This chapter should be cited as follows:
Frawley H, Peterson K, Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.418263
The Continuous Textbook of Women’s Medicine Series – Gynecology Module
Volume 3
Endometriosis
Volume Editors:
Professor Andrew Horne, University of Edinburgh, UK
Dr Lucy Whitaker, University of Edinburgh, UK
Chapter
Physiotherapy for Endometriosis
First published: September 2022
Study Assessment Option
By answering four multiple-choice questions (randomly selected) after studying this chapter, readers can qualify for Continuing Professional Development points plus a Study Completion Certificate from GLOWM.
See end of chapter for details.
INTRODUCTION
Why is this important?
International guidelines currently recommend surgical or pharmacological interventions as first-line treatments for endometriosis;1,2 however, for 20–40% of women, symptoms persist following surgical and pharmacological treatment.3 Furthermore, the extent of endometriosis lesions is known not to correlate well with the woman’s pain,4 and recurrent symptoms do not necessarily correlate with recurrent lesions.5 Alternative ways of managing pain are needed, which need to take into account contemporary pain science and all biopsychosocial aspects of the persistent pain experience. Evidence for conservative therapies in pain management and subsequent impact on function and quality of life in women seeking care for endometriosis-associated pain is limited, but emerging. In this chapter we explore the mechanisms and evidence for physiotherapy management of pelvic pain associated with endometriosis. Physiotherapists provide conservative therapies and as a discipline are increasingly recommended as part of the multidisciplinary team when managing endometriosis-associated pelvic pain.5,6,7,8,9
Clinicians need to consider the underlying mechanisms and patient expectations in the context of the available multidisciplinary health-care provision to ensure that women are given a choice in treatment options based on fully informed consent. As identified by Vincent and Evans,10 viewing endometriosis-associated pain within the new IASP chronic pain classification framework11 allows us to consider the primary and secondary nature of endometriosis-associated pain, and its presentation across visceral and musculo-skeletal domains, as illustrated in Figure 1.
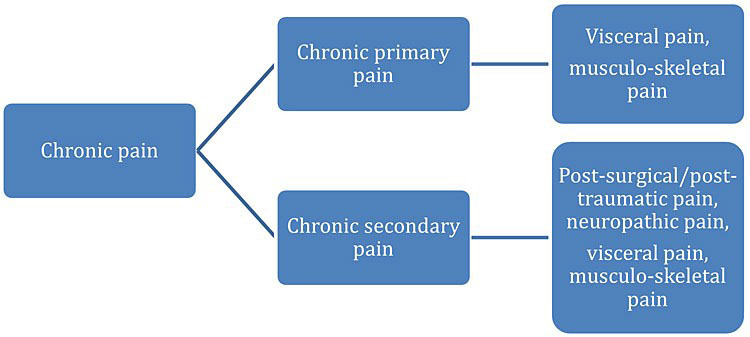
1
Endometriosis viewed as a chronic primary or chronic secondary pain condition (modified from Treede et al. 2019).11
Endometriosis-associated pain and the mechanisms responsible for its initiation and persistence are complex.12 While local tissue disease factors have been the main focus of past investigation and are relatively well – although not completely – understood,5 it is also known that macroscopic tissue disease is poorly correlated with pain symptoms.13 More recently, an appreciation of the complexity of peripheral, central, and cross-sensitization in endometriosis-associated pain and comorbid pain syndromes (bladder pain syndrome, irritable bowel syndrome, abdomino-pelvic myalgia, and vulvodynia) in the persistence of endometriosis-associated pain has emerged.12,14 Visceral structures (uterus, bowel, and bladder) and somatic structures (skin, muscles, fascia, and bones) in the pelvis share neural pathways resulting in similar symptoms and making it difficult to differentiate somatic from visceral causes of pain.14 These viscero–viscero cross-sensitization and viscero–somatic convergence pathways are illustrated in Figure 2 below.
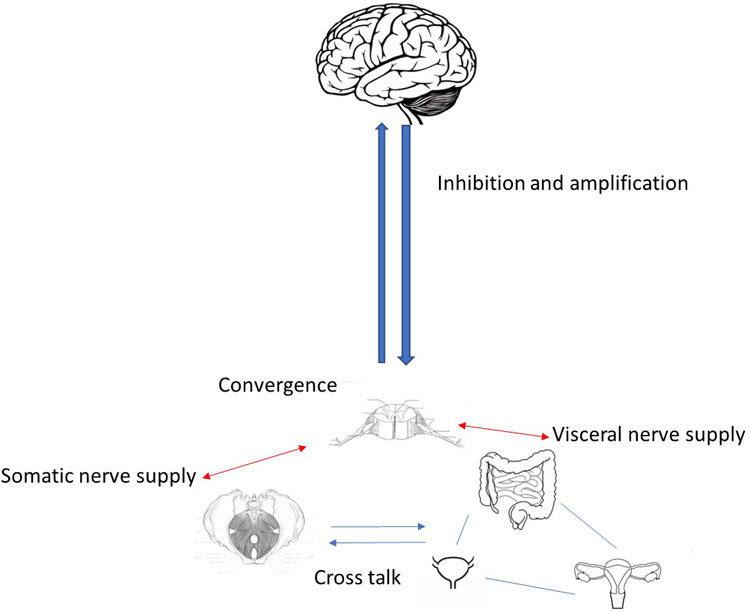
2
Visceral and somatic convergence pathways.
Hopefully awareness of the complexity of pain presentation and the pain experience of sufferers will assist clinicians to embrace evidence-based multidisciplinary care and consider conservative therapies where these have been found beneficial.
RATIONALE FOR PHYSIOTHERAPY MANAGEMENT OF ENDOMETRIOSIS-ASSOCIATED PELVIC PAIN
Physiotherapists increasingly utilize contemporary pain science to inform their management of persistent pain conditions, which involves shifting clinical reasoning and research focus from solely looking at pain from tissue damage to considering the science of pain itself.15
Clinical application of pain science has important implications for clinicians and for how clinicians explain and manage pain in patients with endometriosis. There are many mechanisms by which endometriosis-associated pain can be amplified or reduced.9 Reduction may be affected by activation of descending inhibition generated by central processes; however, it is difficult to demonstrate the translation of the theory into clinical practice. It remains unclear exactly how descending inhibition works, but manual therapy and exercise have been demonstrated to elicit these mechanisms.16,17 Various forms of therapeutic touch and placebo can mediate pain inhibition via different mechanisms, although these may be treatment dependent16 and individualized care should focus on helping the patient to identify modifiable factors as well as strategies to manage non-modifiable factors.9 Pain is a dynamic state regardless of the underlying condition as there are multiple factors that contribute to the pain experience.18 It can be helpful for patients with endometriosis-associated pain to understand that lesions and hormones are not the sole factors that need addressing in manage pain, and fluctuations in pain can be caused by physiological, behavioral, cognitive, attention, and social factors.19 Neural plasticity refers to changes in the nervous system such as learning and reorganization;20 this can be a helpful concept to give patients hope, that even if the pathology cannot be changed, the nervous system can. Biological and psychosocial factors have been identified as predisposing, precipitating, and perpetuating contributing factors in pelvic pain.10 This underpins the need for a biopsychosocial approach to address these contributing factors that impact on the well-being, function, and quality of life of a person with endometriosis-associated pain. Physiotherapists help people maximize their function and quality of life affected by injury, disease, or disability,21,22 using strategies to address physical, psychological, emotional, and social well-being within a biopsychosocial framework. A physiotherapist may collaborate in treatment as part of a larger multidisciplinary team, either co-located or independently, depending on the health system and availability of physiotherapists in the locality.
A respectful and strong therapeutic alliance between the patient and clinician contributes significantly to the therapeutic response.23 Treatment techniques will include pain education, to help the patient make sense of the underlying pain mechanisms; this can make a substantial difference to the patient to understand the nature of their pain and reduce the threat of the experience.24 As most patients with endometriosis-associated pain present to a physiotherapist with long-standing pain, it is important for the patient to understand that pain perceived to be in visceral or musculo-skeletal structures is not necessarily a sign that those structures are causing further disease or tissue damage.25 It is equally important to discuss realistic expectations especially if the patient is looking for complete pain resolution as persistent pain is difficult to treat, and medical treatments (pharmacological and non-pharmacological) have limited benefit in chronic pain conditions.26 Consultations with a physiotherapist may help the patient to shift their understanding of their condition away from purely a disease-centric and mechanical model, and help patients live well with a long-term condition.
As many of the pain symptoms and co-existing disorders associated with endometriosis are pelvic, pelvic health physiotherapists have a role to play in pain management, with their training in gynecological, urological, and gastroenterological conditions, including pelvic floor dysfunction and persistent pelvic pain.27,28 Recently, it has been proposed that endometriosis is a systemic disease rather than a disease predominantly affecting the pelvis,29 therefore it is important that a holistic approach to management is taken, avoiding an ‘end-organ’ focus.
Physiotherapists with training in both abdomino-pelvic and general musculoskeletal disorders, as well as persistent pain management, are ideally placed to contribute to the multidisciplinary team approach. It is important that sufficient resources and support are prioritized to enable researchers and clinicians, together with consumers, to continue expanding the current evidence base of physiotherapy treatment to help women with endometriosis.
EVIDENCE-BASED APPROACHES
Current clinical practice guidelines provide minimal guidance for physiotherapy care of a person with endometriosis,1,2 as evidence has emerged in recent years and is yet to be integrated into published pathways of care. Guidelines for management of pelvic pain – not specific to endometriosis-associated pelvic pain – may be suitable to be adopted, following a comprehensive history, careful assessment of the patient’s presenting symptoms, clinical signs, and results of investigations. It is important that the clinician adopts an evidence-based practice approach30 to guide diagnostic decision-making and clinical expertise in this emerging area of physiotherapy practice.
- Clinical state and circumstances.
- Symptoms: most commonly presenting symptoms related to endometriosis are pain before and during periods, pain during or after sexual activity, fatigue, infertility and heavy bleeding, painful bowel movements, painful urination, diarrhea and/or constipation and other intestinal symptoms during menstruation. The patient may perceive these symptoms to be in the abdomino-pelvic, pelvic floor, perineal or low back region, or a combination of these. The pain may be constant, intermittent, or provoked and the severity may fluctuate hourly, daily, or monthly and not necessarily correlate to the disease or hormonal state. A patient is likely to report significant impact on function and quality of life.31,32 The patient may also report or demonstrate depressed mood, anxiety, pain catastrophizing, pain anticipation, and increased attention to pain, which are all associated with higher reported pain intensity.6,33,34
- Signs: a musculo-skeletally trained physiotherapist will make a clinical judgement and decide with the patient what to focus on in a physical assessment. This could include back/spine, abdominal, pelvic floor, and perineal areas, as indicated by the patient’s symptoms and any findings from investigations/past treatment. From observational studies that have compared clinical findings in women with versus women without endometriosis-associated pain, there appears to be a pattern of pelvic floor muscle dysfunction including increased tenderness to digital palpation and increased pressure-pain thresholds, and increased pelvic floor muscle tone and decreased pelvic floor muscle relaxation ability35,36,37,38,39,40 present in symptomatic women.
- Outcome measures: excellent guidance is available from recent publications on core outcome sets and pain outcome measures. In women with endometriosis, Duffy et al.41 recommend measuring overall pain, the most troublesome symptom, and quality of life. In females with idiopathic chronic pelvic pain, Ghai et al.42 recommend measuring life impact (quality of life, emotional functioning, physical functioning), pain (pelvic pain, dyspareunia, dysmenorrhea) and effectiveness of clinical care using measures of efficacy, satisfaction, cost effectiveness and return to daily activities, and any adverse events associated with care. The IASP guidance on pain outcome measures is comprehensive: recommendations include measures of pain intensity ('how much does it hurt?'), pain-related distress ('how distressed are you by the pain?'), pain-related interference ('how much does the pain interfere with your life?'), rated by the patient on a 0–10 numerical rating scale then transformed into severity stages of 'mild,' 'moderate,' and 'severe,' as well as temporal characteristics (code as continuous, episodic recurrent, and continuous pain with pain attacks) and presence of psychosocial factors, i.e., problematic cognitive (e.g., catastrophizing, excessive worry), emotional (e.g., fear, anger), behavioral (e.g., avoidance), and/or social factors (e.g., work, relationships) that accompany the pain.11
The physiotherapist will integrate findings from the assessment, including history, symptoms, signs from clinical examination and results of investigations, to reach a diagnosis of the patient’s condition. While the diagnosis of endometriosis-associated pain may have been known at the start of the consultation, the comprehensive assessment will highlight what is important to the patient to achieve from physiotherapy care in order to improve the patient’s quality of life, as well as identify any problems that require onward referrals. The assessment will inform a patient-centered discussion about findings, goals, and treatment options. As patients with endometriosis-associated pain often have other pelvic comorbidities as well as psychosocial distress, the assessment may reveal other specific disorders that require attention in physiotherapy treatment, such as bladder urgency, low tolerance to exercises, low self-efficacy, fear avoidance, depression, etc.
- Research evidence: The current evidence from systematic reviews specific to endometriosis-associated pain is limited and much more research is needed. There are a number of conservative therapy approaches that a physiotherapist might use. Below is an overview of the interventions that have been investigated and are likely to fall under the physiotherapy competency frameworks; however, this is far from exclusive, as many physiotherapy interventions considered best practice, including multimodality interventions have not yet been investigated in clinical trials.
- Systematic review evidence, specific to endometriosis-associated pain, includes the following:
- The impact of exercise on pain perception in women with endometriosis has been recently reviewed, with only two randomized controlled trials included in this synthesis, indicating no evidence of benefit on pain.43
- Psychological and mind-body therapies (including yoga) appear promising to treat endometriosis-related pain, anxiety and depressive symptoms, stress, fatigue, with three randomized controlled trials included in this review.44
- Complementary therapies (defined in this review as acupuncture, exercise, electrotherapy, and yoga) were reviewed by Mira et al.,45 with effectiveness for pain relief found only from acupuncture, from four randomized controlled trials.
- Additional randomized controlled trials indicate some benefit from therapies directed to the pelvic area:
- Improved superficial dyspareunia, chronic pelvic pain, and pelvic floor muscle relaxation (increased levator hiatus area on Valsalva maneuver) in women with deep infiltrating endometriosis, following pelvic floor physiotherapy.40
- Reduction of pelvic pain and deep dyspareunia and improved quality of life and sexual function in women with deep infiltrative endometriosis following transcutaneous electrical stimulation applied to the parasacral region (S3-S4).46
- Reduction in pain intensity and present relief scores in women with endometriosis following pulsed high-intensity laser therapy.47 Randomized controlled trial evidence for physiotherapy treatments to reduce pelvic pain specifically in individuals with endometriosis is limited. Therefore, clinicians may cautiously be guided by evidence from systematic reviews of conservative therapy treatment effectiveness in women with persistent pelvic pain.48,49,50,51,52,53,54,55,56 This is a reasonable approach, given that many of these reviews included cohorts who had previously received a diagnosis for endometriosis, and because physiotherapy practice embraces the WHO International Classification of Functioning, Disability and Health57 approach, rather than a disease-specific model of care.
- Systematic review evidence, specific to endometriosis-associated pain, includes the following:
- Patient’s preferences and actions: the James Lind Alliance Priority Setting Partnership questions for future endometriosis research58 reflects the perspectives of what is important to patients in the management of their condition, including two priorities in the top ten listed priorities, which are relevant to physiotherapy care:
- What is the most effective way of managing the emotional impact and/or psychological and/or fatigue impact of living with endometriosis (including medical, non-medical, and self-management methods)?
- What are the most effective non-surgical ways of managing endometriosis-related pain and/or symptoms (medical/nonmedical)?
- Once further research is available to confirm the effectiveness of conservative therapies to treat pain, function, and quality of life in patients with endometriosis-associated pain, these data can be presented to patients to assist in their decision-making for preferred treatments. While many patients may prefer minimal intervention from health professionals, it is important to recognize the limitations of self‑management strategies in women with endometriosis, which currently do not have supporting evidence.59
- Treatment planning. The clinician will integrate the evidence gathered from the history, symptoms, signs, results of investigations, and likely diagnosis(es), and together with his/her knowledge of the clinical state and circumstances, findings from research, and the patient’s preferences for treatment, form a treatment plan that is patient-centered and collaborative. Similar to other persistent pelvic pain conditions,60 phenotypes may exist in patients who present with pelvic pain, with varying predominance of central and peripheral factors.61,62 Adjusting treatment to the particular phenotypic pattern or combination of factors may improve treatment outcomes.61 With limited evidence from endometriosis-specific studies, the clinician may be guided by evidence from high-quality trials of conservative therapies in women with persistent pelvic pain. The clinician needs to maintain an up-to-date knowledge of emerging evidence in this field in order to maximize health outcomes in patients with endometriosis-associated pain.
The approaches and clinical skills used by a physiotherapist will vary depending on their own training and specialization, what is supported by research, and the skill sets of other clinicians they work with or refer to. Some physiotherapists will work in large multidisciplinary settings; others will work in smaller individual clinics. Figure 3 illustrates approaches and clinical skills a physiotherapist may use when managing a patient with endometriosis-associated pain.
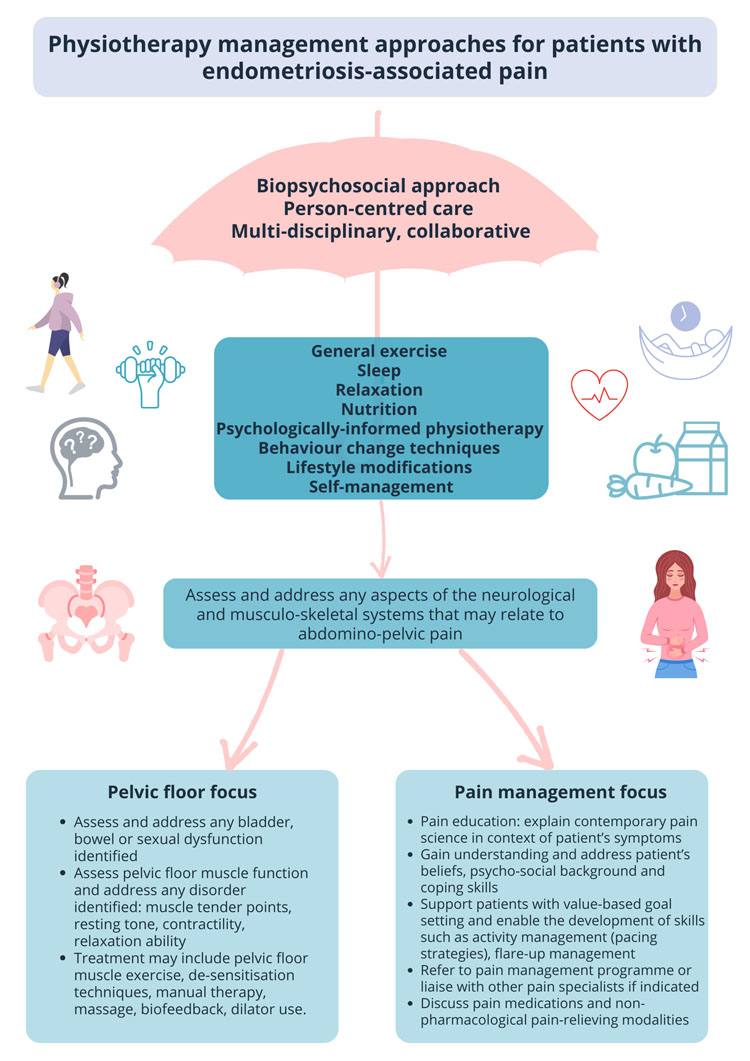
3
Approaches and clinical skills used by a physiotherapist.
CASE STUDY
The following case study demonstrates the approaches and clinical skills used by physiotherapists in the management of a patient with endometriosis-associated pain.
Ms A was a 27-year-old woman who was referred to pelvic health physiotherapy with a diagnosis of endometriosis. She presented with a history of pelvic pain and abdominal cramps from onset of menarche aged 12. She described the pain as 'awful,' necessitating time off school. She also explained that she received little support and was told it was normal period pains. In her late teenage years, she found sexual activity painful and she developed urinary urgency. Her GP reported her pelvic examination as normal and told her she had anxiety. She started using a contraceptive pill, which helped reduce the pain levels around her periods the first couple of years, but she found that she would experience unexplained and fluctuating pain levels independent of the time of month. Her urinary urgency was worsening to the point that she was finding it increasingly difficult to plan her day without knowing where the nearest toilet was. She was avoiding relationships as she feared that she could not have a normal sexual relationship.
At the age of 22, the pain was so severe that she had dropped out of university and had moved back home to obtain support from her parents. Her GP referred her to the local gynecology department and she underwent her first laparoscopy confirming the diagnosis of endometriosis. She was treated with excision and reported good pain relief. However, her symptoms recurred and were exacerbated 6 months after surgery. At her follow-up, she was told to try using a levonorgestrel-releasing intrauterine system (IUS). This did provide some relief and she managed to start a job in an office. She explained that she felt misunderstood by her colleagues who did not seem to understand the nature and impact of her pain, and she was taking more and more time off work with flare-ups. Aged 25 she was offered another laparoscopy as some recurrent lesions were detected on an MRI. She went ahead and underwent minor excision, which again helped for around 6 months before her symptoms recurred. She was subsequently referred to a specialist multidisciplinary endometriosis center and underwent her third laparoscopy. This did not provide any relief and she declined any further surgical interventions. She did feel the IUS was providing some relief and asked if there was anything else she could be offered.
Ms A agreed to be referred to a pelvic health physiotherapist and was keen to see if there were any non-invasive treatments that might help.
Ms A was trying to get on with her life but struggled with the following:
- Sexual dysfunction (dyspareunia);
- Urinary urgency;
- Widespread pain increasing throughout the day affecting ability to exercise;
- Flare-ups of pain, both cyclical and non-cyclical;
- Anxiety;
- Fatigue.
Ms A was seen by a pelvic health physiotherapist 12 years after her first symptoms.
The physiotherapist took time to listen to her story and the impact this had had on her life. It was clear that Ms A’s understanding of her pain aligned with a very biomedical model of pain and she was fearful that the pain she was experiencing meant that there was further harm occurring in her pelvis. Ms A agreed to be examined and together with the physiotherapist, she learned that her pelvic floor was very tense and tender to touch.
The initial plan was agreed with Ms A:
- Pain education;
- Pelvic floor relaxation exercises;
- Breathing;
- Goal setting.
Ms A returned for a follow-up and explained that she felt it was the first time someone had given her hope that her pelvis could function normally. She also reported that she was pleased to be able to talk about sensitive issues such as bowel, bladder, and sexual function. She was keen to access further group support as she felt speaking to other women with similar issues would help.
Ms A was also taught how to reduce her urinary urgency/sensitivity by using breathing techniques and distractions; this allowed her bladder to fill a little more each week before she went to the toilet. This was underpinned by good pain education so Ms A could make sense of her symptoms, understand that she could have severe symptoms without recurrence of her disease and understand how she could manage.
Over the next 7 weeks Ms A attended two more follow-ups. She improved her urinary urgency, learned strategies to relax her pelvic floor muscles, was introduced to dilators to reduce the sensitivity in her vaginal tissues to enable coital function and was more able to go out.
Nevertheless, she was still worried about intimate relationships, managing her job, and her body image as she was struggling to exercise. She recognized that it might be helpful to ask her GP for some additional psychological support, which she was not open to initially.
Throughout the physiotherapy treatment, Ms A gained a broader understanding of pain mechanisms and the multiple factors affecting her pain. Ms A practised exercising in a paced way to build up her exercise tolerance, and slowly regained her confidence. The physiotherapist introduced Ms A to the ReConnect model,63 which uses psychosexual counseling and pain management, desensitization approaches, and a graded approach to explore intimacy. Ms A wrote down a flare-up plan, which included heat, use of a TENS machine, pacing herself, communication skills to gain confidence in explaining her needs, stretches, pelvic floor muscle relaxation, breathing techniques, and learned to identify symptoms that she could self-manage and symptoms that may require a medical review.
Ms A attended six sessions over 15 weeks and completed a battery of outcome measure before and after the physiotherapy episode of care. She described much improved confidence in relationships, ability to exercise and manage her flare-ups by communicating with her colleagues. Her mood was slowly improving, she explained that she understood that she was on a journey learning to accept and manage a long-term painful condition, but she had hope and goals that she felt would be achievable.
This case demonstrates that Ms A befitted from the physiotherapy support to develop her own self-management skills, which improved her quality of life. Endometriosis-associated pain and pelvic floor dysfunction can be addressed in a helpful way even if complete pain relief cannot be achieved. Patients may need to be in the right place in their medical journey and understanding of their symptoms to be able to engage fully in the advice and treatment. At the same time, these strategies should be introduced early to support patient choice. The case also highlights that patients report benefits from meeting other people with similar problems, group support as well as psychological interventions.
In the context of this chapter, this case study focusses on physiotherapy-only strategies. However, multidisciplinary centers for pelvic pain that include pain management programs for pelvic pain do exist in some locations; in these settings, knowledge and care can be shared by a range of members of the multidisciplinary team to the benefit of the patient with complex and persistent pelvic pain.
SUMMARY
In summary, physiotherapists have an emerging and increasingly evidence-based role in the management of endometriosis-associated pain. Physiotherapists provide a range of conservative therapies, which are generally low cost and low risk, and utilize a biopsychosocial approach to care. Multidisciplinary teams providing care for patients with endometriosis-associated pain may benefit from the addition of a physiotherapist to the team. Much more research is needed to support the effectiveness of conservative therapies in the management of endometriosis-associated pain, with focus required on those patients likely to benefit most from conservative therapies.
PRACTICE RECOMMENDATIONS
- All clinicians should ask about the patient’s understanding of their pain and provide pain education.
- Pelvic health physiotherapists should assess the patient’s physical functioning and ask about sexual activity, bowel, and bladder function.
- Ensure patients are assessed holistically, the symptoms of endometriosis are not heterogenous and are influenced by a multitude of factors.
- Recognize that a patient’s coping mechanisms may be strongly related to psychosocial factors.
- Discuss alternative options to surgery and medication and explore the patient’s preferences and goals.
- Physiotherapists are well placed to discuss options to improve quality of life where medical approaches are not the preferred option, or the patient wishes to try alternatives.
CONFLICTS OF INTEREST
The author(s) of this chapter declare that they have no interests that conflict with the contents of the chapter.
Feedback
Publishers’ note: We are constantly trying to update and enhance chapters in this Series. So if you have any constructive comments about this chapter please provide them to us by selecting the "Your Feedback" link in the left-hand column.
REFERENCES
Kuznetsov L, et al. Diagnosis and management of endometriosis: summary of NICE guidance. BMJ 2017;358:j3935. | |
Dunselman GA, et al. ESHRE guideline: management of women with endometriosis. Hum Reprod 2014;29(3):400–12. | |
Vercellini P, et al. The effect of surgery for symptomatic endometriosis: the other side of the story. Hum Reprod Update 2009;15(2):177–88. | |
Masciullo L, et al. A deep insight into pelvic pain and endometriosis: a review of the literature from pathophysiology to clinical expressions. Minerva Obstet Gynecol 2021;73(5):511–22. | |
As-Sanie S, et al. Assessing research gaps and unmet needs in endometriosis. Am J Obstet Gynecol 2019;221(2):86–94. | |
Allaire C, et al. An interdisciplinary approach to endometriosis-associated persistent pelvic pain. Journal of Endometriosis and Pelvic Pain Disorders 2017;9(2):77–86. | |
Allaire C, et al. Interdisciplinary Teams in Endometriosis Care. Semin Reprod Med 2020;38(2–03):227–34. | |
Allaire C, et al. Chronic pelvic pain in an interdisciplinary setting: 1-year prospective cohort. Am J Obstet Gynecol 2018;218(1):114.e1–12. | |
Coxon L, Home AW, Vincent K. Pathophysiology of endometriosis-associated pain: A review of pelvic and central nervous system mechanisms. Best Practice & Research Clinical Obstetrics & Gynaecology 2018;51:53–67. | |
Vincent, K. and E. Evans, An update on the management of chronic pelvic pain in women. Anaesthesia 2021;76(Suppl 4):96–107. | |
Treede RD, et al. Chronic pain as a symptom or a disease: the IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019;160(1):19–27. | |
McNamara HC, et al. Peripheral, Central, and Cross Sensitization in Endometriosis-Associated Pain and Comorbid Pain Syndromes. Frontiers in Reproductive Health 2021;3(56). | |
Schliep KC, et al. Pain typology and incident endometriosis. Hum Reprod 2015;30(10):2427–38. | |
Lamvu G, et al. Chronic Pelvic Pain in Women: A Review. JAMA 2021;325(23):2381–91. | |
Parker R, Madden VJ. State of the art: What have the pain sciences brought to physiotherapy? S Afr J Physiother 2020;76(1):1390. | |
Vigotsky AD, Bruhns RP. The Role of Descending Modulation in Manual Therapy and Its Analgesic Implications: A Narrative Review. Pain Res Treat 2015:292805. | |
Munneke W, Ickmans K, Voogt L. The Association of Psychosocial Factors and Exercise-Induced Hypoalgesia in Healthy People and People With Musculoskeletal Pain: A Systematic Review. Pain Pract 2020;20(6):676–94. | |
Arendt-Nielsen L, et al. Assessment and manifestation of central sensitisation across different chronic pain conditions. Eur J Pain 2018;22(2):216–41. | |
Adams, L.M. and D.C. Turk, Psychosocial factors and central sensitivity syndromes. Curr Rheumatol Rev 2015;11(2):96–108. | |
Bak MS, Park H, Kim SK. Neural Plasticity in the Brain during Neuropathic Pain. Biomedicines 2021;9(6). | |
WCPT. World Confederation for Physical Therapy. https://world.physio/resources/what-is-physiotherapy. | |
CSP. https://www.csp.org.uk/careers-jobs/what-physiotherapy. | |
Denneny D, et al. The application of psychologically informed practice: observations of experienced physiotherapists working with people with chronic pain. Physiotherapy 2020;106:163–73. | |
Moseley GL. Whole of community pain education for back pain. Why does first-line care get almost no attention and what exactly are we waiting for? Br J Sports Med 2019;53(10):588–9. | |
Petersen K. A review of the physiotherapy pain management strategies in the management of patients with chronic pelvic pain. 2015. | |
NICE, National Institute for Health and Care Excellence: Guidelines, in Chronic pain (primary and secondary) in over 16s: assessment of all chronic pain and management of chronic primary pain. National Institute for Health and Care Excellence (NICE) Copyright © NICE 2021.: London, 2021. | |
Frawley HC, Morin M. Chronic pelvic floor pain, in Evidence based physical therapy for the pelvic floor: bridging science and clinical practice. In Bø K, et al. (eds.) accepted 27Jan2021, Elsevier: London, 2022. | |
Frawley HC, Neumann P, Delany C. An argument for competency-based training in pelvic floor physiotherapy practice. Physiotherapy Theory and Practice 2019;35(12):1117–30. | |
Taylor HS, Kotlyar AM, Flores VA. Endometriosis is a chronic systemic disease: clinical challenges and novel innovations. Lancet 2021;397(10276):839–52. | |
Haynes RB, Devereaux PJ, Guyatt GH. Clinical expertise in the era of evidence-based medicine and patient choice. Evidence-Based Medicine 2002;7(2):36–8. | |
Armour M, et al. Endometriosis and chronic pelvic pain have similar impact on women, but time to diagnosis is decreasing: an Australian survey. Sci Rep 2020;10(1):16253. | |
Comptour A, et al. Long-Term Evolution of Quality of Life and Symptoms Following Surgical Treatment for Endometriosis: Different Trajectories for Which Patients? J Clin Med 2020;9(8). | |
Gao M, et al. Psychiatric comorbidity among women with endometriosis: nationwide cohort study in Sweden. Am J Obstet Gynecol 2020;223(3):415.e1–16. | |
McPeak AE, et al. Pain Catastrophizing and Pain Health-Related Quality-of-Life in Endometriosis. Clin J Pain 2018;34(4):349–56. | |
Dos Bispo AP, et al. Assessment of pelvic floor muscles in women with deep endometriosis. Arch Gynecol Obstet 2016;294(3):519–23. | |
Fraga MV, et al. Pelvic floor muscle dysfunctions in women with deep infiltrative endometriosis: An underestimated association. Int J Clin Pract 2021;75(8):e14350. | |
Raimondo D, et al. Pelvic floor muscle dysfunction on 3D/4D transperineal ultrasound in patients with deep infiltrating endometriosis: a pilot study. Ultrasound Obstet Gynecol 2017;50(4):527–32. | |
Mabrouk M, et al. Painful Love: Superficial Dyspareunia and Three Dimensional Transperineal Ultrasound Evaluation of Pelvic Floor Muscle in Women with Endometriosis. J Sex Marital Ther 2020;46(2):187–96. | |
Del Forno S, et al. Transperineal Ultrasound Visual Feedback Assisted Pelvic Floor Muscle Physiotherapy in Women With Deep Infiltrating Endometriosis and Dyspareunia: A Pilot Study. J Sex Marital Ther 2020;46(7):603–11. | |
Del Forno S, et al. Assessment of levator hiatal area using 3D/4D transperineal ultrasound in women with deep infiltrating endometriosis and superficial dyspareunia treated with pelvic floor muscle physiotherapy: randomized controlled trial. Ultrasound Obstet Gynecol 2021;57(5):726–32. | |
Duffy J, et al. A core outcome set for future endometriosis research: an international consensus development study. BJOG 2020;127(8):967–74. | |
Ghai V, et al. A systematic review on reported outcomes and outcome measures in female idiopathic chronic pelvic pain for the development of a core outcome set. BJOG 2021;128(4):628–34. | |
Hansen S, Sverrisdóttir U, Rudnicki M. Impact of exercise on pain perception in women with endometriosis: A systematic review. Acta Obstet Gynecol Scand 2021;100(9):1595–601. | |
Evans S, et al. Psychological and mind-body interventions for endometriosis: A systematic review. J Psychosom Res 2019;124:109756. | |
Mira TAA, et al. Systematic review and meta-analysis of complementary treatments for women with symptomatic endometriosis. Int J Gynaecol Obstet 2018;143(1):2–9. | |
Mira TAA, et al. Hormonal treatment isolated versus hormonal treatment associated with electrotherapy for pelvic pain control in deep endometriosis: Randomized clinical trial. Eur J Obstet Gynecol Reprod Biol 2020;255:134–41. | |
Thabet AAE, Alshehri MA. Effect of Pulsed High-Intensity Laser Therapy on Pain, Adhesions, and Quality of Life in Women Having Endometriosis: A Randomized Controlled Trial. Photomed Laser Surg 2018;36(7):363–9. | |
ACOG. Chronic Pelvic Pain: ACOG Practice Bulletin, Number 218. Obstet Gynecol 2020;135(3):e98–109. | |
Jarrell JF, et al. No. 164-Consensus Guidelines for the Management of Chronic Pelvic Pain. J Obstet Gynaecol Can 2018;40(11):e747–87. | |
Engeler D, et al. EAU Guidelines on chronic pelvic pain. 2020; Available from: http://www.uroweb.org/guidelines/online-guidelines/. | |
Brooks T, et al. Predictors of Psychological Outcomes and the Effectiveness and Experience of Psychological Interventions for Adult Women with Chronic Pelvic Pain: A Scoping Review. J Pain Res 2020;13:1081–102. | |
Fuentes-Márquez P, Cabrera-Martos I, Valenza MC. Physiotherapy interventions for patients with chronic pelvic pain: A systematic review of the literature. Physiother Theory Pract 2019;35(12):1131–8. | |
Klotz Sgr Msc PH, et al. Physiotherapy management of patients with chronic pelvic pain (CPP): A systematic review. Physiother Theory Pract 2019;35(6):516–32. | |
Cottrell AM, et al. Benefits and Harms of Electrical Neuromodulation for Chronic Pelvic Pain: A Systematic Review. Eur Urol Focus 2020;6(3):559–71. | |
Sung SH, et al. Acupuncture Treatment for Chronic Pelvic Pain in Women: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Evid Based Complement Alternat Med 2018:9415897. | |
Mardon AK, et al. Treatment recommendations for the management of persistent pelvic pain: a systematic review of international clinical practice guidelines. BJOG 2021. | |
WHO. International classification of functioning, disability, and health: ICF. World Health Organization: Geneva, 2001. | |
JLA. https://www.jla.nihr.ac.uk/priority-setting-partnerships/endometriosis/. | |
Mardon AK, et al. The Efficacy of Self-Management Strategies for Females with Endometriosis: a Systematic Review. Reprod Sci 2022. | |
Clemens JQ, et al. Urologic chronic pelvic pain syndrome: insights from the MAPP Research Network. Nat Rev Urol 2019;16(3):187–200. | |
Yong PJ, et al. A Proposed Platform for Phenotyping Endometriosis-Associated Pain: Unifying Peripheral and Central Pain Mechanisms. Current Obstetrics and Gynecology Reports 2020;9(3):89–97. | |
Orr NL, et al. Phenotyping Sexual Pain in Endometriosis Using the Central Sensitization Inventory. Journal of Sexual Medicine 2020;17(4):761–70. | |
Edwards S, et al. ‘ReConnect’: a model for working with persistent pain patients on improving sexual relationships. British Journal of Pain 2020;14(2):82–91. |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 2 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards program CLICK HERE)
