplanned pregnancy in racial-minority and lower-income groups.21,22
Certain SDH increase high-risk sexual behavior in adolescents that lead to unintended pregnancy, like the nonuse of contraceptive methods and the early initiation of sexual activity.23,24 These behaviors have correlated with low economic income and low levels of education and living in rural communities, and belonging to unsafe environments.23,24 Due to these high-risk behaviors, adolescents that get pregnant once have a high rate of repeat pregnancy during adolescence.25,26
In societies where sexuality remains a taboo, sociocultural beliefs limit access to appropriate sexually and reproductive care and favor adolescent pregnancy.27,30 Societies with traditional gender roles, assign women and adolescent girls the responsibility of preventing pregnancies, whereas men adopt a secondary role.31
Adverse childhood experiences, including sexual abuse, community violence exposure, being a refugee, or having unsatisfied basic needs are associated with an increased risk of teenage pregnancy.32,33,34,35,36 Also, a history of violence in already pregnant adolescents leads them to have lower schooling, lower incomes, and short-term life projects compared to those without exposure to violence.37,38
Efforts to understand the problem of adolescent pregnancy have been present for decades and have become a public health priority. Interventions to prevent it have had to incorporate new visions, focusing on gender, culture, human rights, racial and socioeconomic inequalities.
Examples of interventions based on SDH that reduce adolescent pregnancy39
- Establishment of free confidential contraceptive services at outreach primary level clinics.
- Conditional cash transfers of a monthly stipend to families, subject to conditions related to school attendance, health talks and check-ups, and nutrition.
- Extending compulsory school hours.
- Skills-based program that combine classroom training, internship placements, and integrated socio-emotional skills building that increase vulnerable youth expectations about the future.
- Contraceptive services targeted to vulnerable adolescents that promote highly effective long-acting reversible contraception (implants and intrauterine devices) over other forms of contraception.40
ABORTION
Although adolescent pregnancy is usually an unwanted outcome in adolescents, the rate in which they choose to terminate their pregnancy with an induced abortion varies according to local, legal, and social contexts. Most teenage pregnancies in the developed world end in induced abortion.41
In countries where abortion is legal, risk factors for adolescent abortion are similar to the risk factors for adolescent pregnancy. Girls with lower socio-economic status, lower educational attainment, and rural residency are the ones who tend to have more induced abortions.42,43,44 This can be explained because these young women concentrate social and individual determinants of health that expose them to a higher risk of unwanted pregnancy.
In countries where abortion is restricted, and information is scarce due to illegality, studies show high socio-economic status women have more illegal abortions. Chae et al. state that in countries of low and medium income, women with higher socio-economic status have more access to abortions.45 A study in Chile where abortion is restricted only to maternal life risk, fatal fetal anomalies, or rape, showed that participants with high socio-economic status had 4.89 (95%[CI], 1.44–16.51) higher odds of induced abortion compared with participants with low socio-economic status. In Chile, low socio-economic status adolescent delivery rates are eight times higher than high socio-economic adolescent delivery rates. Unequal access to unsafe abortion can partly explain that disparity.46 In Ethiopia where abortion is allowed in cases of rape, incest, and fetal body impairment and if a woman has a physical or mental disability; or if she is younger than 18 years old, middle wealthier youths experienced more abortions compared to the poor ones.47 This could be explained because in restricted conditions, high socio-economic status youth have better access to information on how to have an abortion, better access to clinical services including across the border abortion, and more empowerment to act according to their fertility preferences compared with women who have a lower socio-economic status.
Abortion legislation impacts local social determinants of adolescent abortion. Where abortion is legal, vulnerable adolescents have more abortions, where abortion is illegal, vulnerable adolescents have fewer abortions and continue their pregnancies.
SEXUALLY TRANSMITTED INFECTIONS
60% of all sexually transmitted infections (STIs) are diagnosed in adolescents and youth despite making up only a quarter of the population.48 Even though there are known individual risk factors that affect their acquisition of sexually transmitted infections such as multiple sex partners, early sexual debut, lack of condom use, these factors are modeled by structural conditions in which adolescents and youth live and grow. Studies have demonstrated the role of schooling status, employment, migration, and social support in predicting risk and vulnerability to STIs in adolescent girls.49,50,51,52
Adolescents who do not use condoms at sexual debut are less likely to engage in subsequent protective behaviors and experience more infections; therefore, condom use at sexual debut is a good proxy for STI risk in adolescence.53 Condom use has a social gradient. In a country like Chile where only 7% of the adolescents that belong to the richest families attend private schools, condoms were used at sexual debut by 60% of adolescents enrolled in private schools and 37% of those enrolled in public schools.54 Condom use in adolescents is also affected by substantial gender disparities; females report less use than males.55 This phenomenon can be due to transgenerational sex, approximately 30% of adolescent women have sex with male partners who are three or more years older.54 Age difference creates a power differential and favors lack of perceived control over what occurs during the sexual encounter that puts girls at highest risk of coercion in the negotiation of condom and contraceptive use. Also, adolescent girls are often hesitant about buying and possessing condoms, concerned about the social stigma or disapproval by family.
Educational attainment, better grades, and not dropping out of school are also educational measures that improve condom use.52 This may happen because young individuals with stronger schooling may have higher aspirations in their lives, which may impact the perception of potential costs related to risky sexual behaviors.
Chlamydia trachomatis infection is the most frequently reported bacterial STI in sexually active adolescents with a prevalence between 5 to 15% of youth under 25 years old worldwide.56 Systematic reviews have shown a consistent association between socio-economic disadvantage and higher risk of C. trachomatis infections.57 College-level education is protective of C. trachomatis infections.58
Globally, young women represent more than 60% of all young people living with HIV.8 The HIV/AIDS epidemic in adolescents is reaching the poorest population strata. In Africa, where HIV/AIDS prevalence has a substantial heterogeneity across geographic areas and populations, adolescent girls are up to three times as likely to be living with HIV compared to their male counterparts. Moreover, in Ethiopia. highly vulnerable adolescent girls, characterized by extreme social and structural vulnerability with respect to schooling status, migration history, food insecurity, orphanhood, social support, and employment have twice the HIV/STI prevalence than other girls.59 In Brazil, higher HIV/AIDS prevalence is observed in the black population, particularly with lower educational level. In the last 10 years, there was a reduced detection rate of AIDS in the white population (21.9%) and an increased detection rate in the black population (35.7%), especially among women.60
To achieve STI epidemic control in adolescents, assessments of vulnerability that extend beyond measures of sexual risk may hold promise for altering their trajectories of risk earlier in their life cycle. From an intervention-development perspective, early identification of girls who may be at highest risk of STI acquisition and transmission, even in the absence of reported sexual activity, is essential to implement preventive interventions.
Examples of interventions based on SDH that improve condom use
- Mass media campaign and education on entertainment television programming.61,62
- Implementing a sexual and reproductive health/sexually transmitted infections curriculum in schools.63
- School-based condom availability programs.64
CONTRACEPTIVE USE
Socio-economic differences in sexual activity are often the indicator used to account for the inequality that exists in relation to adolescent’s sexual and reproductive health. For the purposes of this analysis, we posit that age of sexual debut is not as important as differences in contraceptive use in young women, given that the use of protection is what differentiates the future trajectories of young people more than whether they are sexually active. As the evidence shows, contraceptive use has invaluable social and health benefits for adolescent and young women worldwide and socio-economic and gender factors are associated with their use.65
There is substantial heterogeneity across and within countries. In low- and middle-income countries, only one-third of sexually active females aged 15 to 19 use contraceptive methods. In high-income countries, 50 to 70% of sexually active females use them.66
Adolescents mainly use short-acting methods, such as condoms and pills.67,68 National differences in condom and pill use among adolescents have been explained by contextual factors, such as economic stability, education, neighborhood, and built environment and employment, sexual education programs at schools, availability of adolescent health services, and quality and access to family planning services and supplies. Measures of inequality, such as the Human Development Index and Gini coefficient, as well as poverty and investments in education, are associated with contraceptive use, especially condoms.69,70
In the United States contraception services' use in adolescents is increasing but socio-economic disparities in their use are widening. Use of services is less among the socially disadvantaged, including girls who are foreign and lacking insurance coverage.71 The rise in contraceptive services is almost entirely due to an increase in contraceptive care received by adolescents visiting private doctors. The delivery of contraceptive services by other providers has remained unchanged.72 Less educated women are only a third as likely to use any form of contraception as those who have a college degree. In Chile, adolescents with low socio-economic status who use any type of contraception at first sexual intercourse is less (67%) than those with medium and high socio-economic status (74%). Urban adolescents who use any type of contraception at first sexual intercourse is higher (71%) than rural adolescents (67%).54
Racial disparities also impact adolescent contraceptive uptake, lower contraceptive use among black and Hispanic adolescents compared to white adolescents has been described, reflecting the vulnerability of women to poor reproductive health outcomes.73,74,75
Even though long active reversible (LARC) contraceptives are 20 times more effective, preventing adolescent pregnancy than other modern contraceptives, in the United States, 8% of 15- to 19-year-old adolescents report using LARCs, while 17% report using birth control pills.76 Speaking English as the primary language (versus Spanish) and having insurance coverage is associated with an increased likelihood for LARC use placement. Access to counseling to understand complex medical information and navigating the logistics of the healthcare system still place a barrier for vulnerable adolescents' LARC use.
Historically excluded populations that desire pregnancy have been victims of forced contraception. This type of coercion enforced by the state, government, or establishment has been unequally targeted to vulnerable girls.
There are socio-economic disparities in the use of reproductive healthcare services for preventive care and contraceptive use among adolescents and young women who live in a context of resource vulnerability. It is essential to recognize the nature and extent of these disparities and promote reproductive health policies aimed at addressing these social inequalities.
DISCUSSION/CONCLUSIONS
Through this chapter we have sought to show the impact that social determinants of health have on sexual and reproductive health of young women, and the situation of vulnerability that this entails for them. Our analyses show that structural factors such as national wealth, income inequality, and access to education are strong determinants of four adolescent sexual health outcomes, pregnancy, abortion, sexually transmitted infections, and contraceptive use.
The importance of recognizing social and structural factors, above and beyond individual risks, recognize that sexual behaviors exist amidst a complex fabric of other structural and individual factors that can potentiate vulnerability.
Interventions that provide adolescents with the economic and social support needed to meet their most basic needs may be most beneficial in supporting them to make better sexual and relationship choices.
The most effective interventions are probably structural changes to improve access to education. Education is a structural determinant that is modifiable and can clearly improve sexual health in adolescents.
Differentiating groups that have different vulnerabilities is important to tailor targeted prevention interventions. For example, interventions that empower girls to improve negotiation skills with their partners could reduce gender disparity in sexual health outcomes. For this, it is crucial that decision makers, health professionals, and communities commit to collective, intersectoral, and participatory work, going beyond the individual risk approach to achieve a broader and more comprehensive view of this problem.
PRACTICE RECOMENDATIONS
- When facing an adverse sexual health outcome always pay attention to the social determinants and how the social contexts, the conditions in which people are born, grow, and live, affect health.
- Health is shaped by communities, by the distribution of social position, gender, ethnicity, access to resources, at worldwide, national, and local levels.
- This perspective challenges the traditional epidemiologic approach, which seeks to identify individual risk factors of disease.
- Globally adolescent girls are vulnerable because social determinants disfavor and socially exclude them, particularly in developing countries.
- Adolescent pregnancy occurs in higher proportion in girls from developing countries, unsafe and impoverished environments with low levels of education and deficient access to healthcare.
- Where abortion is legal, vulnerable pregnant adolescents have more abortions. Where abortion is illegal, vulnerable pregnant adolescents have fewer abortions and continue their pregnancies to term compared to high socio-economic status pregnant adolescents who have more access to abortion under restricted legislations.
- Socio-economic disadvantage is associated with lower rates of condom use at sexual debut, a known proxy of sexually transmitted infection risk in adolescences, and with higher rates of HIV and C. trachomatis infection in adolescent girls.
- The use of contraceptive protection in adolescents is what differentiates their future trajectories more than whether they are sexually active or not. Contraceptive use is less in low- and middle-income countries with higher measures of inequality, in rural, low socio-economic status adolescents who are less educated, and in females.
- Effective interventions to reduce adolescent pregnancy, abortion, and sexually transmitted infections and to improve contraceptive use must provide social, economic, and educational support tailored to vulnerable adolescent girls.
CONFLICTS OF INTEREST
The author(s) of this chapter declare that they have no interests that conflict with the contents of the chapter.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Mead M. Coming of age in Samoa. William Morrow and Co, 1928. | |
M Marmot, Wilkinson R. Social Determinants of Health. Oxford University Press, 2005. | |
Trostle JA. Epidemiology and Culture [Internet]. Cambridge: Cambridge University Press, 2005 [cited 2022 Mar 29]. (Cambridge Studies in Medical Anthropology). Available from: https://www.cambridge.org/core/books/epidemiology-and-culture/3B5E21F9B970CAB57AEF1DA39BD8E68D. | |
Viner R, Ozer E, Denny S, et al. Adolescence and the social determinants of health. Lancet 2012;379:1641–52. | |
Horn A, Smith P, et al. Can social determinants of health influence the reproductive health of adolescents and young adult women. MOJ Women’s Health 2020;9(3):64–5. | |
Obach A, Sadler M, Jofré N. Sexual and reproductive health of adolescents in Chile: the role of sexual education. Rev Salud Pública 2017;19(6):848–54. | |
Obach A, Sadler M, Cabieses B. Intersectoral strategies between health and education for preventing adolescent pregnancy in Chile: Findings from a qualitative study. Health Expect 2019;22(2):183–92. | |
Chandra-Mouli V, Svanemyr J, Amin A, et al. Twenty Years After International Conference on Population and Development: Where Are We With Adolescent Sexual and Reproductive Health and Rights? Journal of Adolescent Health 2015;56:S1eS6. | |
World Health Organization. Adolescent pregnancy [Internet]. [cited 2022 April 30]. Available from: https://www.who.int/news-room/fact-sheets/detail/adolescent-pregnancy. | |
Maness S, Buhi E, Daley E, et al. Social Determinants of Health and Adolescent Pregnancy: An Analysis From the National Longitudinal Study of Adolescent to Adult Health. Journal of Adolescent Health 2016;58:636–43. | |
Decker MJ, Isquick S, Tilley L, et al. Neighborhoods matter. A systematic review of neighborhood characteristics and adolescent reproductive health outcomes. Health & Place 2018;54:178–90. | |
Drewry J, Garcés-Palacio IC. Socio-Demographic Characteristics and Female Empowerment as Determinants of Adolescent Pregnancy in Colombia. International Journal of Sexual Health 2020;32(3):293–305. | |
Gómez OSM, González KO. Fecundidad en adolescentes y desigualdades sociales en México, 2015. Rev Panam Salud Publica [Internet] 2018 [cited 2022 Jan 8];42. Available from: http://iris.paho.org/xmlui/handle/123456789/49168. | |
Béria JU, Schermann LB, Leal AF, et al. Motherhood in early adolescence: a case-control study in Southern Brazil. Ciênc Saúde Coletiva 2020;25(2):439–48. | |
Margherita G, Troisi G, Tessitore F, et al. Teen mothers who are daughters of teen mothers: Psychological intergenerational dimensions of early motherhood. Children and Youth Services Review 2017;83:294–301. | |
Pacheco-Sánchez CI. Embarazo en menores de quince años: los motivos y la redefinición del curso de vida. Salud Pública Mex 2016;58(2):56–61. | |
Aslalema A, Ortuño D, Merlyn MF. Adolescentes mujeres y jóvenes adultas frente a los temas de embarazo y aborto: ¿Percepciones diferentes según la edad? Estudio realizado en Quito, Ecuador (2017). Psicol Conoc Soc [Internet] 2019 [cited 2022 Jan 8];9(1). Available from: https://revista.psico.edu.uy/index.php/revpsicologia/article/view/551/379. | |
Doyenart M, Varela Petito C. Salteando etapas del curso de vida: Maternidad en la adolescencia. Cuad CLAEH [Internet] 2017 [cited 2022 Jan 8]; Available from: http://publicaciones.claeh.edu.uy/index.php/cclaeh/article/view/318. | |
Faisal-Cury A, Tabb K, Niciunovas G, et al. Lower education among low-income Brazilian adolescent females is associated with planned pregnancies. IJWH 2017;9:43–8. | |
de Vargas Nunes Coll C, Ewerling F, Hellwig F, et al. Contraception in adolescence: the influence of parity and marital status on contraceptive use in 73 low-and middle-income countries. Reprod Health 2019;16(1):21. | |
Hall KS, Richards JL, Harris KM. Social Disparities in the Relationship Between Depression and Unintended Pregnancy During Adolescence and Young Adulthood. Journal of Adolescent Health 2017;60(6):688–97. | |
Martinez-Saravia R, Alfaro A, Vaca A, et al. Depression and history of suicide attempts as risk factors for pregnancy in Bolivian adolescents. Acta Psiquiátr Psicol Am Lat 2021;(67(1)):5–15. | |
Mintogbé MM-M, Amadou Sanni M, Ahoussinou C, et al. First Early Pregnancy and Associated Factors Among Adolescent Girls in Benin. Sexuality & Culture 2021;25(1):117–39. | |
Menezes LMS, Vieira IS, Trindade LMD. Demographic-socioeconomic profile and sexual behavior of pregnant adolescents in a city in northeastern Brazil. Acta Sci Health Sci 2016;38(1):1. | |
Galvão R, Figueira C, Borovac-Pinheiro A, et al. Hazards of Repeat Pregnancy during Adolescence: A Case-control Study. Rev Bras Ginecol Obstet 2018;40(08):437–43. | |
Govender D, Naidoo S, Taylor M. Scoping review of risk factors of and interventions for adolescent repeat pregnancies: A public health perspective. Afr J Prim Health Care Fam Med [Internet] 2018 [cited 2022 Jan 9];10(1). Available from: https://phcfm.org/index.php/phcfm/article/view/1685. | |
Odii A, Atama CS, Igwe I, et al. Risky sexual behaviours among adolescent undergraduate students in Nigeria: does social context of early adolescence matter? Pan Afr Med J [Internet] 2020 [cited 2022 Jan 9];37. Available from: https://www.panafrican-med-journal.com/content/article/37/188/full. | |
Astuti AW, Kurniawati HF. The intersection between Health and Culture: A Qualitative Exploratory Study about Indonesian Adolescents’ Sexual Reproductive Health Services. P J M H S 2021;15(3):1147. | |
Ninsiima A, Leye E, Michielsen K, et al. “Girls Have More Challenges; They Need to Be Locked Up”: A Qualitative Study of Gender Norms and the Sexuality of Young Adolescents in Uganda. IJERPH 2018;15(2):193. | |
Flaviano M, Harville EW. Adverse Childhood Experiences on Reproductive Plans and Adolescent Pregnancy in the Gulf Resilience on Women’s Health Cohort. IJERPH 2020;18(1):165. | |
Miura PO, Tardivo LS de LPC, Barrientos DMS, et al. Adolescence, pregnancy and domestic violence: social conditions and life projects. Rev Bras Enferm 2020;73(suppl 1):e20190111. | |
McNiss C, Kalarchian M, Laurent J. Factors associated with childhood sexual abuse and adolescent pregnancy. Child Abuse & Neglect 2021;120:105183. | |
Aguía-Rojas K, Gallego-Ardila AD, Estrada Bonilla MV, Rodríguez-Niño JN. Individual and Contextual Factors Associated with Teenage Pregnancy in Colombia: A Multilevel Analysis. Matern Child Health J 2020;24(11):1376–86. | |
Laursen L, Hebert L, Newton S, et al. Community Violence Exposure and Adolescent Pregnancy in Chicago. J Interpers Violence 2022;37(1–2):NP742–56. | |
Turkay Ü, Aydın Ü, Çalışkan E, et al. Comparison of the pregnancy results between adolescent Syrian refugees and local adolescent Turkish citizens who gave birth in our clinic. The Journal of Maternal-Fetal & Neonatal Medicine 2018;1–6. | |
Govender D, Naidoo S, Taylor M. “My partner was not fond of using condoms and I was not on contraception”: understanding adolescent mothers’ perspectives of sexual risk behaviour in KwaZulu-Natal, South Africa. BMC Public Health 2020;20(1):366. | |
Rodriguez A. Adolescent pregnancy, public policies, and targeted programs in Latin America and the Caribbean: a systematic review, Rev Panam Salud Publica 2021;45:e144. | |
Winner B, Peipert J, Zhao Q, et al. Effectiveness of long-acting reversible contraception. N Engl J Med 2012;366(21):1998–2007. | |
Leppälahti S, Heikinheimo O, Paananen R, et al. Determinants of underage induced abortion – the 1987 Finnish Birth Cohort study. Acta Obstet Gynecol Scand 2016;95(5):572–9. | |
Rasch V, Gammeltoft T, Knudsen L, et al. Induced abortion in Denmark: Effect of socio-economic situation and country of birth. Eur J Public Health 2008;18:144. | |
Taft A, Powell R, Watson L. Factors associated with induced abortion over time: secondary data analysis of five waves of the Australian Longitudinal Study on Women’s Health. Aust N Z J Public Health 2019;43:137. | |
Jones R, Jerman J. Population group abortion rates and lifetime incidence of abortion: United States, 2008–2014. Am J Public Health 2017;107:1904. | |
Chae S, Desai S, Crowell M. Characteristics of women obtaining induced abortions in selected low- and middle-income countries. Plos One 2017;12:e017297. | |
Huneeus A, Capella D, Cabieses B, et al. Induced Abortion According to Socioeconomic Status in Chile. J Pediatr Adolesc Gynecol 2020;33(4):415–420.e1. | |
Gilanold G, Hailegebreal S. Determinants of abortion among youth 15–24 in Ethiopia: A multilevel analysis based on EDHS 2016. Plos One 2021. | |
CDC. Sexually Transmitted Infections Prevalence, Incidence, and Cost Estimates in the United States [Internet]. NCSD [cited 2022 Mar 29]. Available from: https://www.ncsddc.org/resource/sti-cost-estimates-us/. | |
De Neve J, Fink G, Subramanian S, et al. Length of secondary schooling and risk of HIV infection in Botswana: evidence from a natural experiment. The Lancet Global Health 2015;3(8):e470–e7. | |
Operario D, Underhill K, Chuong C, et al. HIV infection and sexual risk behaviour among youth who have experienced orphanhood: systematic review and meta-analysis. J Int AIDS Soc 2011;14:25. | |
Weine S, Kashuba A. Labor migration and HIV risk: a systematic review of the literature. AIDS Behav 2012;16(6):1605–21. | |
Hargreaves J, Bonell C, Boler T, et al. Systematic review exploring time trends in the association between educational attainment and risk of HIV infection in sub-Saharan Africa. AIDS 2008;22(3):403–14. | |
Shafii T, Stovel K, Holmes K. Association between condom use at sexual debut and subsequent sexual trajectories: A longitudinal study using biomarkers. Am J Public Health 2007;97:1090–5. | |
Huneeus A. Type of Primary Education Is Associated with Condom Use at Sexual Debut Among Chilean Adolescents. Sexuality Transmited Diseases 2014;41(5). | |
Feldman BS, Shtarkshall RA, Ankol OE, et al. Diminishing Gender Differences in Condom Use Among a National Sample of Young Israeli Men and Women Between 1993 and 2005. Journal of Adolescent Health 2012;50:311–4. | |
Gottlieb SL, Xu F, Brunham RC. Screening and Treating Chlamydia trachomatis Genital Infection to Prevent Pelvic Inflammatory Disease. Sex Transm Dis 2013;1. | |
Crichton J, Hickman M, Campbell R, et al. Socioeconomic factors and other sources of variation in the prevalence of genital chlamydia infections: A systematic review and meta-analysis. BMC Public Health 2015;15(1):729. | |
Huneeus A, Schilling A, Fernandez MI. Prevalence of Chlamydia Trachomatis, Neisseria Gonorrhoeae, and Trichomonas Vaginalis Infection in Chilean Adolescents and Young Adults. J Pediatr Adolesc Gynecol 2018;31(4):411–5. | |
Comins CA, Rucinski KB, Baral S, et al. Vulnerability profiles and prevalence of HIV and other sexually transmitted infections among adolescent girls and young women in Ethiopia: A latent class analysis. PLoS One 2020;15(5):e0232598. | |
Taquette SR, Rodrigues NCP. Human immunodeficiency virus/acquired immunodeficiency syndrome epidemic in adolescents from a Brazilian metropolis (1978–2017). Rev Soc Bras Med Trop 53:e20190193. | |
Kelly K, Parker W, Hajiyiannis H, et al. Tsha Tsha: Key findings of the evaluation of episodes 1–26. Johannesburg, South Africa: Centre for AIDS Development, Research and Evaluation; 2005 accessed at https://www.comminit.com/content/tsha-tsha-key-findings-evaluation-episodes-1-26 on April 30, 2022. | |
Plautz A, Meekers D. Evaluation of the reach and impact of the 100% Jeune youth social marketing program in Cameroon: Findings from three crosssectional surveys. Reprod Health 2007;4:1. | |
Jemmott JB 3rd, Jemmott LS, O’Leary A, et al. School-based randomized controlled trial of an HIV/STD risk-reduction intervention for South African adolescents. Arch Pediatr Adolesc Med 2010;164:923e9. | |
Wang T, Lurie M, Govidasamy D, et al. The Effects of School-Based Condom Availability Programs (CAPs) on Condom Acquisition, Use and Sexual Behavior: A Systematic Review. AIDS Behav 2018;22(1):308–320. | |
Family Planning 2030. About Us [Internet] 2018 [cited 2022 Mar 29]. Available from: https://fp2030.org/about-us. | |
Kalamar A, Tuncalp Ö, Hindin M. Developing strategies to address contraceptive needs of adolescents: exploring patterns of use among sexually active adolescents in 46 low- and middle-income countries. Contraception 2018;98(1):36–40. | |
Looze M, Madkour A, Hujits T, et al. Country-Level gender equality and adolescents’ contraceptive use in Europe, Canada and Israel: fndings from 33 countries. Perspect Sex Reprod Health 2019;51(1):43–53. | |
Darroch J, Woog V, Bankole A, et al. Adding it up: costs and benefits of meeting the contraceptive needs of adolescents. [Internet]. New York: Guttmacher Institute, 2016. Available from: https://www.guttmacher.org/report/adding-it-meeting-contraceptive-needs-of-adolescents. [Ref list]. | |
Lazarus J, Moghaddassi M, Godeau E, et al. A multilevel analysis of condom use among adolescents in the European Union. Public Health 2009;123(2):138–44. | |
Benefo K. Determinants of condom use in Zambia: a multilevel analysis. Std Fsm Plann 2010;41(1):19–30. | |
Potter J, Trussell J, Moreau C. Trends and determinants of reproductive health service use among young women in the USA. Hum Reprod 2009;24(12):3010–8. | |
Frost J. Trends in women’s use of sexual and reproductive health care services, 1995–2002. AJPH 2008;98:1814–7. | |
Maness S, Thompson E, Yu Lu. Associations Between Social Determinants of Health and Adolescent Contraceptive Use: An Analysis From the National Survey of Family Growth. Fam Communitu Health 2022;45(2):91–102. | |
Witwer E, Jones R, Lindberg L. Sexual behavior and contraceptive and condom use among U.S. high school students, 2013–2017. New York: Guttmacher Institute, 2018. | |
Borges ALV, Duarte LS, Lay AAR, et al. Individual and context correlates of the oral pill and condom use among Brazilian female adolescents. BMC Womens Health 2021;21:307. | |
Tomlin K, Bambulas T, Sutton M, et al. Motivational interviewing to promote long-acting reversible contraception in postpartum adolescentrs. Journal of Pediatric and Adolescent Gynecology 2017;30(3):383–8. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards program CLICK HERE)
