Authors
INTRODUCTION
Gynecologists frequently encounter patients with abnormal bowel, bladder, and sexual function. Normal pelvic visceral function depends on the complex interactions of intact somatic and autonomic nervous systems. A number of diseases or injuries of the central or peripheral nervous system can result in alterations in pelvic visceral function (Table 1). The clinical evaluation of patients with urinary incontinence, fecal incontinence, voiding dysfunction, defecatory dysfunction, or pelvic organ prolapse should undergo a history and physical examination that includes a clinical neurologic evaluation. When this evaluation suggests the possibility of an underlying neurologic condition, a number of neurophysiologic tests can be performed to assist in diagnosis. Commonly used tests to evaluate the autonomic function of the bladder and bowel include urodynamics and anal manometry. Tests that are used to directly investigate the integrity of the somatic innervation of the pelvic floor muscles and urinary and anal sphincters include electromyography (EMG), nerve conduction studies such as the pudendal nerve terminal motor latency (PNTML), and the electrophysiologic evaluation of the sacral reflexes.
Table 1. Neurologic causes of bowel and bladder dysfunction
| Brain Lesions |
| Dementia |
| Frontal lobe lesion |
| Cerebrovascular accident |
| Parkinson's disease |
| Multiple sclerosis |
| Hydrocephalus |
| Multiple systemic atrophy (Shy-Drager syndrome) |
| Spinal Cord Lesions |
| Spinal cord injury |
| Intervertebral disc disease |
| Multiple sclerosis |
| Spinal stenosis |
| Transverse myelitis |
| Infections (Lyme disease, herpes zoster, AIDS, polio, tabes dorsalis) |
| Neoplasm |
| Infarction |
| Cauda Equina Lesions |
| Intervertebral disc disease (central herniation) |
| Spinal stenosis |
| Trauma |
| Ankylosing spondylitis |
| Peripheral Nerve Lesions |
| Childbirth-related injury |
| Radical pelvic surgery |
| Trauma |
| Guillain-Barré syndrome |
| Radiation |
| Diabetes mellitus |
| Neoplasm |
| Endometriosis |
Neurophysiologic tests have played an important role in expanding our understanding of the relationship between vaginal childbirth, pelvic floor denervation, pudendal neuropathy, and the development of disorders of the pelvic floor, like urinary and fecal incontinence and pelvic organ prolapse. Recent studies suggest neurophysiologic testing may have a prognostic role in predicting likelihood of success for certain therapies such as Burch colposuspension for treatment of stress urinary incontinence and sacral neuromodulation for the management of refectory urge urinary incontinence.1, 2, 3
While these neurophysiologic tests are not typically in the purview of the practicing gynecologist, a familiarity with these techniques and their application is important for those interested in the evaluation and management of patients with disorders of the pelvic floor. This chapter reviews normal pelvic floor neuroanatomy, discusses the clinical evaluation of sacral nervous system, and reviews the common neurophysiologic tests used to investigate pelvic floor dysfunction, including EMG, nerve conduction studies, and sacral reflex studies. A review of the clinical conditions in which sacral neurophysiologic testing may be useful is also included. A detailed description of the central control of bowel and bladder function is beyond the scope of this chapter and can be found elsewhere. Additionally, a discussion of the urodynamic evaluation, an invaluable tool for investigating the autonomic function of the lower urinary tract, is found elsewhere.
NEUROANATOMY OF THE FEMALE PELVIS
To understand and apply neurophysiologic testing to pelvic floor symptoms, a comprehensive understanding of pelvic neuroanatomy is necessary. The nervous system can be divided into the central nervous system, including the brain and spinal cord, and the peripheral nervous system, which includes each of the 31 paired spinal nerves and the 12 paired cranial nerves. The peripheral nervous system is divided into two functional divisions, the somatic component, which innervates skeletal muscle and the autonomic component, which innervates smooth muscle, cardiac muscle, glands, and viscera. Normal pelvic floor function depends on intact central and peripheral nervous systems, including both somatic and autonomic components.
Sensory nerve fibers that carry a message to the central nervous system are labeled afferent fibers. Nerve fibers that carry messages from the central nervous system to their target organ are labeled efferent fibers. The somatic efferent nerves to skeletal muscles are typically large myelinated fibers that innervate the extrafusal muscle fibers, known as alpha (α) motor neurons, and smaller myelinated fibers that innervate the muscle spindles (intrafusal muscle fibers), known as gamma (γ) fibers. Somatic afferent nerves that sense touch and pressure (Aβ fibers) are myelinated and intermediate in size, between alpha and gamma neurons. Afferent neurons that sense pain (nociceptors) are small unmyelinated fibers (C fibers). Larger-diameter fibers conduct action potentials faster than do smaller fibers, and myelinated fibers conduct faster than unmyelinated fibers.
SOMATIC INNERVATION
The terminal portion of the spinal cord is known as the conus medullaris. The conus medullaris contains most of the nerve cell bodies that supply the pelvic floor. In general, the peripheral motor system begins as a lower motor neuron in the ventral horn of the spinal cord, which gives rise to a motor root. The motor root exits ventrally from the spinal cord and unites with the sensory root from the same spinal segment to form a spinal nerve. The lower motor neurons that supply anal and urethral sphincters are located together in Onuf's nucleus. Onuf's nucleus is located on the ventrolateral border of the ventral horn of the sacral spinal cord. The motor neurons in Onuf's nucleus are smaller and demonstrate greater dendritic arboration than the motor neurons that supply the other skeletal muscles of the body.4 The motor neurons of Onuf's nucleus demonstrate the unique characteristic of being resistant to polio and amyotrophic lateral sclerosis but are selectively involved in multiple system atrophy (MSA), also known as Shy-Drager syndrome.5 Unlike the urethral and anal sphincters and similar to that of limb muscles, the motor neurons of the levator ani muscles are located in the ventral horn of the sacral spinal cord outside of Onuf's nucleus.6,7,8 The levator ani motor neurons have similar size and appearance as the motor neurons of the lower extremity.
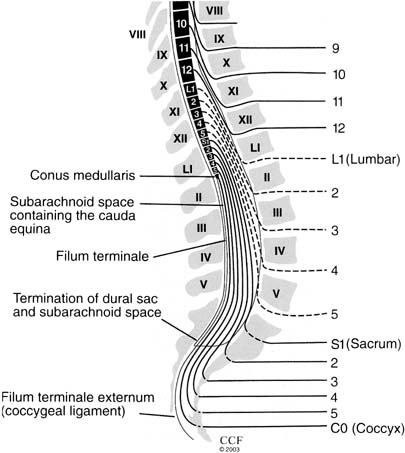
The primary sensory neuron, the dorsal root ganglion (DRG), lies outside the spinal cord and is found in the intervertebral foramen. The DRG is composed of bipolar cells that project centrally as sensory nerve roots, which enter the spinal cord and synapse with sensory neurons in the dorsal horn. The DRG also gives rise to the sensory fibers that project peripherally and form the spinal nerve. During early development the bony vertebral column outgrows the spinal column. In an adult the spinal cord ends approximately at the level of the disk between the first and second lumbar vertebrae. Thus, the lumbosacral nerve roots travel all the way from the conus medullaris at the L1/L2 level to their corresponding vertebral foramina in the lower lumbar vertebrae and sacrum. This portion of the cord is called the cauda equina (“horse's tail”) and is particularly susceptible to damage from lumbosacral disk disease and other traumatic injury (Fig. 1). The spinal nerves divide into dorsal rami, which run posteriorly and supply sensory innervation to the skin over the spine and sacrum and innervation to the paraspinal muscles and the ventral rami, which course anteriorly to form the lumbosacral plexus. The lumbosacral plexus divides into dorsal and ventral divisions, which then give rise to the peripheral nerves that supply the lower extremities and pelvis.
The skeletal muscles of the pelvic floor include the levator ani muscles, the coccygeus muscles, the external anal sphincter, the striated urethral sphincter, and the superficial perineal muscles (bulbocavernosus, ischiocavernosus, and transverse perinei). The levator ani muscle complex consists of the iliococcygeus, pubococcygeus, and puborectalis muscles. They extend from the pubis to the coccyx and laterally to obturator internus muscle where they are attached via the arcus tendineus levator ani. They separate in the midline to form the genital hiatus through with the urethra, vagina, and anus pass. The puborectalis muscle forms a sling behind the rectum to form the anorectal angle and contribute to fecal continence. When contracted, the levator ani muscles squeeze the vagina, urethra, and rectum closed by compressing them against the pubic bone and lifting the pelvic floor and visceral organs cephalad. Like other postural muscles, the levator ani muscles maintain constant tone except during voiding, defecation, and Valsalva maneuver. This constant tone closes the genital hiatus and eliminates any opening through which prolapse could occur. It also forms a horizontal shelf on which the pelvic organs are supported.9 The external anal sphincter and striated urethral sphincter also have tonic activity, although much of the resting tone of these sphincters is maintained by their autonomic component.10 The levator muscles and the skeletal components of the urethral and anal sphincters all have the ability to contract quickly at the time of an acute stress, such as a cough or sneeze, to maintain continence.
PUDENDAL NERVE
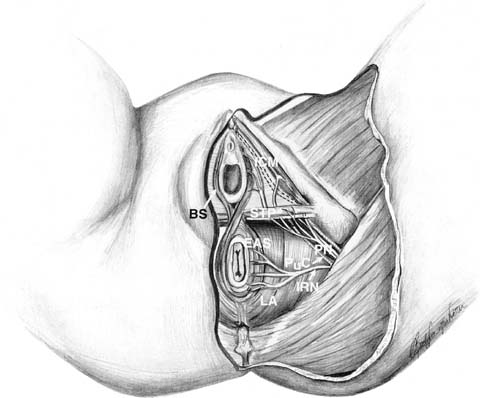
The pudendal nerve supplies the innervation of external anal sphincter and the striated urethral sphincter. The pudendal nerve also provides innervation to the superficial perineal muscles and sensory innervation of the perineal skin. It is formed in the lower division of the lumbosacral plexus from portions of the S2–S4 nerve roots.11 These nerve roots join to form the pudendal nerve on the ventral surface of the piriformis muscle. The pudendal nerve then passes behind the sacrospinous ligament (and overlying coccygeus muscle) just medial to the ischial spine, to exit the pelvic cavity through the greater sciatic foramen. The nerve then enters the ischioanal fossa (previously called the ischiorectal fossa) through the lesser sciatic notch. After traveling along the medial surface of the obturator internus muscle, the pudendal nerve enters an area of fascial investment called the pudendal canal (also called Alcock's canal). The pudendal canal is located on the medial surface of the ischium and is approximately 3 cm in length.11 Within the pudendal canal, the pudendal nerve is fixed in place, and some have suggested that this is an area that is susceptible to stretch injury during vaginal delivery.12, 13 The first major branch of the pudendal nerve is the inferior rectal nerve. In most people, this branch separates from the pudendal nerve within the pudendal canal, and then penetrates through the medial wall of the pudendal canal at its approximate midpoint. The inferior rectal nerve then crosses the ischioanal fossa coursing inferiomedially to divide into multiple small branches that innervate the external anal sphincter and peri-anal skin.11 In approximately one-fifth of women, the inferior rectal nerve branches from the pudendal nerve and crosses the ischioanal fossa without ever entering the pudendal canal.11 After exiting the pudendal canal, the pudendal nerve then separates into two remaining major branches, the dorsal nerve of the clitoris, and the perineal nerve (Fig. 2). The dorsal nerve of the clitoris travels along the margin of the inferior pubic ramus to terminate at the clitoris. The perineal nerve branch provides innervation to the ischiocavernosus, bulbocavernosus, and superficial transverse perineal muscles as well as the striated urethral sphincter and labial skin.
LEVATOR ANI NERVE
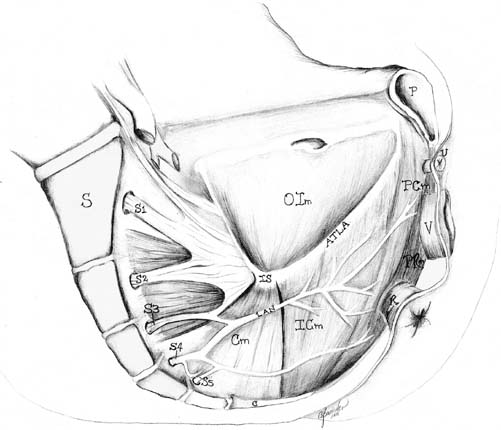
The standard textbook descriptions of the motor innervation of the pelvic floor suggest that the levator ani muscle complex is dually innervated by the pudendal nerve and by direct sacral nerve roots (S3–S4) traveling on the superior surface of the muscles. Recent anatomic, neurophysiologic, and experimental evidence indicate that these standard descriptions are inaccurate and that the levator ani muscles are innervated solely by a nerve traveling on the superior (intrapelvic) surface of the muscles without contribution of the pudendal nerve.11, 14, 15, 16 Barber et al. who examined the innervation of the levator ani muscles in 12 female cadavers, the authors histologically confirmed their gross findings and found no contribution from the pudendal nerve to any of the levator ani muscles.11 They identified a nerve that originated from S3–S5 foramina and traveled along the superior surface of the levator ani muscles before penetrating each of the pelvic floor muscles at their approximate midpoint (Fig. 3). After exiting the sacral foramina, the levator ani nerve crossed the superior surface of the coccygeus muscle approximately 3 cm medial to the ischial spine. It then coursed along the superior surface of the iliococcygeus muscle and sent off one or more branches to penetrate the iliococcygeus muscle. The major branch entering the iliococcygeus muscle did so at a point approximately halfway between the pubic bone and the ischial spine and 2–3 cm below the tendinous insertion of the iliococcygeus muscle on the obturator internus fascia (arcus tendineus levator ani). The nerve then continued on to enter the pubococcygeus and then puborectalis muscles. The major branch innervating the pubococcygeus and puborectalis muscles did so at a point midway between the inferior pubis and the coccyx. In several cadavers, a small nerve branch originating from S4/S5 coursed independently to innervate the midportion of the puborectalis muscle.
Many electrophysiologic studies have also demonstrated that the levator ani muscles and the external anal sphincter have physiologically distinct innervations and that the pudendal nerve does not appear to innervate the iliococcygeus, pubococcygeus, or puborectalis muscles.13, 14, 15 Additionally, a recent nerve transection study in the squirrel monkey confirmed this pattern of innervation.16 Transection of the levator ani nerve resulted in decreased muscle mass and myofiber size of the levator ani muscles, whereas transection of the pudendal nerve had no effect on the levator ani. Neuroanatomical tracer studies in the rat and cat models also support the finding of a distinct “nonpudendal” innervation of the pelvic floor.6, 7, 8 These studies demonstrate that tracers injected into the levator ani muscle-labeled neurons in the midportion of the ventral horn,6, 7, 8 but not in Onuf's nucleus where all pudendal nerve motor neurons are located.6, 17, 18
That the levator ani muscles and the urethral and anal sphincters have separate and distinct innervations may have important implications in understanding childbirth-related denervation injury and subsequent development of pelvic floor disorders. It also has implications with regard to neurophysiologic testing, because both the levator ani nerve and the pudendal nerve need to be evaluated to completely investigate the neurologic function of the pelvic floor. Electrophysiologic evaluation of the anal sphincter cannot be used as a surrogate for an investigation of the levator ani muscles as some have suggested.
AUTONOMIC INNERVATION
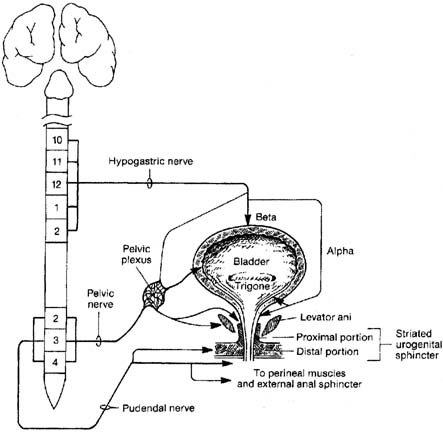
The autonomic nervous system consists of general visceral efferent and general visceral afferent fibers. It is subdivided anatomically and functionally into the sympathetic and parasympathetic systems. In the pelvis, the sympathetic nervous system acts to promote storage by causing relaxation of the bladder and rectum and contraction of the smooth muscle components of the urethral and anal sphincter (Fig. 4). Sympathetic nerves to the pelvis originate at the T5 to L2 spinal level. Preganglionic fibers exit the spinal cord in thoracic and lumber nerves and then travel from the spinal nerves to the sympathetic chain via white rami communicantes. Some end in paravertebral sympathetic chain ganglia, from which unmyelinated postganglionic fibers rejoin the spinal nerves via gray rami communicantes to then innervate their target organs, along with somatic peripheral nerves such as the pudendal nerve. Others continue through the paravertebral chain without synapsing and reach the inferior mesenteric ganglion. Postganglionic fibers then travel along the hypogastric plexus to enter the pelvis and innervate the pelvic viscera.
The parasympathetic nerve supply to the pelvic viscera originates from the second, third, and fourth sacral nerves. Preganglionic parasympathetic nerves travel directly anterior, several centimeters above the pelvic floor, to combine with the hypogastric plexus and pelvic sympathetic nerves to form the pelvic nerve plexus. This plexus of nerves leaves the sacral surface to fan out on either side of the rectum approximately 3–4 cm superior to the pelvic floor muscles.11 The plexus then continued distally to invest the lateral aspects of the vagina, particularly the upper third, and then invest the detrusor muscle at the level of the bladder base. The parasympathetic ganglia are located within or very near the organs they supply, thus having very short postganglionic fibers. Visceral sensory innervation within the pelvis can follow the sympathetic and parasympathetic nerves.
NEUROLOGIC EXAMINATION OF THE PELVIC FLOOR
Urinary incontinence, fecal incontinence, urinary retention, and other pelvic floor disorders may be the presenting symptoms of neurologic disease. As such, all women with these symptoms should undergo, at minimum, a screening lumbosacral neurologic examination. This screening examination should include assessments of: (1) pelvic floor muscle strength; (2) anal sphincter resting tone; (3) voluntary anal contraction; and (4) perineal sensation. This simple screening examination can be performed quickly and easily as part of the gynecologic examination. When abnormalities are noted, or when an individual is suspected of having neurologic dysfunction, a comprehensive neurologic examination with particular emphasis on the lumbosacral nerve roots should be performed. The comprehensive evaluation should include an evaluation of mental status, motor strength, sensory function, and deep tendon and sacral reflexes. This comprehensive evaluation should be performed before any neurophysiologic testing, because any such testing should only be interpreted in the context of the patient's history and physical examination findings.
Mental status is determined by noting the patient's level of consciousness, orientation, memory, speech, and comprehension. Disorders associated with mental status aberrations that may result in changes in bowel or bladder function include dementia, frontal lobe lesions, strokes, Parkinson's disease, and normal pressure hydrocephalus.
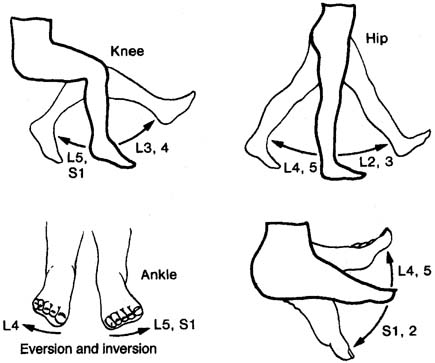
Motor strength of the lower extremities, anal sphincter, and levator ani muscle should be assessed when evaluating sacral neurologic function. When a more generalized neurologic disorder is suspected, a motor evaluation of the cranial nerves and upper extremities should also be performed. In addition to an assessment of strength, muscles should be inspected for atrophy, fasciculations, and spasticity. To test for sacral motor function, the patient extends and flexes the hip, knee, and ankle and inverts and everts the foot (Fig. 5). Skeletal muscle strength is graded on a scale from 0 to 5 (Table 2). Common diseases associated with motor abnormalities that can effect bowel and bladder continence include Parkinson's disease, multiple sclerosis, cerebrovascular disease, lumbar disc disease, infections, and tumors.
Table 2. Grading scales for muscle strength
| Score | Limb Muscles | Levator Ani |
| 0/5 | No movement | No contraction |
| 1/5 | Trace of contraction | Flicker, barely perceptible |
| 2/5 | Active movement when gravity eliminated | Loose hld, 1 to 2 sec |
| 3/5 | Active movement against gravity only | Firmer hold, 1 to 2 sec |
| 4/5 | Active movement against resistance but not normal | Good squeeze, 3 to 4 sec, pulls fingers in and up loosely |
| 5/5 | Normal strength | Stronger squeeze, 3 to 4 sec, pulls in and up snugly |
Levator Ani Muscle
The most common method used to assess pelvic floor muscle strength is digital palpation. To assess pelvic floor muscle strength, an examiner places two fingers into the posterior vagina at least 2 to 4 cm above the hymenal ring with the patient in lithotomy position.19 The patient is asked to relax and the levator ani muscles are palpated bilaterally to assess bulk and spasticity. The patient is then asked to contract the pelvic floor muscles maximally for as long as possible. Instructing the patient to “squeeze around my fingers” and/or “squeeze the muscles you would use to hold your urine or to avoid passing gas” will assist the patient in appropriately identifying the levator ani muscles. Patients should be encouraged to avoid contracting their rectus abdominus, adductor, or gluteus muscles. The presence of a contraction, the strength and duration of any contraction, and the ability of the levator muscle to elevate the examiner's fingers should all be assessed. Muscle function is then quantified using one of several scales. A 0 to 5 rating scale similar to that used for rating other skeletal muscles is used commonly20 (see Table 2). Another technique rates three characteristics (pressure, duration, and displacement) each on a 0 to 3 point scale, resulting in an overall score of 0 to 921, 22 (Table 3). While this scale is more complicated than the 5-point scale, it has undergone more careful validation demonstrating good interrater and intrarater reliability and correlating with surface EMG activity and urinary continence status.21, 22 Neurologic causes for a weak or absent levator ani muscle contraction include lesions involving the conus medullaris, the cauda equina, the lumbosacral plexus, or the levator ani nerve. A common nonneurologic cause for a weakened levator ani muscle is direct muscle trauma from childbirth.23 Levator ani myopathy also occurs but is infrequent. Neurophysiologic testing, particularly needle EMG, can be useful for identifying neurologic from nonneurologic causes of levator ani weakness.
Table 3. Pelvic muscle rating scale
| Pelvic Muscle Contraction Rating Scale | ||||
| 0 | 1 | 2 | 3 | |
| Pressure | None | Weak | Moderate | Strong |
| Duration | None | <1 sec | 1–5 sec | >5 sec |
| Displacement | None | Slight anterior | Whole anterior | Gripped |
Romanzi LJ, Polaneczky M, Glazer HI. Neurourol Urodynam 18:603–612, 1999
Anal Sphincter
Both the resting tone and voluntary contraction of the anal sphincter should be assessed. The examiner should first inspect the anus, looking for scarring or a gaping sphincter. Women with disruption of the external anal sphincter may have gross abnormalities of the perineal body with a “dove-tail” sign in the area of the disrupted sphincter.19 A digital rectal examination should be performed, noting the resistance to entry of the examining finger. Approximately 50–85% of overall resting anal tone is generated by the internal anal sphincter.24 Loss of resting tone suggests disruption of the internal anal sphincter and/or an injury to its sympathetic innervation (i.e., pelvic plexus injury).25 The patient then should be asked to maximally squeeze the anal sphincter. The presence of a strong voluntary anal sphincter contraction indicates intact pudendal innervation and external anal sphincter. Unlike pelvic muscle strength, there is no widely accepted validated scale for quantifying anal squeeze strength. Kaushal and Goldner used a 0 to 3+ scale and found that it had a high correlation with maximum squeeze pressure as measured by anal manometry.26 Others have used modified versions of the pelvic muscle rating scale to quantify anal squeeze strength.27 Absence or decrease of both anal sphincter tone and voluntary contraction suggests a possible sacral or peripheral nerve lesion. Preservation of resting tone in the absence of a voluntary contraction suggests a suprasacral lesion.
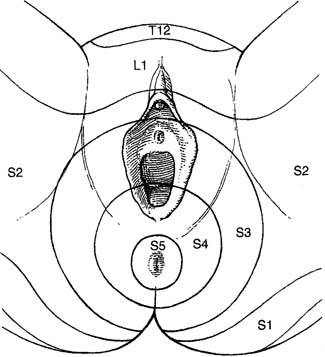
Sensory function is evaluated by testing the lumbo-sacral dermatomes for the ability to sense light touch, pinprick, and temperature. The important sensory dermatomes include the perineum and perianal skin (pudendal nerve, S2–S4), mons pubis, and upper aspect of labia majora (ilio-inguinal nerve, L1–L2), front of the knees (L3–L4), and sole of the foot (S1). Dermatome maps (Fig. 6) are useful for characterizing sensory deficits, although it is important to remember that there can be considerable overlap between dermatomes. Position sense and vibration should be assessed but need only be evaluated in the distal extremities.28 Visceral sensation of the bladder and rectum can be assessed with cystometry and anal manometry, respectively. Loss of perineal sensation in a patient with bowel or bladder dysfunction, particularly if acute, should always alert the examiner to a potentially serious neurologic problem. Neurophysiologic testing and/or radiologic evaluation should be performed to assess for conus medullaris or cauda equina syndrome.
Deep tendon reflexes are assessed to evaluate the integrity and interaction of upper and lower motor neurons. They include the patellar reflex (L3–L4), the Achilles tendon reflex (L5, S1, S2) and the plantar toe reflex (Babinski's sign). In patients with upper motor neuron lesions, the deep tendon reflexes are hyperactive and Babinski's sign is positive (dorsi-flexion of the big toe). This is often associated with bladder overactivity. In contrast, lower motor neuron lesions involving the cauda equina or lumbosacral plexus often result in hypoactive deep tendon reflexes, a negative Babinski's sign, and can be associated with a hypoactive or acontractile bladder.
Sacral reflexes that should be assessed include the anal reflex and the bulbocavernosus reflex. These reflexes evaluate spinal cord reflex arcs of the pudendal nerve. The anal reflex evaluates the integrity of the sensory and motor neurons of the inferior rectal branch of the pudendal nerve. It is elicited by lightly stroking the peri-anal skin and visualizing an anal sphincter contraction. If the contraction is not visualized it can often be palpated with an examining finger.28 The anal reflex is a polysynaptic response, which is absent in patients with lesions affecting the nerve supply to or from the anal sphincter, but is preserved in patients after transection of the spinal cord above L3.29 The bulbocavernosus reflex evaluates the sacral reflex arc involving the sensory neurons of the clitoral branch of the pudendal nerve and the motor neurons of the perineal and inferior rectal nerves. It is elicited by lightly tapping or squeezing the clitoris and visualizing a contraction of the bulbocavernosus muscle and/or external anal sphincter. Absence of either the anal reflex or the bulbocavernosus reflex suggests a lower motor neuron lesion involving the sacral nerve roots; however, absence of the reflex may also be a consequence of trauma from vaginal childbirth and not necessarily significant neurologic disease. In a study evaluating the bulbocavernosus reflex, Blaivas and associates found that 19% of neurologically intact women had an absent bulbocavernosus reflex.30 In women with incomplete lower motor neuron lesions, 47% had an absent bulbocavernosus reflex; in women with complete lower motor neuron lesions, all had an absent reflex.
FUNDAMENTALS OF ELECTRODIAGNOSTIC TESTING
Common neurophysiologic tests used to investigate peripheral neurologic disease include EMG, nerve conduction studies, and spinal reflex testing. These tests are often performed together, because each provides unique information about the integrity of the nervous system. The results of electrodiagnostic testing should always be interpreted in the context of the patient's clinical presentation and examination findings. Other tests that are often useful in evaluation of the patient with pelvic floor symptoms and suspected neurologic disease include urodynamics, anal manometry, MRI (lumbar and pelvic), dynamic proctography, and endo-anal ultrasound.
The next section is intended to provide a fundamental overview of the neurophysiologic tests commonly used in the investigation of pelvic floor disorders. Some common indications for neurophysiologic testing of the pelvic floor are listed in Table 4.
Table 4. Indications for neurophysiologic testing of the pelvic floor
| Incontinence or voiding dysfunction associated with abnormal lower extremity or sacral neurologic examination |
| Pelvic floor disorder in a patient with known neurologic disease (i.e., multiple sclerosis, Parkinson's disease, etc.) |
| Voiding dysfunction in young women |
| Urinary retention in patient without obvious cause (i.e., advanced pelvic organ prolapse, previous anti-incontinence surgery) |
| Diabetics with bowel or bladder disorders |
| Evaluation for neurogenic fecal incontinence |
| Prior to anal sphincter repair (for prognosis and/or sphincter mapping) |
| Unexplained perineal numbness or pain |
| For differentiation between early Parkinson's disease and multiple systemic atrophy |
| Bowel or bladder dysfunction unexplained after standard evaluation |
ELECTROMYOGRAPHY
The term electromyography is a general term that refers to methods of studying electrical activity of muscle. A variety of EMG techniques exist, each with their own indications, advantages, and limitations. Of the many EMG techniques, only a few have utility for the study of pelvic floor disorders. EMG techniques study neuromuscular activity of striated muscles using a recording electrode that is inserted into or placed on the surface of a muscle. Bioelectric potentials generated by the depolarization of the skeletal striated muscle are picked up by this electrode and then filtered and amplified. They are displayed on an oscilloscope for visual analysis and fed through a speaker system so they can be monitored acoustically. Modern computer-based equipment allows for conversion of the signal into digital data that can then be easily stored, processed, and analyzed. EMG studies used to evaluate pelvic floor disorders can be broadly separated into two categories, kinesiological EMG (kEMG) and motor-unit EMG.31 kEMG is used simply to assess the activity or inactivity of a muscle, usually the urethral or anal sphincter. It is used in conjunction with physiologic tests such as urodynamics and anal manometry to assess sphincter relaxation during voiding or defecation. kEMG is also used for biofeedback during pelvic muscle rehabilitation for treatment of urinary or fecal incontinence. In contrast, motor-unit EMG is a diagnostic test used to assess the neuromuscular function of a muscle. It can differentiate normal muscle from denervated/reinnervated or myopathic muscle. Common techniques used for motor-unit EMG are concentric needle EMG (CnEMG) and single-fiber EMG (SfEMG). Motor-unit EMG that uses computer-assisted digital analysis to obtain a faster, more standardized, and detailed assessment of neuromuscular function than traditional needle EMG is known as quantitative EMG (qEMG). The general principles, techniques, interpretation, and limitations of each of these EMG techniques as they apply to the investigation of pelvic floor disorders and sacral neurologic disease are outlined.
KINESIOLOGICAL ELECTROMYOGRAPHY
kEMG is used to assess the activity or inactivity of a muscle during a defined activity. kEMG provides information on the timing of a muscle contraction by recording the increase in electrical activity that occurs during a contraction through surface or wire/needle electrodes placed on or within the specific muscle(s) being investigated. This increase in electrical activity correlates moderately with muscle strength and has been used by some as a surrogate for measuring this parameter.32 kEMG cannot, however, be used to detect neuropathic or myopathic changes within a muscle.
In the investigation of pelvic floor disorders, kEMG is used most frequently during urodynamic evaluations. Specifically, it is used to assess urethral sphincter and/or pelvic floor muscle activity during voiding. By simultaneously recording pelvic floor muscle activity using kEMG and detrusor pressure using the urodynamic pressure catheters, detrusor/sphincter coordination can be assessed. The primary role of kEMG in this context is to detect the condition of detrusor sphincter dyssynergia in which a detrusor contraction is coupled with a simultaneous urethral sphincter contraction resulting in abnormal voiding and, frequently, urinary retention. Similarly, it can also be used to investigate coordinated relaxation of the levator ani muscles during defecation. kEMG has been used by some to diagnose anismus, a condition characterized by an inappropriate contraction of the levator ani complex, particularly the puborectalis muscle, during defecation resulting in obstructed evacuation. Another common use for kEMG is to provide visual and/or audio biofeedback of pelvic floor muscle activity during a pelvic muscle exercise program for treatment of urinary or fecal incontinence. Pelvic floor rehabilitation using biofeedback has long been advocated as more effective than teaching pelvic muscle exercises with verbal instructions alone, although recent studies have called this into question.33
Technique
kEMG can performed with various types of surface or intramuscular (needle or wire) electrodes. Surface electrodes measure the net electrical activity within a muscle. They have the advantage of being simple and noninvasive; however, they are prone to artifact and contamination from signal from other muscle. Because they measure net electrical activity of a muscle and are not capable of measuring individual motor unit potentials, surface electrodes cannot be used to diagnostically evaluate for denervation/reinnervation injury or myopathic diseases. Surface electrodes are used commonly for biofeedback for pelvic floor strengthening in the treatment of urinary or fecal incontinence. For measuring levator ani activity, two small circular skin electrodes are commonly applied on each side of the perineum 1 centimeter anterior to the anus.32 Anal plugs with concentric ring electrodes are commonly used to assess external anal sphincter activity for biofeedback-assisted sphincter strengthening for the treatment of fecal incontinence. Similarly, ring electrodes placed on a Foley catheter 1 centimeter distal from the balloon have been used to measure urethral sphincter activity. Electrical activity measured from surface or ring electrodes are amplified and visually displayed on a computer screen and/or audibly projected through a speaker system to provide the patient with immediate feedback during a contraction. Often surface electrodes are also placed on the gluteus or abdominal muscles as well so that patients can learn to appropriately contract their pelvic floor/sphincter muscles while avoiding simultaneous contraction from other surrounding muscle groups. Needle electrodes, which are typically placed 5 mm ventral to the urethral meatus into the striated urethral sphincter muscle, are consistently more interpretable than surface electrodes.34 However, difficulties associated with correct needle placement, patient discomfort and the requirement for a degree of patient mobility during testing have limited their use for kEMG in clinical settings.
To evaluate detrusor–sphincter coordination in a patient with voiding dysfunction, kEMG is performed in conjunction with a urodynamic evaluation. Either surface electrodes are applied to the perineum as described, or a wire electrode is placed peri-urethrally into the urethral sphincter. The electrical activity of the pelvic floor/urethral sphincter is then recorded during the voiding phase of the study.
Interpretation
In a neurologically intact subject, voiding is characterized by cessation of all sphincter EMG activity just before contraction of the detrusor muscle. In patients who have spinal cord lesions between the lower sacral segments and the upper pons, coordination between the detrusor muscle and the urethral sphincter can be lost. This detrusor sphincter dyssynergia is characterized by an increase in sphincter EMG activity during a detrusor contraction rather than a decrease, and these patients typically have severe voiding dysfunction and urinary retention.
Limitations
As a diagnostic test, except for the evaluation of detrusor–sphincter coordination, the relevance of kEMG, is unclear and no standardized method for performing or interpreting kEMG has be accepted.35 In the artificial setting of the urodynamic laboratory, many neurologically intact women will contract their urethral sphincter during voiding because of embarrassment and/or the discomfort of the urethral catheters and electrodes. It is, therefore important to ask a patient whether she is trying to stop voiding voluntarily so that detrusor sphincter dyssynergia is not diagnosed in error. In a study of 550 consecutive patients, Blaivas and associates found that dyssynergia was only found in patients with well-defined lesions of the suprasacral spinal cord.36 Therefore, the diagnosis of detrusor–sphincter dyssynergia made in the absence of other neurologic deficits consistent with this level of injury should be suspect. Inappropriate urethral contraction during voiding can also be a learned behavior resulting in dysfunctional voiding.37 As a method of biofeedback, kEMG is useful, but the limitations associated with surface electrodes still apply.
CONCENTRIC NEEDLE ELECTROMYOGRAPHY
CnEMG is a widely used diagnostic test for evaluating the neuromuscular integrity of skeletal muscles. It can be used to differentiate normal muscle from muscle that is neuropathic or myopathic. A concentric needle electrode consists of a stainless steel outer cannula within which runs a fine silver, steel, or platinum wire that is insulated except at its tip. The concentric needle is inserted into a muscle where the inner wire serves as a recording electrode while the outer cannula serves as a reference electrode. Bioelectrical potentials are measured as voltage differences between the two electrodes that are then recorded, displayed, and analyzed.
A CnEMG examination provides information on the insertional activity, spontaneous activity, motor unit action potentials (MUAPs), and recruitment pattern (also known as interference pattern) of a muscle. Insertional activity is the electrical activity that occurs when the needle electrode is first introduced into a muscle or is moved, is the result of mechanical stimulation or injury of the muscle fibers, and usually stops within approximately 2 seconds of movement. After resolution of the insertional activity, a typical limb muscle is electrically silent when at rest. Denervated muscle fibers may produce rhythmic spontaneous electric potentials, such as fibrillation waves or positive sharp waves. The presence of this spontaneous activity in a resting muscle is a sign of denervation. In contrast to limb muscles but similar to the postural muscles of the back, the levator ani muscles, and the urethral and anal sphincters are tonically active and demonstrate normal continuously firing action potentials even at rest. It is important to be able to distinguish abnormal spontaneous activity from this normal tonic activity when performing CnEMG on these muscles.
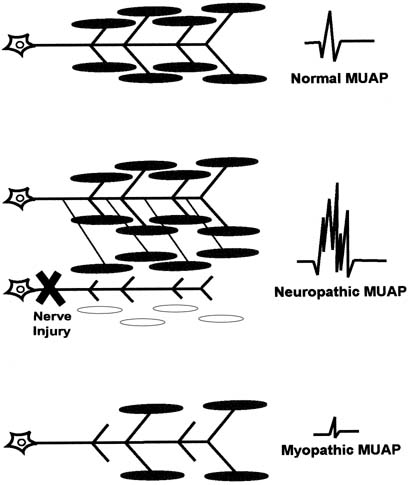
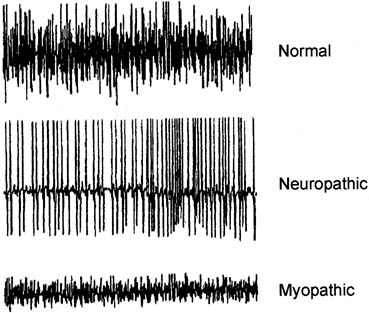
The motor unit is the smallest functional unit of the motor system and consists of a motor neuron, its axon, and all of the muscle fibers innervated by the axon. The motor unit in a normal human limb muscle consists of several dozen muscle fibers lying within an area of 5–10 mm in diameter. The motor unit action potential (MUAP) is a compound potential representing the sum of the individual action potentials generated in the few muscle fibers of the motor unit that are within the pick-up range of the recording electrode. With slight voluntary contraction of a muscle, individual MUAPs can be seen and MUAP analysis can be performed. Analyzing the shape, amplitude, duration, and number of phases of a MUAP allows a normal motor unit to be distinguished from one that has been denervated and reinnervated or one that is myopathic. Increasing force within a muscle is accomplished by an orderly increase in the firing rate of individual MUAPs and the recruitment of additional MUAPs. In normal muscle, as the force of voluntary contraction increases, motor units are recruited in a specific order that is determined by the thresholds that are inherent to the individual unit.38 Analyzing this recruitment pattern provides additional information about the health of a muscle and its innervation. When a muscle is maximally contracted, the number and firing rate of the individual MUAPs becomes so great that they can no longer be distinguished and the baseline is obscured. This is called an interference pattern (IP). Neuropathic and myopathic muscles each have distinct interference patterns that can be readily distinguished from that of normal muscle.
CnEMG can be performed on an individual muscle, as on the anal sphincter when evaluating isolated fecal incontinence, or can be systematically performed on several muscles to determine the level of a neurologic injury. All muscles that are innervated by one spinal segment (level) are referred to as a myotome. Using CnEMG to systematically evaluate several muscles in different myotomes often permits localization of a lesion to the spinal root, nerve plexus, or an individual peripheral nerve. In a patient with bowel or bladder dysfunction in which a neurologic cause is suspected, a thorough evaluation often requires EMG of the lower extremity as well as pelvic floor musculature.
Technique
The clinical history and sacral neurologic examination should be carefully reviewed before beginning the EMG evaluation, because this will help determine which muscles should be examined. Ideally, the evaluation should be performed in a shielded room to prevent interference from other electronic devices or AC power cords. The patient is placed in a comfortable position that allows access to the pelvic floor musculature, usually the dorsal lithotomy or lateral decubitus positions. A grounding surface electrode is applied. Most laboratories do not use local anesthetics in any form before insertion of the needle electrodes, although some authors advocate using a topical anesthetic, particularly for examination of the urethral or anal sphincter.35 After wiping the skin overlying the appropriate muscle with alcohol, the concentric needle electrode is inserted until the insertional activity of the muscle is noted, confirming that the electrode is within the muscle. The EMG investigation consists of analysis of electrical activity at rest (assessment of spontaneous activity), at slight voluntary contraction (MUAP analysis), and at strong contraction (interference pattern analysis). Generally the most painful portion of the examination is the initial insertion through the skin, so several sites within the muscle should be sampled by moving the tip of the needle without removing it from the skin. Depending on the muscle, more than one skin penetration may be necessary. Both the visual output on the screen of the EMG machine and the audio output from the speaker are used to assess the quality of the recording and identify electrophysiological phenomena. Commonly used settings for CnEMG evaluation of the pelvic floor muscles are: filter settings, 5–10 kHz; horizontal sweep speed, 10 msec/div; and gain setting, 50–500 μV/div.35
Anal Sphincter
Both the subcutaneous and deep portions of the external anal sphincter (EAS) are accessible for CnEMG evaluation. To study the subcutaneous portion of the EAS, the needle electrode is inserted 1 centimeter outside the mucocutaneous junction of the anal orifice to a depth of 3–6 mm beneath the skin.39 The deep portion of the EAS is assessed by inserting the needle at the mucocutaneous junction of the anus, at an angle of approximately 30 degrees to the anal canal axis, for a depth of 1–3 cm.39 Typically the subcutaneous and/or deep portion of the EAS are sampled in at least four quadrants, approximately divided into the upper and lower and left and right portions of the sphincter. Ideally, 20 or more MUAPs should be sampled during the evaluation.
Anal mapping has been used in the past to identify the location of a sphincter defect before an anal sphincteroplasty in the treatment of fecal incontinence. To identify the precise location of a sphincter defect, more needle insertions are typically required, usually at 9:00, 10:00, 12:00, 2:00, 3:00, and 6:00. Endo-anal ultrasound has largely replaced anal mapping with EMG for the identification and localization of sphincter defects.40, 41
Urethral Sphincter
The external urethral sphincter can be studied by inserting the electrode into the sphincter muscle periurethrally or transvaginally. For the periurethral approach, the needle is inserted approximately 5 mm anterior to the external urethral meatus (12:00 position) to a depth of approximately 1–2 cm.42 For the transvaginal approach, the posterior vaginal wall is retracted with a speculum and the needle is inserted approximately 2 cm proximal to the external urethral meatus, off the midline, and directed laterally into the urethral sphincter.42 Although slightly more painful, the periurethral approach provides superior sampling of the urethral sphincter, obtaining as many as twice the number of MUAPs as the transvaginal approach.42 At least 10 MUAPs should be recorded to adequately evaluate the urethra.43
Bulbocavernosus
The bulbocavernosus muscle is a readily accessible perineal muscle that is innervated by the perineal branch of the pudendal nerve. The bulbocavernosus muscle can be reached either transmucosally with a needle insertion medial to the labia minora or through the skin lateral to the labia majora.35
Levator Ani
The iliococcygeus and pubococcygeus portions of the levator ani muscle complex are most easily investigated using a transvaginal approach. The muscles are localized by first inserting two fingers into the vagina and asking the patient to contract. One side of the levator complex is isolated and the electrode is inserted using the opposite hand in at least two sites on the muscle. This is then repeated on the opposite side. Although there is no standardized location for needle insertion into the levator ani muscles, one technique that has been proposed uses the ischial spine as a fixed reference point and samples two sites relative to this easily identifiable landmark.44 The first site is located 2 cm caudal and medial from the ischial spine. The second site is 2 cm further medial. The puborectalis muscle can be accessed from a perineal approach. A 75-mm electrode is required and is inserted approximately 1 centimeter posterior to the anus in the midline for a depth of 3–5 cm.
Lower Extremity
Bladder and bowel dysfunction are not uncommon when there are lesions involving the lumbosacral nerve roots and/or lumbosacral plexus. These lesions typically also affect innervation of the lower extremity. Therefore, whenever a patient's history and examination suggest lower extremity involvement as well as bowel and/or bladder dysfunction, the electrophysiologic evaluation should include the muscles of the lower extremity and the pelvic floor. A detailed description of the CnEMG evaluation of the lower extremity musculature is beyond the scope of this text. However, muscles that are often useful in such an evaluation include: quadriceps (L3, L4; femoral nerve); adductor longus (L4; obturator nerve); tibialis anterior (L4, L5; deep peroneal nerve); gastrocnemius (S1, S2; tibial nerve); gluteus maximus (S1; superior gluteal nerve); gluteus medius (L5; inferior gluteal nerve); adductor hallucis brevis (S1, S2; tibial nerve); and the paraspinal muscles from L3 to S1.
Interpretation
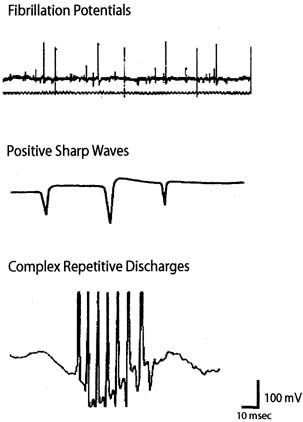
CnEMG is a valuable tool for evaluating lower motor neuron disease and muscle disease. Lesions involving the upper motor neurons in isolation have a normal EMG evaluation. The initial assessment in any CnEMG examination is an evaluation for insertional activity. The presence of insertional activity confirms that the electrode has been placed within the muscle. Absence of insertional activity with an appropriately placed needle electrode usually means a complete atrophy of the examined muscle. Once the needle has been properly placed, the patient is asked to completely relax the muscle being examined and the presence or absence of spontaneous activity is assessed. In the urethral sphincter, the anal sphincter, and the levator ani muscles, which all tonically contract even in the resting state, the only normal spontaneous activity is normal MUAPs. In limb muscles and the bulbocavernosus muscle, which do not tonically contract, there should be a complete absence of spontaneous activity at rest. The pelvic floor muscles achieve complete electrical silence during voiding and defecation. The tonic activity of the pelvic floor muscles are typically characterized by small-amplitude "low threshold" MUAPs that fire rather regularly at lower frequencies.45 Spontaneous activity that is found in pathologic conditions includes fibrillation potentials, positive sharp waves, complex repetitive discharges, fasciculations, myotonia, myokymia, and neuromyotonia (Fig. 7). Fibrillation potentials are biphasic muscle fiber potentials that occur spontaneously and typically have an amplitude of between 20 and 300 μV and a duration of less than 5 msec.38 They usually fire rhythmically at a rate of 2–20 Hz. Fibrillation potentials develop 2–30 days after an injury and can occur with a motor nerve lesion as well as with primary muscle diseases such as acute muscle injury, muscular dystrophies, and inflammatory myopathies. Positive sharp waves are biphasic waves with an amplitude of 20–500 μV and a 1- to 5-msec duration.38 They are more common than fibrillations and have a similar clinical significance. Complex repetitive discharges (CRD) are spontaneous high-frequency discharges with a regular firing pattern beginning and ending abruptly and can be bizarre in appearance. They can be found after chronic partial denervation, muscular dystrophy, inflammatory myopathies, and in some metabolic disorders.38 The striated urethral sphincter appears to be particularly likely to develop CRDs, which have been found in association with urinary retention in young women (Fowler's syndrome) and even in some neurologically normal women.46, 47
After a determination about spontaneous activity is made, the patient is asked to slightly contract the muscle being examined and attention is turned to MUAP analysis. The shape, amplitude, duration, number of phases, and stability of each MUAP should be assessed. Most EMG units have a trigger and delay mechanisms that allow MUAPs to be “frozen” for more careful analysis. Ideally, 20 or more MUAPs should be sampled for each muscle. This is often difficult for striated urethral sphincter, in which analysis of 10 MUAPs is often all that can be achieved because of the small size of the muscle.43 Muscles that have been denervated and reinnervated and muscles that are myopathic have distinct MUAP characteristics from those of normal muscle (Fig. 8). The morphology of a MUAP reflects, among other things, the number and local concentration of muscle fibers comprising a motor unit. After a neuronal injury, the muscle fibers innervated by that neuron begin to atrophy. Adjacent nerve fibers attempt to reinnervate these denervated muscle fibers, resulting in a neuron that now supplies a greater number of muscle fibers. This creates a MUAP with larger amplitude, longer duration, and a greater number of phases and turns. Because these changes depend on reinnervation by an adjacent motor neuron, large complex polyphasic MUAPs are not typically seen until 3–6 months after a nerve injury. In the setting of an acute nerve injury, reinnervation has not had time to occur and MUAP morphology is normal. Myopathic injury results in a loss of muscle fibers and therefore a motor unit with fewer muscle fibers. This results in a MUAP with shorter duration and smaller amplitude than normal.
After performing MUAP analysis, the patient is asked to increase her contraction effort and motor unit recruitment is assessed. In normal motor unit recruitment, there is a sequential increase in the firing rate of MUAPs as well as a sequential acquisition of new higher threshold MUAPs as the force of voluntary contraction increases. An interference pattern is called full or complete when the number and firing rate of the individual MUAPs becomes so great that they can no longer be distinguished and the baseline is obscured (Fig. 9). Recruitment is said to be normal when a complete interference pattern occurs at maximal effort. In neuropathic disorders, there are a reduced number of motor units so there is decreased recruitment and an incomplete interference pattern, although the remaining units fire rapidly. In myopathic disorders, there are reduced muscle fibers, but a normal number of motor units. A complete interference pattern is seen, but it occurs at much less than maximal effort and the amplitude to the MUAPs is reduced.
The chronicity of a nerve lesion can be determined by the CnEMG features present. In an acute nerve lesion, reinnervation has not occurred so the MUAPs have normal morphology. There are a reduced number of motor units, however, so recruitment is decreased. Between 2 and 30 days after an injury, spontaneous activity such as fibrillation potentials and positive sharp waves become apparent and insertional activity becomes longer. Three to 6 months after an injury, reinnervation has occurred so the MUAPs become larger and more complex. The location of a nerve lesion is determined by the pattern of muscles demonstrating denervation. For instance, neuropathic CnEMG findings in the external anal sphincter, but normal findings in the levator ani muscle and bulbocavernosus muscle suggest an isolated lesion involving the inferior rectal branch of the pudendal nerve. In contrast, if neuropathic findings were found in the external anal sphincter, the right levator ani muscle, the right gluteus maximus, and gluteus medius muscles, but not on the left side or in the L5, S1 paraspinal muscles, this would suggest a right-side lumbosacral plexus lesion.
Traditionally, CnEMG has depended largely on an examiners auditory and visual impression for analysis. In an attempt to improve the accuracy, reliability, and speed with which CnEMG can be performed, quantitative techniques have been developed. Although the first form of quantitative EMG (qEMG) was introduced in the 1950s, it did not become widespread until recently, when newer EMG machines became computerized.48 The technical aspects of performing a qEMG evaluation are identical to conventional CnEMG described. The difference is in the analysis, in which computerized digital analysis is performed on the collected electromyographic data, allowing a much more detailed evaluation of neuromuscular function in a shorter period of time. Two complementary forms of qEMG are: (1) analysis of multiple motor unit action potentials (multi-MUAP analysis) and (2) interference pattern analysis. In several recent studies, qEMG has been applied to the investigation of the pelvic floor muscles.27, 44, 49, 50, 51
In multi-MUAP analysis, the examiner identifies a period of crisp EMG activity during a slight-to-moderate muscle contraction. The computer uses a system of template matching to automatically extract, quantify, and sort any well-defined MUAPs according to their shape.52 This allows a rapid acquisition of data, such that the 20–30 MUAPs needed to adequately describe a muscle can be obtained in only a few minutes.44 Several MUAP parameters are then quantified, including amplitude, duration, area, number of phases, and number of turns, increase time, and spike duration. Thickness (area/amplitude) and size index (2*log [amplitude + area/amplitude]) are automatically calculated by the computer and assist in differentiating between normal and myopathic or neuropathic muscles.53 Normative data for the external anal sphincter and levator ani muscles have been published and are available for comparison.44, 49, 50
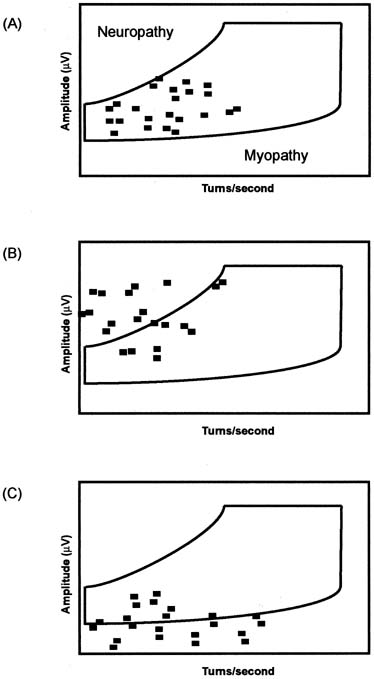
Interference pattern analysis is a broad term used to describe one of several automatic quantitative techniques for evaluating muscle recruitment. Computerized analysis of interference patterns is particularly useful because the electromyographic signal recorded at even a moderate contraction is too dense to be accurately assessed by visual inspection.54 The most popular technique for interference pattern analysis is turns/amplitudes cloud analysis (Fig. 10). This method of analysis is even faster than multi-MUAP analysis (2–3 minutes) and does not require a standardized force of contraction, eliminating an important source of variability.52, 54
Limitations
While CnEMG is the most valuable tool for investigating lower motor neuron damage of the pelvic floor, it has several limitations. The primary limitation of needle EMG techniques in the evaluation of women with pelvic floor dysfunction is the lack of experience on the part of most gynecologists and the limited access to qualified experts with interest in studies of pelvic floor muscles and sphincters.55 The role of CnEMG in the day-to-day evaluation and management of patients with urinary and fecal incontinence or other pelvic floor disorders has yet to be established, and thus far appears to be limited. Techniques for EMG of the pelvic floor muscles have yet to be standardized, although some progress has been made towards standardization of the evaluation of the anal sphincter.39, 50, 51 The adoption of qEMG techniques has improved the speed, accuracy, and reliability of conventional CnEMG evaluations, but widespread applicability remains limited because of the specialized equipment and expertise needed. The concentric needle electrode is invasive and can be painful, although it is usually well-tolerated in most patients.
SINGLE-FIBER ELECTROMYOGRAPHY
Single-fiber EMG (SfEMG) is a specialized test that allows sampling of individual muscle fibers within a motor unit. A SfEMG electrode is slightly narrower than a CnEMG electrode and consists of fine platinum or silver wire embedded in resin surrounded by an outer steel cannula. The inner wire serves as the recording electrode and exits a small aperture through the side of the electrode rather than at its tip. The pick-up area of a SfEMG electrode is considerably smaller than a CnEMG electrode (300 μm versus 0.5–1 mm), allowing it to record only one to three individual muscle fibers within a muscle unit. The primary application of SfEMG in neurophysiologic investigation is for the diagnosis of diseases of the neuromuscular junction, such as myasthenia gravis and Eaton–Lambert syndrome. This application is not used in the investigation of pelvic floor muscles, however. The principal SfEMG parameter that has been applied to the pelvic floor is the measurement of fiber density. Fiber density is the mean number of muscle fibers belonging to an individual motor unit axon per detection site. A finding of increased fiber density suggests reinnervation after a denervation injury. Reinnervation of denervated muscle fibers is achieved by collateral sprouting from adjacent uninjured axons, so that an individual motor unit axon will supply more muscle fibers (i.e., increased fiber density).
Technique/Interpretation
The measurement of fiber density requires sampling of at least 20 sites in a muscle.56 This usually implies four skin insertions of the electrode for each muscle with adjustments of the position of the electrode within each insertion site. Amplifiers are set so that low-frequency activity is eliminated (500 Hz to 10 kHz) and each muscle fiber appears as a biphasic positive–negative action potential.35 The number of muscle fiber action potentials present at each detection site is averaged to determine fiber density. The normal fiber density of most limb muscles is approximately 2. The average fiber density for the anal sphincter is 1.5.57 Fiber density increases with both age and parity. The principal use of SfEMG and fiber density measurements in the investigation of the pelvic floor has been in the evaluation for neurogenic fecal incontinence.57, 58, 59 An investigation of 57 patients with fecal incontinence demonstrated that mean fiber density as recorded by SfEMG correlated more closely with incontinence severity scores than did PNTML.60
Limitations
SfEMG is a sensitive test for detecting changes associated with reinnervation but is unable to detect changes associated directly with denervation such as abnormal insertional activity and spontaneous activity.35 It therefore is not useful in the acute setting because 3–6 months is required for reinnervation to occur. While it was used more commonly one to two decades ago, SfEMG is no longer widely used in neurophysiologic laboratories, except for the investigation of diseases of the neuromuscular junction.
NERVE CONDUCTION STUDIES
The asymmetrical distribution of ions between the inside (negative) and outside (positive) of a nerve cell creates a voltage potential that, when breached (depolarization), allows the flow of current (electrons). Ohm's law predicts that current, or nerve conduction, is inversely related to the resistance along the distance the current travels. On an anatomic level, resistance is determined by the diameter of a neuron, the presence (or absence) of myelination, and the distance between nodes of Ranvier (bigger distances yield faster conduction velocities). Studies of nerve conduction all rely on the elementary formula: rate = distance ÷ time. The clinical significance of nerve conduction studies draws from the fact that nerve injury affects the rate at which a nerve impulse travels. For example, because resistance would increase with a demyelinating injury, conduction velocity would decrease. In a typical nerve conduction study, a voltage potential is applied between two points of known distance across a single nerve fiber. The time taken for the current to move between the two points is determined and the rate or conduction is calculated from the aforementioned formula.
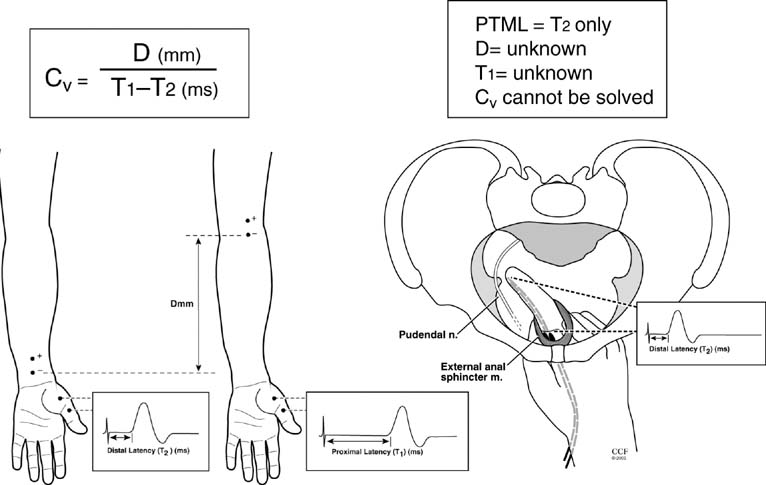
Outside of the pelvis, both motor and sensory nerve conduction studies are performed as part of routine neurophysiologic investigation. Conduction studies can aid in the diagnosis of peripheral neuropathy and distinguish between axonal loss and segmental demyelination. Conduction studies are also useful in localizing focal lesions to individual nerves, such as nerve entrapment syndromes (i.e., carpal tunnel syndrome). When applying these studies to pelvic floor function, two studies are performed: pudendal nerve terminal motor latency (PNTML) and perineal nerve terminal motor latency (PeNTML). The time it takes for an applied stimulus to generate a motor or sensory response over a set distance is called latency (Fig. 11). For motor responses, the recorded contraction of a muscle in response to an electrical stimulus is called a compound motor action potential (CMAP). The amplitude of the CMAP is determined by the number of intact motor nerve fibers. However, CMAP amplitude can vary with the configuration of the test electrodes limiting its diagnostic value. Nerve latency is determined by the fastest conducting fiber stimulated. Nerve cell depolarization is an all-or-nothing event; therefore, across any one nerve fiber only a finite voltage potential can be established. A nerve is composed of many fibers, some more conductive than others, if a stimulus does not depolarize all the fibers within the studied nerve, then the latency could be falsely prolonged. In Figure 11 the arrangement for measuring nerve conductions in the median nerve is displayed. Stimulating electrodes are placed distally and proximally and the CMAPs are recorded from the abductor pollicis muscle. The distance is calculated between the two points of stimulation. The conduction velocity is calculated as the quotient of this distance divided by the differences in latencies from the two stimulating sites. It is important to note that the time portion of this equation is the distal latency subtracted from the proximal latency. Subtracting the proximal latency removes the added conduction time attributed to the neuromuscular junction and muscle, and allows calculation of the conduction velocity of the nerve alone.
Technique
Currently most clinicians' use the St. Mark's disposable electrode to perform PNTML and PeNTML. Figure 12 shows the appearance of a St. Mark's electrode with its stimulating electrode at the tip of the second digit and receiving electrode at the base of the same digit. Commonly approached rectally, the stimulating tip is placed at the level of the ischial spine so as to stimulate the pudendal nerve. A receiving electrode situated at the level of the external anal sphincter detects the elicited CMAP. Stimuli of 0.1 msec duration are applied at 1-second intervals as the stimulating tip is positioned over the pudendal nerve. The ideal location is determined at the point the external anal sphincter muscle is felt to contract and compound motor action potentials are maximal. Perineal nerve terminal motor latency uses the same technique except that the receiving electrode is a modified bladder catheter that detects the CMAP associated with the striated urethral sphincter. The actual conduction velocity of a stimulus along these pelvic nerves is not calculated because the traveled distance is unknown; instead, only the latency is determined. Transvaginal stimulation using the St. Mark's electrode can also be used with normative values similar to that of the transrectal approach.61 Another method for measuring PNTML uses concentric needles placed in the bulbocavernosus or external anal sphincter muscles with bipolar stimulation of the perianal or perineal surfaces.62 Interestingly, this technique yields different results than the commonly used St. Mark's technique.
Interpretation
There is not a universally agreed latency that defines a patient as abnormal.63 Instead, each laboratory must establish its own normal values with dysfunction typically defined as any values greater than 2 standard deviations from the mean. These values should consider the differences that have been demonstrated with age and sex.64, 65 Additionally, each testing program should specify the patient positioning as this seems to affect the reproducibility of the technique.64 Generally, PNTML is considered prolonged (abnormal) when greater than 2.4 msec and PeNTML is considered prolonged when greater than 2.6 msec.
Limitations
PNTML is perhaps the most common electrophysiologic test used in clinical practice for the diagnosis and management of pelvic floor disorders. It is relatively simple and easy to learn, unlike many other neurophysiologic tests. Unfortunately, PNTML and PeNTML have significant limitations, causing some to advocate abandonment of these tests.66
Determination of nerve conduction requires knowledge of both the time it takes for a stimulus to generate a CMAP and the distance over which the stimulus travels. This distance should include only the studied nerve and not the neuromuscular junction or muscle, because passage through these structures would add time and obscure determination of conduction velocity. In measuring PNTML, the distance over which a stimulus is applied cannot be measured because of the inaccessible and circuitous route of the pudendal nerve. Moreover, the stimulus travels, not only through the pudendal nerve, but also through the neuromuscular junction and muscle. PNTML and PeNTML represent a distal latencies; no proximal latency can be measured for the pudendal nerve.
The differences in clinical information provided by PNTML and PeNTML and that of a typical nerve condition test used in the limbs cannot be underestimated. Any prolonged latency cannot be conclusively linked to nerve damage because conduction could be delayed because of difference in distance, neuromuscular junction transmission, muscle mass, and so on. The American Gastroenterological Association recognized this problem in their position statement concluding that PNTML cannot discriminate between muscle weakness caused by pudendal nerve injury and muscle weakness caused by muscle injury.66 Furthermore, they condemned PNTML for: (1) poor correlation with clinical symptoms and histologic findings; (2) lack of sensitivity and specificity for detecting external anal sphincter muscle weakness; (3) being operator-dependent; and (4) having no clear prognostic value in predicting surgical outcome.2
NERVE CONDUCTION STUDIES OF THE LOWER EXTREMITY
When clinical evaluation suggests the possibility of a lesion involving the lumbosacral nerve roots, lumbosacral plexus, or a generalized peripheral neuropathy, nerve conduction studies of the lower extremities should be performed. Motor conduction studies of the peroneal (L4, L5) and tibial nerves (L5, S1, S2) and sensory conduction studies of the deep and superficial peroneal (L4, L5) and sural (L5, S1) nerves can be performed. Detailed explanations of the technique and interpretation of these tests can be found in standard neurology and electrophysiology texts.
SACRAL REFLEXES
The electrophysiologic testing of sacral reflexes evaluates the spinal cord reflex arc of the pudendal nerve and/or the pelvic plexus. Like the clinical examination, the two reflexes most commonly tested during neurophysiologic testing of the pelvic floor are the bulbocavernosus reflex and the anal reflex. A normal reflex implies intact efferent and afferent innervation and normal integration of the two in the sacral spinal cord (S2–S4 level). The electromyographic assessment of the bulbocavernosus reflex has been found to be more sensitive than clinical assessment for detection of sacral neurologic disease.30 The bulbocavernosus reflex has also been called the clitoral-anal reflex, reflecting the site of the stimulating and recording electrodes, respectively.67 This reflex assesses the afferent and efferent branches of the pudendal nerve. It has been widely studied, is easy to learn and perform, and control data have been published by several groups.35
It is also possible to stimulate visceral afferent neurons in the lower urinary tract that travel within the pelvic plexus and cause a reflex contraction of the anal sphincter via pudendal efferent fibers. This autonomic/somatic reflex has been called the urethro-anal reflex and the bladder-anal reflex, depending on the stimulation site. The primary goal of testing these reflexes is to evaluate for pelvic plexus pathology.67 The urethro-anal and bladder-anal reflex are not as well-tested as the somatic pudendal reflexes and have yet to be widely adopted. A recent study, however, suggests that these tests may be useful in predicting the outcome of sacral neuromodulation.68
Technique/Interpretation
The bulbocavernosus reflex is assessed by applying an electrical, mechanical, or magnetic stimulus to the dorsal clitoral nerve and measuring the latency of the reflex response with recording electrodes within the anal sphincter or bulbocavernous muscle.35 The strength of stimulus affects the latency (stronger stimulus results in shorter latencies) so the stimulus is slowly increased until it is approximately three-times the patient's sensory threshold. In some subjects, a paired stimulus 3–5 msec apart may be necessary to obtain a response.35 The bulbocavernosus reflex has two components. The first component has mean latencies of approximately 33 msec and is thought to be an oligosynaptic response.35 The second component, which is not always demonstrable, has a latency of approximately 70 msec and is thought to represent a polysynaptic suprasacral response.67 Like PNTML, individual laboratories are expected to define there own normal values, but typically a latency for the first component of the reflex is considered abnormal if it is greater than 45 msec. Stimulation can be performed on either side of the clitoris, allowing evaluation of both the right- and left-side reflex arcs. The anal reflex is performed similarly to the bulbocavernosus reflex, but the stimulus is applied peri-anally. Normal latencies for the anal reflex are longer than those of the bulbocavernosus reflex because of the thinner myelinated nerve fibers in the afferent limb of the reflex arc.69, 70 A prolonged or absent latency in either the bulbocavernosus or the anal reflex implies a lesion somewhere along the reflex arc from the pudendal nerve to the conus medullaris.
Urethral stimulation for the urethro-anal reflex is applied via an electrode mounted on a Foley catheter. Bladder stimulation for the bladder-anal reflex is applied by moving this ring electrode into an empty bladder. The electrical stimulus is slowly increased until it is approximately three-times the patient's sensory threshold and latency is measured via a recording electrode as described. Normal latencies for these reflexes have been reported between 50 and 65 msec.67, 70 A prolonged or absent urethro-anal or bladder-anal reflex latency with a normal bulbocavernosus reflex implies a pelvic plexus lesion or autonomic neuropathy, such as is seen in people with diabetes.
Limitations
Of all of the sacral reflexes, only the bulbocavernosus reflex is widely used. It is a relatively easy test to learn and perform and (along with CnEMG) is probably the most useful and accepted of the neurophysiologic tests of the pelvic floor. That said, like all tests that rely on nerve conduction, it is not sensitive to detection of partial nerve lesions because the presence of only a few intact neurons can yield a normal latency. The urethral-anal and bladder-anal reflexes can be technically difficult to obtain and are not widely accepted. Furthermore, the sensitivity of these visceral-somatic reflexes for detecting pelvic plexus lesions is unknown.35
AUTONOMIC AND SENSORY TESTING
Evaluation of the sympathetic and parasympathetic innervation of the pelvic viscera is an important part of the evaluation of pelvic floor disorders. The integrity of the autonomic innervation of the bladder and ano-rectum is most frequently evaluated using urodynamics and anal manometry, respectively. These physiologic tests can provide information about visceral sensory innervation, as well as indirect evidence about the integrity and coordination of their sympathetic and parasympathetic innervations. A normal urodynamic or anal manometry evaluation implies a normally functioning autonomic innervation. However, abnormalities can reflect neurogenic or nonneurogenic dysfunction. When a pelvic plexus injury or a generalized autonomic neuropathy is suspected, methods to directly evaluate the integrity of the autonomic innervation of the pelvic viscera are needed.
Methods that have been suggested for directly evaluating the pelvic autonomic innervation include assessment of the urethro-anal and bladder-anal reflexes, the sympathetic skin response (SSR), and the quantitative sudomotor axon reflex test (QSART). The SSR and QSART both evaluate the sympathetic sudomotor (sweat gland) innervation. The SSR is elicited by electrical stimulation to mixed nerve in the upper or lower extremity or the genitalia. This results in a reflex stimulation of sweat production on the hands, soles, and genitalia. Sweat production is quantified by measuring changes in electrical resistance on the skin. The absence of sweat production is considered abnormal.35 QSART assesses the integrity of the axon reflex arc involved in sweat production. Postganglionic sympathetic sudomotor (sweat) fibers are activated by iontophoresis of acetylcholine into the skin. QSART has greater sensitivity and specificity than SSR and, where available, has largely replaced this older test.71 The application of these autonomic studies in the evaluation of patients with pelvic floor disorders is currently unknown and undergoing investigation.
Generalized autonomic neuropathy can be caused by diseases such as diabetes, amyloidosis, Guillain-Barré syndrome, alcoholism, nutritional deficiencies, and certain metabolic syndromes. Testing for generalized autonomic dysfunction usually involves monitoring heart rate and blood pressure changes in response to deep breathing, the Valsalva maneuver, and tilt testing.
Increasing evidence suggests that alterations in afferent signaling in the lower urinary tract may play a critical role in various lower urinary tract disorders, including overactive bladder, detrusor hyperreflexia and diabetic cystopathy.72, 73, 74 Afferent signals from the urinary tract are conducted by A-delta and C fibers in pelvic, hypogastric and pudendal nerves, which follow sympathetic and parasympathetic pathways. Normally A-delta fibers are activated by increasing tension in the bladder wall, while C fibers are not typically activated but begin firing in certain pathologic states. Several investigators have recently reported the feasibility of quantitative sensory testing of the lower urinary tract using Current Perception Threshold (CPT) testing.72, 74, 75, 76 CPT testing delivers sine-wave stimuli at frequencies of 2000, 250 and 5 Hz that have been shown to selectively stimulate large mylinated (A-beta), small myelinated (A-delta) and small unmyelinated (C) fibers, respectively.74 Minimum sensory thresholds can be assessed at each of these frequencies to assess for hyperesthetic (abnormally low) or hypoesthetic (abnormally elevated) sensory thresholds for each fiber type. CPT testing is used primarily for evaluating cutaneous sensory nerves and has only recently been applied to the lower urinary tract. Normative values for CPT testing for both the urethra and bladder have been published.75
CLINICAL CONDITIONS, PELVIC FLOOR DISORDERS, AND CHILDBIRTH INJURIES
Numerous studies demonstrate an association between vaginal childbirth and the subsequent development of pelvic floor disorders, including stress urinary incontinence, fecal incontinence, and pelvic organ prolapse.12, 77, 78, 79, 80 A recent large cohort study found that 50% of severe urinary incontinence was attributable to vaginal delivery.81 In addition to mechanical injury to the levator ani muscles, the urethral and anal sphincters, and pelvic connective tissue, many studies have demonstrated injury to the innervation of the pelvic floor after vaginal childbirth.77, 78, 79, 80, 81, 82 The pudendal nerve, being fixed at the level of the pudendal canal, is thought to undergo stretch or traction injury with the descent of the fetal head.82 Additionally, distal nerve branches may be compressed directly.
Neurophysiologic studies demonstrate prolonged PTML,78, 79, 80, 83 increased fiber density as measured by SfEMG,12, 77, 78, 80 and CnEMG79 evidence of pelvic floor denervation after vaginal delivery. Snooks and associates found evidence of pudendal neuropathy after childbirth in 42% of women.77 Two months after delivery, pudendal nerve function recovered in 60% of the women. This denervation injury leads to decreased levator ani and anal sphincter squeeze strength, which is thought to contribute to the development of pelvic organ prolapse, stress urinary incontinence, and fecal incontinence.13 Quantitative EMG of the anal sphincter using multi-MUAP analysis demonstrates evidence of subtle nerve injury in asymptomatic women 12 weeks postpartum after a single vaginal delivery that is not detectable by less sensitive measures like PNTML.84
Multiple successive vaginal deliveries are associated with increased incidence of pudendal nerve injury, while cesarean section performed before the descent of the fetal head appears to be protective.77, 78, 81 Women who undergo elective cesarean section do not demonstrate neuropathic injury, whereas women who undergo cesarean section for second stage arrest often do.81 Fynes and colleagues found prolongation of anal squeeze pressures and prolonged PNTML in women who underwent cesarean section after cervical dilation of 8 cm or greater.81 The relative contribution of pelvic floor denervation versus mechanical injury in the development of pelvic floor disorders after childbirth is currently unknown.
The primary role of neurophysiologic testing in the setting of childbirth is as a research tool. There is currently no clinical application of this technology in the postpartum woman except for the investigation of symptomatic pelvic floor disorders or neurologic dysfunction.
STRESS URINARY INCONTINENCE
Many studies have demonstrated an association between stress urinary incontinence and pudendal neuropathy with denervation of the urethral sphincter and/or levator ani muscles.12, 85, 86, 87, 88, 89 Investigators have used PNTML, PeNTML, SfEMG, and CnEMG to demonstrate this relationship. Hale and colleagues correlated histologic analysis of urethral biopsy specimens with CnEMG of the urethra and found that women with stress incontinence had greater histologic and CnEMG evidence of sphincter denervation than continent controls.89 Vaginal childbirth has often been implicated as the cause of this denervation injury, but aging and chronic straining may also contribute.13, 90 Alterations in pelvic floor muscle contraction patterns and reflex responses to cough have also been demonstrated using kEMG.91, 92 The relative contribution of denervation injury versus direct mechanical injury in the pathogenesis of stress incontinence is unknown. One report has even suggested that urethral sphincter myopathy may play a role in some patients with stress incontinence caused by intrinsic sphincteric deficiency.93
While neurophysiologic testing has contributed to our understanding of the pathogenesis of stress urinary incontinence, its role in the diagnosis or management of patients with uncomplicated stress incontinence is unknown and thus far limited. However, two studies have suggested that EMG may be useful in predicting the success of Burch urethropexy for treatment of stress incontinence. Kenton and associates used qEMG of the urethral sphincter preoperatively in 74 women undergoing Burch urethropexy and found that cases that were cured had greater muscle recruitment than cases that underwent unsuccessful surgery.1 Kjolhede and Lindhammar performed CnEMG on the pubococcygeus muscles of women after Burch urethropexy and found evidence of denervation significantly more often in the pubococcygeus muscles of women who had recurrent stress incontinence postoperatively.2
VOIDING DYSFUNCTION
The most common use of neurophysiologic testing in the evaluation of patients with voiding dysfunction is to identify detrusor sphincter dyssynergia. As previously described, this is the primary role of kEMG, which is performed to assess urethral relaxation/contraction during a urodynamic evaluation. Because true detrusor sphincter dyssynergia is very uncommon in patients without obvious neurologic dysfunction, it is probably unnecessary to perform kEMG during urodynamics if the clinical evaluation does not reveal pre-existing or suspected neurologic dysfunction.36
Another instance in which neurophysiologic testing appears to have clinical utility is in the evaluation of young women with urinary retention.35 In 1988, Fowler described a syndrome of painless urinary retention in premenopausal women often associated with polycystic ovary syndrome, so-called Fowler's syndrome.46 CnEMG of the urethral sphincter of these women reveal complex repetitive discharges (CRDs) and decelerating bursts. The urethral sphincter is often hypertrophied and overactive.94 The typical patient is in her mid-20s and presents with painless urinary retention with bladder capacity of greater than 1 L.95 A recent report suggests women with this condition respond well to sacral neuromodulation.96 The presence of CRDs in the urethral sphincter of a women with urinary retention should suggest Fowler's syndrome, but it is important to note that CRDs of the sphincter can be nonspecific and found in women with stress incontinence as well as voiding dysfunction.47
FECAL INCONTINENCE
In the diagnosis and management of pelvic floor disorders, neurophysiologic testing has perhaps been most often applied to the patient with fecal incontinence. Common clinical applications for neurophysiologic testing in women with fecal incontinence include: (1) sphincter mapping in a patient with a disrupted anal sphincter before surgical repair; (2) as a prognostic tool in patients with a disrupted sphincter before surgical repair; and (3) in the evaluation for neurogenic incontinence. As previously mentioned, anal sphincter mapping has largely been replaced by endoanal ultrasound for the identification and characterization of anal sphincter disruption. This is primarily because of decreased discomfort and the ability to evaluate the internal as well as external anal sphincter with ultrasound.40, 41 Several studies have found that women with fecal incontinence and a disrupted anal sphincter who have prolonged PNTML have a higher failure rate after surgical repair than women with normal latencies.97, 98, 99, 100 This has led many authors to advocate routine preoperative PNTML testing before anal sphincteroplasty. A number of studies have failed to confirm this relationship, however101, 102, 103, 104, 105, 106, 107, 108 (Table 5). These mixed results and the limitations of PNTML outlined previously have led the American Society of Gastroenterology to discourage the routine use of this test.66
Table 5. Prolonged PNTML and outcomes from anal sphincter surgery for fecal incontinence
| Success Rate (%) | |||||||
| Author, year | Procedure | Definition prolonged (ms) | n | Follow-up (mo) | Normal PNTML (%) | Prolonged PNTML (%) | p-value |
| Laurberg et al, 1988 | Overlapping | >2.4 | 19 | 9–36 | 80 | 11 | 0.05 |
| Wexner et al, 1991 | Overlapping | >2.1 | 16 | 3–16 | 92 | 50 | ns |
| Engel et al, 1994 | Ant plication | Not specified | 55 | 50 | — | — | ns |
| Londono-Schimmer et al, 1994 | Overlapping | Not specified | 94 | 12–98 | 55 | 30 | <0.001 |
| Simmang et al, 1994 | Overlapping | >2.3 | 10 | 6 | 100 | 67 | ns |
| Felt-Bersma et al, 1996 | Not specified | 18 | 3–39 | — | — | ns | |
| Nikiteas et al, 1996 | Overlapping | >2.5 | 42 | 12–36 | 73* | 60* | ns |
| Oliveira et al, 1996 | Anterior sphincteroplasty | >2.2 | 48 | 3–61 | 73 | 38 | ns |
| Sitzler and Thomson, 1996 | Not specified | 31 | 1–36 | 67 | 63 | ns | |
| Sangwan et al, 1996 | Overlapping | >2.4 | 15 | 4–32 | 100 | 14 | <0.005 |
| Chen et al, 1998 | Ant plication | >2.2 | 12 | 20–73 | 100 | 64 | ns |
| Gilliland et al, 1998 | Overlapping | >2.2 | 77 | 2–96 | 63 | 16 | <0.01 |
* Subgroup of 26 women with postobstetric injury
ns = not significant
Diagnosing neurogenic causes of fecal incontinence remains an important role for neurophysiologic testing. CnEMG and sacral reflex testing are valuable tools for this endeavor. The role of these tests as prognostic tools before surgery are currently unknown, however.
NEUROLOGIC CONDITIONS
Brain Lesions
Many conditions that affect the cerebrum can result in alterations in bowel and bladder function, including cerebrovascular accidents, dementia, tumors, hydrocephalus, multiple sclerosis, and lesions involving the anterior-medial frontal lobe. Alterations in continence can result from detrusor and rectal hyperreflexia, detrusor sphincter dyssynergia, and uninhibited sphincter relaxation.109, 110, 111 Additionally, conditions such as dementia and frontal lobe lesions can lead to socially inappropriate urination and defecation even with normally functioning lower urinary and gastrointestinal tract. Urodynamics and anal manometry in conjunction with kEMG can be helpful in characterizing the disturbances in these patients. CnEMG, nerve conduction studies, and sacral reflexes are typically normal.
Parkinson's Disease/Multiple System Atrophy
Parkinson's disease and multiple system atrophy (MSA; previously called Shy–Drager disease) are distinct neurologic diseases with different pathology; however, in their early stages they can often be difficult to differentiate.35 Bowel and bladder dysfunction are common in both conditions with as many as 50–80% of patients with either disease reporting bowel and/or bladder symptoms.112, 113 Urodynamic evaluation can reveal detrusor hyperreflexia, detrusor sphincter dyssynergia, or detrusor areflexia. Constipation is common in both conditions and is the result of decreased colonic motility, decreased rectal sensation, and paradoxical puborectalis contraction during defecation.114, 115 One feature that distinguishes the two is the neuronal degeneration of Onuf's nucleus in MSA. This results in EMG abnormalities of the urethral and anal sphincter including abnormal spontaneous activity and neuropathic MUAPs that are typically not present in patients with Parkinson's disease.35 This has led some to recommend CnEMG of the anal sphincter as the test to distinguish the two diseases, particularly in the first 5 years after onset of symptoms.116
Spinal Cord Lesions
Bowel and bladder dysfunction are common in patients with spinal cord lesions and represent a major source of distress for these patients.117 The timing and location of the lesion or injury are the major determinants in the nature of the dysfunction. Immediately after an acute injury, the spinal shock phase occurs, resulting in bladder and bowel areflexia. Within several weeks, the recovery phase begins, and if the injury is above the sacral cord, bladder activity often returns albeit uninhibited. In a study that included 284 patients with spinal cord injury, Kaplan found that in patients with cervical spine injuries, 15% had detrusor areflexia, 55% had detrusor sphincter dyssynergia, and 30% had detrusor hyperreflexia with a coordinated sphincter.117 In patients with a thoracic spine injury, 90% had detrusor sphincter dyssynergia. Lumbar spinal injuries resulted in detrusor hyperreflexia 30% of the time, detrusor sphincter dyssynergia in 30%, and areflexia in 40%. The relationship between the nature of bowel dysfunction and the location of spinal cord injury is less clear than with the bladder. Typically, patients have slow colon transit, increased rectal compliance, and decreased pelvic floor and anal sphincter function. The levator ani and anal sphincter may also demonstrate uncoordinated defecation, similar to detrusor sphincter dyssynergia. In a study of 115 patients after spinal cord injury, Glickman found that constipation occurred in 17%, weekly fecal incontinence in 11%, and occasional fecal incontinence in 50%.118 Almost all of the patients in this study had to use at least one therapeutic method to induce defecation.
Patients with spinal cord disease will demonstrate lower extremity hyperreflexia, sensory loss, and weakness consistent with the size and location of their injury. Urodynamics and anal manometry with kEMG are useful for characterizing the nature of their bladder and/or bowel symptoms. As injury to the spinal cord affects upper motor neurons rather than lower motor neurons, neurophysiologic studies such as CnEMG, nerve conduction studies, and sacral reflexes are usually normal unless the lower sacral cord (conus medullaris) is involved.
Conus Medullaris and Cauda Equina Lesions
Patients with lesions involving the conus medullaris or cauda equina classically present with so-called saddle anesthesia, lower extremity weakness, and bowel and bladder dysfunction. Lesions to the conus medullaris can result from L1/L2 disc disease, spinal stenosis, tumor compression, trauma, infarction, and multiple sclerosis. A common cause of cauda equina injury is central disk herniation of the lumbar spine, usually at the L4–L5 level. Central herniations, which represent less than 3% of herniations, preferentially compress the sacral nerve roots.110 Acute disk herniations are often dramatic and should be considered emergencies. Conditions such as spinal stenosis, ankylosing spondylitis, tumor compression, and chronic central disc herniation may present less dramatically and be a greater diagnostic challenge.
Because the conus medullaris represents the distal portion of the spinal cord and contains the anterior horn cells that supply the pelvic floor muscles and sphincters, lesions to this area result in a combination of upper and lower motor neuron symptoms. Typically, motor and sensory symptoms will be bilateral and symmetric. Sensory loss tends to be localized to the peri-anal region. In contrast, lesions of the cauda equina demonstrate only lower motor neuron symptoms that are often asymmetric and unilateral. Sensory loss is usually more variable and can be found from the soles of the feet to the perineum/perianal region. Radicular pain to the back, buttock, perineum, and lower extremity can be found with both lesions but tends to be more severe in cauda equina lesions. In both, weakness is often noted the gastrocnemius, hamstring, and gluteal muscles (S1, S2 innervated muscles) as well as the anal sphincter and levator ani muscles. There is a loss of anal sphincter resting tone and squeeze strength. Motor loss is symmetric in a conus lesion and often asymmetric in cauda equina lesion. Because of the upper motor neuron involvement in a conus medullaris lesion, the ankle reflex is increased and Babinski's sign is positive, while the knee jerk is typically normal. In contrast, in cauda equina lesions, the knee and ankle reflexes are normal and Babinski's sign is negative. The bulbocavernosus and anal wink reflexes are typically absent in both conditions.
Urodynamics often reveal absent bladder sensation and a hypoactive detrusor with elevated postvoid residuals. As a result, the patient often has overflow incontinence that is worsened by a concurrent loss of urethral tone. Anal manometry also reveals absent sensation and lack of ano-rectal tone. In conus medullaris lesions, findings of denervation in the pelvic floor muscles and sphincters are expected but are often not seen in the lower extremities as weakness in these muscles are typically caused by upper motor neuron injury. In cauda equina lesions, CnEMG often reveals denervation of muscles of the lower limbs and pelvic floor in an asymmetric pattern. Lower extremity motor nerve conduction studies demonstrate normal or prolonged conduction velocity with decreased amplitude and PNTML and PeNTML are prolonged. These changes are bilaterally symmetric with conus lesions and have variable bilaterally with cauda equina lesions. Sensory nerve conduction studies of the lower extremity are normal for both conus medullaris and cauda equina lesions, because the dorsal root ganglion and distal sensory axon are spared in either case. MRI of the spine is the radiographic test of choice with these presentations.
Lumbosacral Plexus Lesions
Lesions of the lumbosacral plexus can result from pelvic trauma, radiation, diabetes, malignant neoplasms (colorectal, breast, sarcomas, multiple myelomas), radical pelvic surgery, and, rarely, obstetric injury. Depending on the nature and location of the lesion, symptoms may be unilateral or bilateral and can include lower extremity weakness and sensory loss and pain in the lower back, hip, buttock, and leg. Bowel and bladder dysfunction are common, particularly if the pelvic plexus is involved. When lower sacral nerve roots are involved, perineal anesthesia and loss of levator ani and sphincter tone and squeeze strength are noted. Knee jerk and ankle reflexes may be normal or decreased and Babinski's sign should be negative. Urodynamics and anal manometry will often reveal an areflexic bladder and ano-rectum. Neurophysiologic testing is useful to confirm a lumbosacral plexopathy and distinguish it from a cauda equina lesion or generalized peripheral neuropathy. CnEMG will typically reveal denervation in the pelvic floor and lower extremity musculature in a distribution consistent with the nature of the lesion. Unlike cauda equina lesions, the L3–S1 paraspinal muscles should not be involved as these are innervated by the dorsal rami of the lumbosacral nerve roots and separate from the plexus. Lower extremity motor and sensory conduction studies will be abnormal in a distribution consistent with the lesion, and PNTML and PeNTML may be prolonged. Sacral reflexes will be unilaterally or bilaterally abnormal.
PERIPHERAL NEUROPATHY
Isolated injury to the distal pudendal nerve is the most common peripheral neuropathy seen in women with pelvic floor disorders. As described, distal pudendal neuropathy is commonly related to childbirth and has been implicated in the development of stress urinary incontinence, fecal incontinence, and pelvic organ prolapse. In an isolated pudendal nerve injury, CnEMG of the urethral and anal sphincters and/or bulbocavernosus muscle will reveal denervation, but the levator ani muscles and lower extremities will not. PNTML and PeNTML may be prolonged and sacral reflexes are often prolonged or absent. In rare cases, perineal sensation will be altered. Injury to the levator ani nerve is also common after vaginal delivery, and denervation of the levator ani muscles can often be found in conjunction with distal pudendal neuropathy.
Generalized peripheral neuropathies, including diabetic neuropathy, amyloidosis, Guillain-Barré syndrome, and some hereditary neuropathies can also cause bowel and bladder dysfunction. These disorders often affect the autonomic as well as the somatic nerves. Typically, clinical examination will reveal weakness and alterations in sensation of the lower extremities. If large fiber somatic nerves are involved, nerve conduction studies and CnEMG of the lower limbs will demonstrate the generalized, and typically symmetric, nature of these conditions.
PELVIC PLEXUS INJURY
Disruption of the autonomic pelvic plexus can occur with traumatic pelvic fractures, radical pelvic surgery, and, rarely, obstetric injury. Surgical procedures in women commonly implicated in pelvic plexus injury include abdominal perineal resection of the rectum for rectal carcinoma and radical hysterectomy for cervical carcinoma. Most commonly, the parasympathetic innervation is disrupted resulting urinary retention with elevated postvoid residuals. Occasionally sympathetic injury will result in loss of tone of the internal urethral sphincter and stress incontinence. Bladder and rectal sensation may also be decreased. Typically, bladder dysfunction is transitory, with normal voiding resuming within 6 months, although in some patients the dysfunction will be permanent. As mentioned, some generalized polyneuropathies, such as diabetic neuropathy, can cause autonomic dysfunction of the bowel and bladder.
On clinical examination, this type of injury is characterized by normal perineal sensation, normal levator ani and anal sphincter squeeze strength, and normal bulbocavernosus and anal wink reflexes. Anal sphincter resting tone may be decreased. Urodynamics and anal manometry will often demonstrate areflexia with or without sphincter incompetence. Autonomic testing such as urethro-anal and bladder-anal reflexes and QSART are typically abnormal. CnEMG of the pelvic floor muscles and sphincters, PNTML and PeNTML, and sacral reflexes will be normal if the injury is isolated to the pelvic plexus. In diseases like diabetes that can affect both autonomic and somatic nerves, neurophysiologic testing of the pelvic floor and lower limbs will reflect the degree of somatic involvement.
REFERENCES
Kenton K, FitzGerald MP, Shott S et al: Role of urethral electromyography in predicting the outcome of Burch retropubic urethropexy. Am J Obstet Gynecol 185:51-55, 2001 |
|
Kjolhede P, Lindehammar H: Pelvic floor neuropathy in relation to the outcome of Burch colposuspension. Int Urogynecol J 8:61-65, 1997 |
|
Sacral nerve stimulation results may be improved by electrodiagnostic techniques. Int Urogynecol J 11:352-357, 2000 |
|
Sasaki M: Morphological analysis of external urethral and external anal sphincter motoneurons of the cat. J Comp Neurol 349:269-287, 1994 |
|
Chalmers D, Swash M: Selective vulnerability of urinary Onuf motor neurons in Shy-Drager syndrome. J Neurol 234:259-260, 1987 |
|
Thor KB, Morgan C, Nadelhaft I et al: Organization of afferent and efferent pathways in the pudendal nerve of the female cat. J Comp Neurol 288:263-279, 1989 |
|
Schroder HD: Organization of the motoneurons innervating the pelvic muscles of the male rat. J Comp Neurol 192:567-587, 1980 |
|
Vanderhorst VG, Holstege G: Organization of lumbosacral motoneuronal cell groups innervating hindlimb, pelvic floor, and axial muscles in the cat. J Comp Neurol 382:46-76, 1997 |
|
Berglas BICR: Study of the supportive structures of the uterus by levator myography. Surg Obstet Gynecol 97:677-692, 1953 |
|
Lestar B, Penninckx F, Kerremans R: The composition of anal basal pressure. An in vivo and in vitro study in man Int J Colorectal Dis 4:118-122, 1989 |
|
Barber M, Bremer R, Thor K et al: Innervation of female levator ani muscles. Am J Obstet Gynecol 187:64-71, 2002 |
|
Smith AR, Hosker GL, Warrell DW: The role of partial denervation of the pelvic floor in the aetiology of genitourinary prolapse and stress incontinence of urine. A neurophysiological study Br J Obstet Gynaecol 96:24-28, 1989 |
|
Swash M, Snooks SJ, Henry MM: Unifying concept of pelvic floor disorders and incontinence. J R Soc Med 78:906-911, 1985 |
|
Percy JP, Neill ME, Swash M et al: Electrophysiological study of motor nerve supply of pelvic floor. Lancet 1:16-17, 1981 |
|
Snooks SJ, Swash M: The innervation of the muscles of continence. Ann R Coll Surg Engl 68:(1):45-49, 1986 |
|
Pierce LM, Reyes M, Thor KB et al: Innervation of the levator ani muscles in the female squirrel monkey. Am J Obstet Gynecol 188:1141-1147, 2003 |
|
McKenna KE, Nadelhaft I: The organization of the pudendal nerve in the male and female rat. J Comp Neurol 248:532-549, 1986 |
|
Roppolo JR, Nadelhaft I, de Groat WC: The organization of pudendal motoneurons and primary afferent projections in the spinal cord of the rhesus monkey revealed by horseradish peroxidase. J Comp Neurol 234:475-488, 1985 |
|
Toglia M, DeLancy JOL: Anal incontinence and the obstetrician-gynecologist. Obstet Gynecol 84:731-740, 1994 |
|
Sampselle CM, Brink CA, Wells TJ: Digital measurement of pelvic muscle strength in childbearing women. Nurs Res 38:134-138, 1989 |
|
Brink CA, Wells TJ, Sampsell CM et al: A digital test for pelvic muscle strength in women with urinary incontinence. Nurs Res 43:352-356, 1994 |
|
Romanzi LJ, Polaneczky M, Glazer HI: Simple test of pelvic muscle contraction during pelvic examination: Correlation to surface electromyography. Neurourol Urodynam 18:603-612, 1999 |
|
DeLancey JOL, Kearney R, Chou Q et al: The appearance of levator ani muscle abnormalities in magnetic resonance images after vaginal delivery. Obstet Gynecol 101:46-53, 2003 |
|
Lestar B, Penninckx F, Kerremans R: The composition of anal basal pressure. An in vivo and in vitro study in man Int J Colorecta Dis 4:118-122, 1989 |
|
Frenckner B, Ihre T: Influence of autonomic nerves on the internal anal sphincter in man. Gut 17:306-312, 1976 |
|
Kaushal JN, Goldner F: Validation of the digital rectal examination as an estimate of anal sphincter squeeze pressure. Am J Gastroenteerol 86:886-887, 1991 |
|
Weidner AC, Barber MD, Visco AC et al: Pelvic muscle electromyography of levator ani and external anal sphincter in nulliparous women and women with pelvic floor dysfunction. Am J Obstet Gynecol 183:1390-1401, 2000 |
|
Lind LR, Rosenzweig BA, Bhatia NN: Urologically Oriented Neurological Examination in Ostergard's Urogynecology and Pelvic Floor Dysfunction. 103-114, 5th edn. Philadelphia, Lippincott Williams & Wilkins, 2003 |
|
Rossolimo G: Der Anal Reflex: Physiologie und Pathologie. Neurol Cent Blatt Leipzig 9:257-259, 1891 |
|
Blaivas JG, Zayed AA, Labib KB: The bulbocavernosus reflex in urology: A prospective study of 299 patients. J Urol 126:197-199, 1981 |
|
Vodusek DB: Clinical neurophysiological tests in urogynecology. Int Urogynecol J 11:333-335, 2000 |
|
Workman D, Cassisi J, Dougherty M: Validation of surface EMG as a measure of intravaginal and intra-abdominal activity: Implications for biofeedback-assisted Kegel exercises. Psychophysiology 30:120-124, 1993 |
|
Burgio KL, Goode PS, Locher JL et al: Behavioral training with and without biofeedback in the treatment of urge incontinence in older women: A randomized controlled trial. JAMA 288:2293-2299, 2002 |
|
Mahajan ST, Fitzgerald MP, Kenton K et al: Concentric needle electrodes are superior to perineal surface-patch electrodesfor electromyographic documentation of urethral sphincter relaxation duringvoiding. BJU Int. 2006 Jan;97(1):117-20. |
|
Fowler CJ, Benson JT, Craggs MD et al: Clinical Neurophsiology in 2nd International Consultation on Incontinence. 391-424, Plymouth, Health Publication Ltd, 2002 |
|
Blaivas JG, Sinha HP, Zayed AA et al: Detrusor-external sphincter dyssynergia. J Urol 125:542-544, 1981 |
|
Rudy DC, Woodside JR: Non-neurogenic and neurogenic bladder: The relationship between intravesical pressure and the external sphincter electromyogram. Neurourol Urodynam 10:169-176, 1991 |
|
Aminoff MJ: Clinical Electromyography in Electrodiagnosis in Clinical Neurology. pp 243-259, 4th edn. New York, Churchill Linvingstone, 1999 |
|
Podnar S, Rodi Z, Lukanovic A et al: Standardization of anal sphincter EMG: Technique of needle examination. Muscle Nerve 22:400-403, 1999 |
|
Law PJ, Kamm MA, Bartram CI: A comparison between electromyography and anal endosonography in mapping external anal sphincter defects. Dis Colon Rectum 33:370-373, 1990 |
|
Tjandra JJ, Milsom JW, Schroeder T et al: Endoluminal ultrasound is preferable to electromyography in mapping anal sphincter defects. Dis Colon Rectum 36:689-692, 1993 |
|
Olsen AL, Benson JT, McClellan E: Urethral sphincter needle electromyography in women: Comparison of periurethral and transvaginal approaches. Neurourol Urodynam 17:531-535, 1998 |
|
Podnar S, Vodusek DB, Fowler CJ: Electrophysiology of the Anterior Pelvic Floor and Urinary Sphincter in The Pelvic Floor: Its Function and Disorders. 154-166., In Pemberton JH, Swash M, Henry MM (eds): Philadelphia, WB Saunders, 2002 |
|
Weidner AC, Sanders DB, Nandedkar SD et al: Quantitative electromyographic analysis of levator ani and external anal sphincter muscles of nulliparous women. Am J Obstet Gynecol 183:1249-1256, 2000 |
|
Enck P, Vodusek DB: Electromyography of pelvic floor muscles. J Electromyogr Kinesiol. 2006 Dec;16(6):568-77. Epub 2006 Oct 18. |
|
Fowler CJ, Christmas TJ, Chapple CR et al: Abnormal electromyographic activity of the urethral sphincter, voiding dysfunction, and polycystic ovaries: A new syndrome? Br Med J 297:1436-1438, 1988 |
|
FitzGerald MP, Blazek B, Brubaker L: Complex repetitive discharges during urethral sphincter EMG: Clinical correlates. Neurourol Urodynam 19:577-583, 2000 |
|
Buchthal F: Introduction to Electromyography. Copenhagen, Scandinavian Univeristy Press, 1957 |
|
Gilad R, Giladi N, Korczyn AD et al: Quantitative anal sphincter EMG in multisystem atrophy and 100 controls. J Neurol Neurosurg Psychiatry 71:596-599, 2001 |
|
Podnar S, Vodusek DB, Stalberg E: Standardization of anal sphincter electromyography: Normative data. Clin Neurophysiol 111:2200-2207, 2000 |
|
Podnar S, Vodusek DB, Stalberg E: Standardization of anal sphincter electromyography: Comparison of quantitative techniques of anal sphincter electromyography. Muscle Nerve 25:83-92, 2002 |
|
Stalberg E, Nandedkar SD, Sanders DB et al: Quantitative motor unit potential analysis. J Clin Neurophysiol 13:401-422, 1996 |
|
Sonoo M, Stalberg E: The ability of MUP parameters to discriminate between normal and neurogenic MUPs in concentric EMG: Analysis of the MUP “thickness” and the proposal of “size index.” Electroenecph Clinc Neurophys 89:291-303, 1993 |
|
Sanders DB, Stalberg EV, Nandedkar SD, Analsyis of electromyographic interference pattern. J Clin Neurophysiol 13:385-400, 1996;Coates KW: Physiologic evaluation of the pelvic floor. Obstet Gynecol Clin North Am 25:805-824, 1998 |
|
Stalberg E, Thiele B: Motor unit fibre density in the extensor digitorum communis muscle. J Neurol Neurosurg Psychiat 38:874-880, 1975 |
|
Neill ME, Swash M: Increased motor unit fibre density in the external sphincter muscle in anorectal incontinence: A single fiber EMG study. J Neurol Neurosurg Psychiat 43:343-347, 1980 |
|
Osterberg A, Graf W, Eeg-olofsson E et al: Results of neurophysiologic evaluation of fecal incontinence. Dis Colon Rectum 43:1256-1261, 2000 |
|
Kiff ES, Swash M: Slowed conduction in the pudendal nerves in idiopathic (neurogenic) fecal incontience. Br J Surg 71:614-616, 1984 |
|
Rogers J, Laurberg S, Misiewicz JJ et al: Anorectal physiology validated: A repeatability study of the motor and sensory tests of anorectal function. Br J Surg 76:607-609, 1989 |
|
Fowler AL, Mills A, Durdey P et al: Single-fiber electromyography correlates more closely with incontinence scoresthan pudendal nerve terminal motor latency. Dis Colon Rectum. 2005 Dec;48(12):2309-12. |
|
Cavalcanti GA, Manzano GM, Giuliano LM et al: Pudendal nerve latency time in normal women via intravaginal stimulation. Int Braz J Urol. 2006 Nov-Dec;32(6):705-11; discussion 712. |
|
Olsen AL, Rao SS: Clinical neurophysiology and electrodiagnostic testing of the pelvic floor. Gastroenterol Clin North Am 30:33-54, 2001 |
|
Tetzschner T, Sorensen M, Rasmussen OO et al: Reliability of pudendal nerve terminal motor latency. Int J Colorectal Dis 12:280-284, 1997 |
|
Lefaucheur J, Yiou R, Thomas C: Pudendal nerve terminal motor latency: Age effects and technical considerations. Clin Neurophysiol 112:472-476, 2001 |
|
Barnett JL, Hasler WL, Camilleri M: American Gastroenterological Association medical position statement on anorectal testing techniques. American Gastroenterological Association. Gastroenterology 116:732-760, 1999 |
|
Benson JT: Clinical Neurophysiologic Techniques in Urinary and Fecal Incontinence in Ostergard's Urogynecology and Pelvic Floor Dysfunction. 155-184, 5th edn. Philadelphia, Lippincott Williams & Wilkins, 2003 |
|
Benson JT: Sacral nerve stimulation results may be improved by electrodiagnositc techniques. Int Urogynecol J 11:352-357, 2000 |
|
Henry MM, Swash M: Assessment of pelvic floor disorders and incontinence by electrophysiological recording of the anal reflex. Lancet i:1290-1291, 1978 |
|
Vodusek DB, Janko M, Lokar J: Direct and reflex responses in perineal muscles on electrical stimulation. J Neurol Neurosurg Psychiat 46:67-71, 1983 |
|
Shimada H, Kihara M, Kosaka S et al: Comparison of SSR and QSART in early diabetic neuopathy-the value of length-dependent pattern in QSART. Autonom Neurosci 92:72-75, 2001 |
|
Snooks SJ, Setchell M, Swash M et al: Injury to innervation of pelvic floor sphincter musculature in childbirth. Lancet 2:546-550, 1984 |
|
Wyndaele JJ. Is abnormal electrosensitivity in the lower urinary tract a sign of neuropathy? Br J Urol 1993;72:575–9. |
|
Yokoyama, T., Nozaki, K., Fujita, O., Nose, H., Inoue, M., and Kumon, H.: Role of C afferent fibers and monitoring of intravesical resiniferatoxin therapy for patients with idiopathic detrusor overactivity. J Urol, 172: 596, 2004. |
|
Ukimura, O., Ushijima, S., Honjo, H., Iwata, T., Suzuki, K., Hirahara, N. et al.: Neuroselective current perception threshold evaluation of bladder mucosal sensory function. Eur Urol, 45: 70, 2004. |
|
Kenton K, Simmons J, FitzGerald MP et al: Urethral and bladder current perception thresholds: normative data in women. J Urol. 2007 Jul;178(1):189-92; discussion 192. Epub 2007 May 17. |
|
Wyndaele JJ, Van Eetvelde B, Callens D. Comparison in young healthy volunteers of 3 different parameters of constant current stimulation used to determine sensory thresholds in the lower urinary tract. J Urol 1996;156:1415–7. |
|
Snooks SJ, Swash M, Mathers SE et al: Effect of vaginal delivery on the pelvic floor: A 5-year follow-up. Br J Surg 1990;77:1358-1360, 1990 |
|
Allen RE, Hosker GL, Smith ARB et al: Pelvic floor damage and childbirth: A neurophysiological study. Br J Obstet Gynecol 97:770-779, 1990 |
|
Fynes M, Donnelly V, O'Connell PR et al: Cesarean delivery and anal sphincter injury. Obstet Gynecol 92:496-500, 1998 |
|
Fynes M, Donnelly V, O'Connell PR et al: The effect of second vaginal delivery on anal sphincter function and faecal continence: A prospective study. Lancet 354:983-986, 1999 |
|
Kamm MA: Obstetric damage and faecal incontinence. Lancet 344:730-733, 1994 |
|
Tetzschner T, Sorensen M, Rasmussen OO et al: Pudendal nerve damage increases the risk of fecal incontinence in women with anal sphincter rupture after childbirth. Acta Obstet Gynecol Scand 74:434-440, 1995 |
|
Snooks SJ, Swash M: Abnormalities of the innervation of the urethral striated sphincter musculature in incontinence. Br J Urol 56:401-405, 1984 |
|
Gregory WT, Lou JS, Stuyvesant A et al: Quantitative electromyography of the anal sphincter after uncomplicated vaginaldelivery. Obstet Gynecol. 2004 Aug;104(2):327-35. |
|
Snooks SJ, Badenoch DF, Tiptaft RC et al: Perineal nerve damage in genuine stress urinary incontinence. An electrophysiological study Br J Urol 57:422-426, 1985 |
|
Smith ARB, Hosker GL, Warrel DW: The role of pudendal nerve damage in the aetiology of genuine stress incontinence in women. Br J Obstet Gyncol 96:29-32, 1989 |
|
Anderson RS: A neurogenic element to urinary genuine stress incontinence. Br J Obstet Gynecol 91:41-45, 1984 |
|
Hale DS, Benson JT, Brubaker L et al: Histologic analysis of needle biopsy of urethral sphincter from women with normal and stress incontinence with comparison of electromyographic findings. Am J Obstet Gyencol 180: 342-348, 1999 |
|
Perucchini D, DeLancey JO, Ashton-Miller JA et al: Age effects on urethral striated muscle. I. Changes in number and diameter of striated muscle fibers in the ventral urethra Am J Obstet Gynecol 186:351-355, 2002 |
|
Takahashi S, Homma Y, Fujishiro, et al: Electromyographic study of the striated urethral sphincter in type 3 stress incontinence: Evidence of myogenic-dominant damages. Urology 56:946-950, 2002 |
|
Deffieux X, Hubeaux K, Porcher R et al: Pelvic floor muscle activity during coughing: altered pattern in women withstress urinary incontinence. Urology. 2007 Sep;70(3):443-7; discussion 447-8. |
|
Devreese A, Staes F, Janssens L et al: Incontinent women have altered pelvic floor muscle contraction patterns. J Urol. 2007 Aug;178(2):558-62. Epub 2007 Jun 14. |
|
Noble JG, Dixon PJ, Rickards D et al: Urethral sphincter volumes in women with obstructed voiding and abnormal sphincter electromyographic activity. Br J Urol 76:741-746, 1995 |
|
Swinn MJ, Fowler CJ: The clinical features of non-psychogenic urinary retention in young women (Fowler's syndrome). Neurourol Urodynam 17:304-305, 1998 |
|
Swinn MJ, Kitchen ND, Goodwin RJ et al: Sacral neuromodulation for women with Fowler's syndrome. Eur Urol 38:439-443, 2000 |
|
Laurberg S, Swash M, Henry MM: Delayed external sphincter repair for obstetric tear. Br J Surg 75:786-788, 1988 |
|
Londono-Schimmer EE, Garcia-Duerly R, Nicholls RJ et al: Overlapping anal sphincter repair for faecal incontinence due to sphincter trauma: Five year follow-up functional results. Int J Colorect Dis 9:110-113, 1994 |
|
Sangwan YP, Coller JA, Barrett RC et al: Unilateral pudendal neuropathy. Impact on outcome of anal sphincter repair Dis Colon Rectum 39:686-689, 1996 |
|
Gilliland R, Altomare DF, Moreira H et al: Pudendal neuropathy is predictive of failure following anterior overlapping sphincteroplasty. Dis Colon Rectum 41:1516-1522, 1998 |
|
Wexner SD, Marchetti F, Jagelman DG: The role of sphincteroplasty for fecal incontinence reevaluated: A prospective physiologic and functional review. Dis Colon Rectum 34:22-30, 1991 |
|
Engle AF, Kamm MA, Sultan AH et al: Anterior anal sphincter repair in patients with obstetric trauma. Br J Surg 81:1231-1234, 1994 |
|
Simmang C, Birnbaum EH, Kodner IJ et al: Anal sphincter reconstruction in the elderly: Does advancing age affect outcome? Dis Colon Rectum 37:1065-1069, 1994 |
|
Nikiteas N, Korsgen S, Kumar D et al: Audit of sphincter repair. Factors associated with poor outcome Dis Colon Rectum 39:1164-1170, 1996 |
|
Felt-Bersma RJ, Cuesta MA, Koorevaar M: Anal sphincter repair improves anorectal function and endosonographic image. A prospective clinical study Dis Colon Rectum 39:878-885, 1996 |
|
Oliveira L, Pfeifer J, Wexner SD: Physiological and clinical outcome of anterior sphincteroplasty. Br J Surg 83:502-505, 1996 |
|
Sitzler PJ, Thomson JP: Overlap repair of damaged anal sphincter. A single surgeon's series Dis Colon Rectum 39:1356-1360, 1996 |
|
Chen AS, Luchtefeld MA, Senagore AJ et al: Puendal nerve latency. Does it predict outcome of anal sphincter repair? Dis Colon Rectum 41:1005-1009, 1998 |
|
Sakakibara R, Hattori T, Yasuda K et al: Micturitional disturbance after acute hemispheric stroke: Analysis of the lesion site by CT and MRI. J Neurol Sci 37:47-56, 1996 |
|
Andrew J, Nathan PW: Lesions of the anterior frontal lobes and disturbances of micturition and defecation. Brain 87:233-262, 1964 |
|
Weber J, Dlanger T, Hanneqin D et al: Anorectal manometric anomalies in seven patients with frontal lobe brain damage. Dig Dis Sci 35:225-230, 1990 |
|
Sakakibara R, Hattori T, Uchiayama T et al: Urinary dysfunction and orthostatic hypotension in multiple system atrophy: Which is the more common ad earlier manifestation. J Neurol Neurosurg Psychiatry 68:65-69, 2000 |
|
Hattori T, Yasuda K, Kita K et al: Voiding dysfunction in Parkinson's disease. Jpn J Psychiatry Neurol 46:181-186, 1992 |
|
Stocchi F, Badiali D, Vacca L et al: Anorectal function in multiple system atrophy and Parkinson's disease. Mov Disord 15:71-76, 2000 |
|
Mathers S, Empster P, Swash M et al: Constipation and paradoxical puborectalis contractions in anismus and Parkinson's disease: A dystonic phenomenon? J Neurol Neurosurg Psychiatry 51:1503-1507, 1988 |
|
Vodusek DB: Sphincter EMG and differential diagnosis of Multiple System Atrophy. Mov Dis 16:600, 2001 |
|
Kaplan SA, Chancellor MB, Blaivas JG: Bladder and sphincter behavior in patients with spinal cord lesions. J Urol 146:113-117, 1991 |
|
Glickman S, Kamm MA: Bowel dysfunction in spinal cord injured patients. Lancet 347:1651-1653, 1996 |
|
Fowler CJ, Sakakibara R, Frohman EM et al: Cauda Equina Disorders in Neurologic Bladder, Bowel and Sexual Dysfunction. pp 63-74, Amsterdam, Elsevier Science, 2001 |