Uterine Artery Embolization and Minimally Invasive Techniques for Uterine Fibroids
Authors
INTRODUCTION
Until recently, the only definitive treatment options for symptomatic uterine fibroids were surgical, usually hysterectomy or myomectomy. Medical therapies such as oral contraceptives or gonadotropin-releasing hormone (GnRH) agonists were useful only for temporary relief of symptoms and not definitive therapy. GnRH agonists are effective in reducing the size of uterine fibroid as well as associated symptoms such as bleeding or pressure, but their use is currently limited by cost, the need for continuous therapy, and side effects.
Recently, several new minimally invasive techniques for treatment of uterine fibroids have been developed. Additionally, several promising medical therapies are being investigated. This chapter reviews alternative minimally invasive techniques of hysterectomy and myomectomy for the treatment of uterine fibroids
FIBROID BIOLOGY
Uterine leiomyomata or fibroids are the most common pelvic tumor in women of reproductive age, occurring in up to 77% of women if the uterus is extensively examined at autopsy.1 Fortunately, most of these tumors are small and usually asymptomatic. However, it has been estimated that between 20% and 50% of reproductive age women do have clinically symptomatic fibroids.2 Fibroids are more common in black women than in white women and account for approximately 30% of all hysterectomies, including 65.45% of hysterectomies in black women and 28% in white women.3 Leiomyomata are composed of smooth muscle cells and fibrous tissue with each fibroid is thought to develop from a single myometrial cell.4 Most uteri with fibroids contain multiple fibroids rather than a single tumor. This implies that each myoma developed independently from other fibroids.
As fibroids grow, they frequently undergo degeneration. This is generally believed to be because the fibroids outgrow their blood supply. Fibroids, unlike the rest of the uterine myometrial tissue, do not have an extensive collateral blood supply. In fact, fibroids have a very tenuous blood supply that makes them susceptible to ischemia. The blood supply of fibroids is primarily derived from one or two large arteries that penetrated into the central portions of the myoma and by smaller arteries that pass through the capsule and supply the peripheral portions of the tumor. These arteries are branches from the uterine arcuate arteries.
As fibroids grow in size, their blood supply has been shown to decrease.5 Consequently, larger fibroids are more likely to undergo degeneration than smaller ones. As such, it appears logical that the fibroids in a single uterus may be at different stags of development. As degeneration occurs, the proportion of living smooth muscle to nonliving tissue increases. The response of uterine fibroids to both hormonal therapies and embolization are thought to be affected, in part, by the amount of metabolic active living tissue comprising the fibroid. Those fibroids composed of more living tissue are generally thought to respond more readily to these therapies.
HORMONAL TREATMENT
The use of hormonal methods such as oral contraceptives, estrogens, and progestins for symptomatic relief of fibroids is well established, but the use of hormonal agents as a definitive treatment remains in its infancy. This section reviews agents that have been used and are being investigated as a treatment for leiomyomata.
GnRH AGONISTS
It has been well shown that the use of GnRH agonist produces a reduction in the size and vascularity of uterine fibroids. Leuprolide has FDA approval to treat anemia resulting from menstrual bleeding caused by fibroids. There are reports showing that preoperative use of GnRH agonists in both myomectomy and hysterectomy patients also reduce operative blood loss. Several studies have reported on fibroid regrowth after cessation of GnRH agonist therapy, but fewer reported on symptomatic recurrence or incidence of surgical treatment. However, given the small number of studies that report data on symptoms and additional treatment and the small size of the studies, accurate estimation of the risk of symptomatic recurrence is difficult. Given that regrowth is an almost universal occurrence after cessation of GnRH agonist therapy in premenopausal women, it is not surprising that recurrent symptoms, in some cases leading to myomectomy or hysterectomy, occur as well. However, it is unclear in what proportion of women symptoms recur, at what level of severity, and whether alternative treatments would be more or less likely to work after treatment with a GnRH agonist.
Most studies have described the short-term reduction in uterine or fibroid volume observed with GnRH agonist treatment. The average percentage reduction in uterine size is generally reported as approximately 50%. Fewer studies measured fibroid volume. Studies that reported both total uterine volume and fibroid volume found the percentage of reductions to be similar, suggesting that shrinkage occurs in fibroid tumors, as well as in the nonmyomatous uterus.6, 7, 8
Most of the reduction in fibroid and uterine volume occurred during the first month of treatment with the GnRH agonist, with diminishing reductions in size over subsequent months. The magnitude of change in uterine size during the first month was found to be a significant predictor of the ultimate response.9
Several studies continued to monitor uterine or fibroid size after GnRH agonist therapy was discontinued.8, 10, 11, 12, 13 These studies found that after GnRH agonists were stopped, uterine and fibroid sizes returned toward pretreatment values over several months.
Two studies assessed recurrence of symptoms after GnRH agonist treatment was discontinued.8, 12 One study reported only that there was a significant increase in the intensity of myoma-related symptoms during treatment, but the other quantified the proportion of women with recurrent symptoms. Although all women were symptomatic before treatment, 94% had complete resolution or improvement of their symptoms after 4 months of treatment with leuprolide. At 8–12 months after treatment was discontinued, 24% of women had recurrent symptoms, 64% remained asymptomatic, and 7.3% were lost to follow-up.
In summary, GnRH agonist treatment is associated with reduction of fibroid and uterine size, control of bleeding, and reduction of some symptoms; however, these drugs cause menopausal symptoms and, with long-term use, bone loss. Follow-up studies show that after treatment with GnRH agonists is stopped, there is regrowth of both the fibroid tumors and the uterus to near-pretreatment size, which is often associated with the return of fibroid-related symptoms.
Selective Estrogen and Progesterone Receptor Modulators
In the past decade, new compounds have been developed that selectively affect estrogen or progesterone receptors. These agents constitute a class of molecules that occupy receptor sites with resultant antagonist or agonist activity. They may act as an antagonist, blocking the initiation of intracellular events leading to estrogen or progesterone's hormonal effects (i.e., growth and maintenance of endometrial tissue) or may act as an agonist. The effect of these compounds is organ-dependent, with the same agent acting as an agonist on one target tissue and antagonist on another.
The antiprogestin agent RU-486 was tested in a prospective, nonrandomized, clinical trial comparing three doses.14 Limited data showed that, although all groups became amenorrheic, there was a smaller reduction in uterine size in the lowest-dose group (5 mg daily) compared with the higher-dose (25 mg or 50 mg daily) groups (25% reduction vs. 50% and 55% reduction; no p-value reported).
Currently, phase III trial of the progesterone receptor modulator, J867, is in progress. Initial reports indicate that this drug also produces shrinkage in uterine fibroids comparable with RU-486 and GnRH agonists.
These studies raise the possibility for the oral use of such agents for long-term treatment of symptomatic fibroids with minimal other systemic effects.
UTERINE ARTERY EMBOLIZATION
Transcatheter arterial embolization has recently been proposed as a definitive nonsurgical method for the treatment of symptomatic uterine fibroids. The use of transcatheter arterial embolization in obstetrics and gynecology is a well-established procedure. This procedure has been used extensively for hemorrhage from complications of pregnancy, surgical procedures, and pelvic carcinoma. In the early 1990s, Jacques Ravina and associates began using uterine artery embolization as a preoperative adjunct to decrease blood loss at myomectomy.15 In addition to reduced operative and postoperative blood loss, they noted that the uterine fibroids decrease in size and that women who had been treated for acute life-threatening bleeding also had resolution of their bleeding symptoms. Subsequently, this group treated 16 patients who were considered at too great of a surgical risk for hysterectomy with uterine artery embolization alone.15 Fourteen of the 16 patients (87.5%) were able to avoid any subsequent surgery. Uterine volume decreased an average of 36% in those patients available for follow-up with ultrasonography. The authors concluded that uterine artery embolization was a definitive procedure for symptomatic fibroids equal to currently available surgical methods.
Biologic Mechanism of Uterine Artery Embolization of Fibroids
Once embolic material is injected into the uterine arteries, it is carried along by blood flow to smaller and smaller branches. When enough embolic material is present to significantly slow blood flow in an arterial branch, clotting occurs. As smaller arteries clot, the flow in feeding arteries also slows, and they also clot. The flow of blood per unit volume of tissue is generally greater to the uterine myometrium than to fibroids. Consequently, more embolic particle will flow to the myometrium than the fibroids.
Because of the extensive collateral blood supply to the uterus, occlusion of one uterine artery dose not produce significant ischemia of either fibroids or myometrium. Once both uterine arteries are occluded, both myometrium and fibroids become ischemic. The resultant hypoxia triggers recruitment of other collateral blood flow from the ovarian arteries and other collateral vessels. Generally within 24 hours, enough blood flow has been established to relive most of the ischemia to the uterine myometrium.
Although the mechanism is somewhat unclear, myometrium appears to be much more tolerant of the ischemia produced by uterine artery embolization than fibroids. There is speculation that fibroids may be less able to lyse clots in their feeding vessels, less able to recruit additional blood flow, or may be inherently more susceptible to hypoxia than myometrium. As result, fibroid tissue dies while myometrium is spared. The resulting decrease in volume of any particular fibroid is dependent on the proportion of the fibroid that is made up of living tissue and the proportion that is nonliving degenerated tissue.
Procedure of Uterine Artery Embolization
Uterine artery embolization is performed in an angiographic suite using fluoroscopic guidance. The suite is usually located in a hospital, but the procedure has been performed in outpatient surgery centers. The procedure is usually performed with the patient under conscious sedation rather than general anesthesia.
The procedure begins with the percutaneous puncture of either the right or the left common femoral artery. After the area of the groin overlying the planned puncture is anesthetized with local anesthesia, the common femoral artery is punctured with an 18-gauge needle and a guidewire placed into the artery. The needle is then replaced with a sheath through which catheters may be placed into the artery.
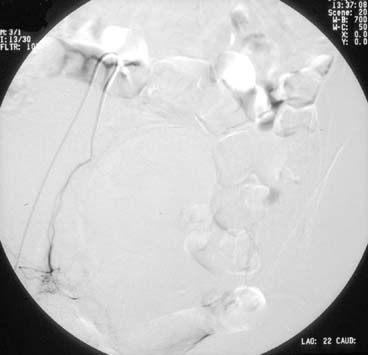
A pelvic arteriogram is generally performed to delineate the arterial anatomy. Embolization of the uterine artery contralateral to the access site is usually attempted first. A catheter is directed over the guidewire, up the external iliac artery, to the bifurcation of the abdominal aorta. Using a steerable guidewire, the catheter is directed down the common iliac artery and then down the hypogastric artery and into the origin of the uterine artery. Angiography is used to aid in guiding the catheter into the proper position (see Figs. 1 and 2). Embolic material is mixed with contrast material and injected. Repeat injections continue until blood flow significantly slows or stops (see Fig. 3). The catheter is then withdrawn and the procedure repeated on the ipsilateral uterine artery (see Fig. 4).
After the procedure, pressure is held over the puncture site for 10–20 minutes. The patient is then instructed to keep the leg on the side of the puncture straight for 6 hours. Generally, patients who have uterine artery embolization performed for fibroids are admitted overnight for pain control. Occasionally some patients will require longer periods of hospitalization to achieve adequate pain control.
EMBOLIC MATERIAL
The most common embolic material for uterine artery embolization is polyvinyl alcohol or PVA. Despite a common misperception among gynecologists, PVA is not a liquid but a radiolucent plastic that is not soluble in water. Blocks of the solid polymer are ground to various sizes for use as an embolic agent. The particles produced are very irregular in shape and have sharp jagged edges. When injected into arteries, the particles attract platelets readily and clump together, producing blood clots. Even small PVA particles (100 μm) are fairly large compared with red blood cells (8 μm), but because of the clumping produced, single particles do not occlude arteries equal to their size. The ideal-size PVA particle to use for uterine artery embolization is uncertain, with different centers preferring different size particles. Some groups prefer small particle in the range of 150–500 μm, others 350–500 μm particles, and yet others prefer relatively large (500–710 μm ) particles.16 Although PVA particles do not dissolve, they do not occlude arteries permanently because significant recanalization can occur. Follow-up ultrasound has shown normal uterine artery flow several weeks after the procedure.17
Another common embolic agent is absorbable gelatin sponges. Because the material is absorbable, it is viewed as a temporary embolic agent. Studies following-up femoral artery occlusion in dogs showed substantial recanalization occurred within 2 weeks and total recanalization in 2 months.18 Because absorbable pledgets are much larger than even large PVA particles, these pledgets should block larger more proximal arteries than PVA particles, which are believed to block smaller more distal arteries.
It remains uncertain whether distal or proximal uterine artery occlusion is better. Theoretically, if occlusion is too distal, then excessive uterine tissue would be destroyed along with the fibroid. There is some belief that more distal uterine artery occlusion produces more postprocedural pain caused by the increased tissue ischemia. Conversely, if occlusion is too proximal, the collateral blood supply of the uterus may result in minimal fibroid destruction. In one publication, fibroid shrinkage was thought to be greatest with smaller PVA particles, but it was believed there was a corresponding increase in postoperative pain and complications.19
Other embolic materials available for embolization are stainless steel pellets or coils, metal filings, silicone spheres, and bucrylate. These materials are rarely used as the primary embolic agent in uterine artery embolization for fibroids. However, some centers used stainless coils to further occlude the uterine arteries after PVA is used as the initial embolic agent.
COMPLICATIONS
Technical failure, defined as the inability to successfully catheterize and embolize the right and left uterine arteries, occurs in approximately 1–2% of cases. Procedure-related complications include groin hematoma, infection at the puncture site, guidewire perforation of the arteries, reactions to iodinated contrast material, thromboembolic events, and embolization of nontarget tissues.
Overall Complication Rate
A recent survey of interventional radiologists in the United States reported 4165 procedures performed by 408 interventional radiologists.20 There were 25 major complications requiring gynecologic surgery with 30 days of the embolization procedure resulting in a major complication rate of 1 in 167 cases. Although no fatalities were reported in the United States survey, two fatalities have been reported in Europe. In Italy, one fatality after uterine artery embolization with PVA particles was attributed to a pulmonary embolus believed to have originated from a clotted pelvic vein. In Britain, a second fatality occurred from Escherichia coli sepsis and disseminated intravascularly. An estimated mortality rate derived from available data has been calculated to be 2 in 5365 or 0.4 in 1000 uterine artery embolization procedures.20
Ovarian Failure
Ovarian failure may occur after uterine artery embolization. This complication has been reported to occur as often as 5% in one study, but other studies have estimated only a 1–2% incidence.16, 21 The cause of this ovarian failure is unknown, but most likely from ovarian embolization caused by embolic material passing through the utero-ovarian vasculature. The ovarian artery normally gives off a small communicating artery that connects with the superior branch of the uterine artery of the same side. Theoretically, embolic material could pass into this system and result in occlusion of the ovarian arteries. The presence of embolic microspheres within the ovarian arterial system has been demonstrated after uterine artery embolization in at least one patient.22
Postprocedural Amenorrhea
Amenorrhea after uterine artery embolization, both transient and permanent, has been reported.23 The incidence has ranged from 2% to 5%. However in the largest long-term series available from the Fibroid Registry, Goodwin reported on 2112 patients of which 1916 remained in the study at 36 months and 1278 completed the study questionnaire.24 At 36 months, 28.6% of the 1278 patients were amenorrheic (excluding those who underwent hysterectomy.
In some of amenorrheic patients, hormonal and clinical findings have been consistent with ovarian failure and presumed menopause, possibly as a result of ovarian failure. In other patients, there was no evidence of ovarian failure. The amenorrhea in these patients may have been as a result of decreased uterine vasculature. Although amenorrhea can be viewed as a successful outcome by many patients, this would not be the case in patients desiring to maintain their fertility.
Postprocedural Pain
Almost all women undergoing uterine artery embolization will experience moderate-to-severe pain after the procedure. The most intense pain usually subsides within 24 hours but may last for more than 2 weeks in 5–10% of patients.25 Persistent pain months after the procedure has also been reported in a patient with a large necrotic intracavitary fibroid.26
The source of acute pain after uterine artery embolization is generally attributed to degeneration of leiomyomata. However, Burbank and Hutchins have argued that the pain is caused by myometrial ischemia and not fibroid degeneration.20 These authors give several observations that seem to support this conclusion. Women who have little or no fibroid shrinkage after embolization still experience postprocedure pain similar to those who do have significant fibroid shrinkage. Secondly, fibroids vary in size and one would predict that those women with larger fibroids would experience more pain after embolization than patients with smaller fibroids. In reality, all patients generally experience moderate to severe pelvic pain within the first 24 hours postembolization. Patients with larger uterine volumes or larger individual fibroid have not been shown to experience greater pain than women with smaller uterine volumes or smaller individual fibroids. Third, there is a negative correlation between fibroid blood supply as demonstrated by gadolinium enhancement on MRI and pain experience after embolization. Theoretically, if a fibroid receives more blood supply, it should also receive more embolic material than the surrounding myometrium and thus more ischemia. Patients who have been treated with GnRH agonists before embolization do not have less postprocedure pain compared with control groups who did not receive GnRH agonists despite a two-fold difference in uterine volume. Also, patients with adenomyosis who have underwent uterine artery embolization report pain similar to patients treated for leiomyomata. Lastly, it has been shown that soon after uterine artery embolization, there is no blood flow to either the myometrium or the fibroids as demonstrated by the gadolinium-enhanced MRI, but 1 week later the myometrium is well-vascularized while the fibroids remain ischemic. All these arguments support the theory that in most patients, pain after uterine artery ligation is related to myometrial ischemia and not fibroid degeneration.
Postembolization Syndrome
Within 2–3 days of the procedure, up to one-third of women will have fever and leukocytosis, sometimes as high as 30,000.16 This may be accompanied by nausea, emesis, malaise, and anorexia. This constellation of symptoms has been termed postembolization syndrome and is generally thought to reflect infarction and necrosis of the myomas and not infection. However, cases of postprocedural endometritis that eventually required hysterectomy have occurred. In some cases, a lack of collateral blood flow to the uterus has resulted in persistent pelvic pain and required hysterectomy. Rarely, uterine gangrene may occur and require immediate hysterectomy.
Subsequent Surgical Procedures
In the previously noted long-term outcome data from the Fibroid Registry, 2.82% of patients underwent subsequent myomectomy, 9.79% hysterectomy, and 1.83% repeat uterine artery ligation.24 The authors noted that this rate was lower than reported in some studies and may reflect an underreporting because of patients lost to follow-up
TECHNICAL ISSUES OF UTERINE ARTERY EMBOLIZATION
Uterine Size
Some authors have questioned whether there is an upper limit on uterine size that is appropriate for uterine artery embolization. Early studies found no correlation between uterine volume and success of treatment. Recently, an abstract by McLucas and associates looking at the effect of uterine size on outcome reported their results in 300 patients.27 Fifteen percent of patients had treatment failures as defined by either continued symptoms or patients who would not recommend the procedure to others. Uterine volume itself was not a predictor of failure, but failure was more common if the largest fibroid was greater than 8.7 cm in diameter. For each additional 1-cm increase in diameter, there was a corresponding 10% increase in the failure rate.
Submucosal Fibroids
One of the complications associated with uterine artery embolization for fibroids is the subsequent vaginal expulsion of submucosal fibroids. Although there is no proof, it has been suggested that the pretreatment presence of submucous fibroids may increase the subsequent failure rate of uterine artery embolization. As a result, some authors advocate hysteroscopic resection of these fibroids as the preferable approach to the patient with symptomatic submucosal fibroids.28
Adenomyosis
Adenomyosis of the uterus is a condition that may mimic the symptoms of uterine fibroids. This condition is associated with uterine enlargement, dysmenorrhea, and abnormal bleeding. Because these symptoms are similar to uterine fibroids, it may be misdiagnosed. In patients with pure adenomyosis, ultrasonography should be able to note the absence of uterine fibroids, but because fibroids are so common, it is not unusual to find patients with adenomyosis who also have fibroids. Unfortunately, there is no way to accurately make a diagnosis in these patients. Ultrasound has been reported to have a sensitivity of approximately 80% in diagnosing adenomyosis while MRI has an even greater sensitivity as well as superior specificity. However, none of these modalities is 100% accurate.
The accurate diagnosis of adenomyosis is of concern because theoretically, this condition responds less favorably to uterine artery embolization. Several preliminary reports have shown that adenomyosis does appear to be associated with increased treatment failures, and some centers now consider adenomyosis a contraindication to uterine artery embolization.16 However, reports of successful treatment of patients with adenomyosis have also been reported. In one recently presented abstract, 14 women with adenomyosis confirmed by MRI were treated with uterine artery embolization. Improvement in symptoms occurred in 10 of 11 patients.29 At 6 months, the average uterine volume had also decreased by 47%.
Currently, no definitive statements can be made about the effect of adenomyosis on failure rates after uterine artery embolization. Based on limited data, adenomyosis probably does increase the failure rate after uterine artery embolization by an undetermined amount but probably should not be considered an absolute contraindication as long as this association is understood.
Pregnancy after Uterine Artery Embolization
Many women with symptomatic fibroids who desire future fertility see uterine artery embolization as an option that avoids the surgical complications and problems of myomectomy. Although uterine artery embolization for postpartum hemorrhage appears to have no adverse effect on future fertility, the effect of uterine artery embolization for fibroids on subsequent fertility remains unknown. Although the procedures are technically similar, the effect of pregnancy-induced changes in the vasculature of peripartum uteri may significantly alter the effect of embolization on the uterine myometrium. Questions also remain whether the procedure could predispose to uterine rupture with subsequent pregnancy or if the procedure itself could decrease fertility through an effect on endometrial perfusion resulting in decreased implantation or survival of early embryos. Likewise, fertility could be affected by a decrease in ovarian function or production of frank ovarian failure.
Ravina reported on nine women with 12 pregnancies occurring after uterine artery embolization.30 Five early miscarriages occurred. Of those pregnancies continuing, three premature births and one case of preeclampsia resulted.
In a review of the literature Hurst and associates reported a total of 32 pregnancies occurring in 1730 patients who had undergone uterine artery embolization for fibroids.16 Unfortunately, no study to date has been able to accurately identity the number of women attempting pregnancy after this procedure, so the true denominator of women trying to conceive is unknown. Likewise, no study has evaluated the cycle fecundity rate of patients trying to conceive after uterine artery embolization.
Forman and associates did identify 17 women of 192 patients undergoing uterine artery embolization who desired pregnancy after the procedure.31 Six of those patients had complications as a result of the procedures that were expected to reduce their fertility. The authors conclude from this that the current literature supported myomectomy as a better option for those patients younger than age 40 who desired pregnancy.
Because of these concerns, some centers do not offer this procedure to women who wish future pregnancy or reserve it for individuals when there is no alternative to hysterectomy or repeat myomectomy. Until more studies are available to delineate the true fecundity as well as the rate of pregnancy complication, such as spontaneous abortion and premature delivery after uterine artery embolization for fibroids, it seems reasonable that patients deserving future fertility should at least be informed of the minimal data currently available on pregnancy outcome.
Overall Results of Uterine Artery Embolization
In an analysis of the major studies for uterine artery embolization for fibroids, Hurst and associates reviewed articles involving 772 patients.16 Follow-up was from 2 months to 1 year. The percent of patients experiencing a decrease in abnormal bleeding ranged from a low of 20% to a high of 89%, with the majority of studies showing decreases at approximately 80% to 85%. Unfortunately, most studies relied on the patient's subjective impression of their bleeding as an outcome measure. Therefore, these series are subject to several potential biases regarding the improvement in uterine bleeding.
The decrease in uterine volume after uterine artery embolization ranged from 35% to 69% with most studies averaging approximately 50%. Because the follow-up time was relatively short, there is the possibility that a continued decrease in uterine volume will be seen over time. Also, because follow-up is relatively short, it remains to be determined whether this procedure will have long-term effect and reduce the recurrence and growth of new myomas.
OTHER MINIMALLY INVASIVE TECHNIQUES
High-Intensity Ultrasound
An initial study in nude mice reprorted in 2000 demonstrated that fibroids could be successfully treated with high-intensity focused ultrasound (HIFU).32 In this study, researchers treated 28 mice with fibroid tumors with HIFU equipment. Diagnostic use of ultrasound delivers ultrasonic wave intensity levels less than 0.1 watts/cm2, while HIFU can deliver levels up to 10,000 watts/cm2. After treatment, all of the mice in this study experienced tumor reduction and 87% experienced this reduction within 4 weeks.
Subsequent work in humans, led to the development of the Exablate 2000 ( inSightec, Tirat Carmel, Israel) which was FDA approved for treatment of fibroids in 2004. The technology uses Magnetic Resonance imaging to focus the high intensity ultrasound waves. Treatment last 2–4 hours. Patient outcomes from the FDA pivital trial showed reduction in fibroid volume of 13.5% at 6 months and 9.4% at 12 months using an intent-to-treat analysis.33, 34 Despite the small reduction in volume, 71% reached their target symptom reduction at 6 months and 51% at 12 months. By 12 months, 21% of women had underwent some form of additional surgical therapy
Myolysis
Myolysis or myoma coagulation is a minimally invasive technique for leiomyoma uteri. The procedure originally used a bare Nd:YAG laser fiber to pierce the myoma and to necrose and destroy stromal tissue. This procedure fell out of favor because of the formation of dense pelvic adhesions in many patients. Subsequently, Goldfarb modified the procedure in 1992, using 5-cm bipolar needle and a circumferential technique to spare severe serosal damage and reduce adhesion formation.35
Generally fibroids greater than 10 cm or a uterus greater than 14 weeks has generally been considered relative contraindications to myolysis. However, GnRh agonists may be used to reduce the size of fibroids that otherwise would not be suitable for myolysis. Even with smaller fibroids, the use of GnRH agonist for 3 months is recommended to decrease both the size and vascularity of the fibroids. A trial of GnRH agonist will also predict the likely response to myolysis. Patients who do not have a size reduction in the myoma or a decrease in symptoms such as pelvic pressure will likely have unsatisfactory response to myolysis as well. Goldfarb also recommends the use of a broad-spectrum antibiotic before surgery. There are, however, no data to support or refute this recommendation. The procedure, as performed by Goldfarb, uses three suprapubic puncture 5-mm trocars and myoma corkscrews to stabilize the fibroid.
Original Technique with the Nd:YAG Laser
The procedure is generally performed with 40–50 watts of continuous power using bare Nd:YAG laser fibers of 600 or 1000 μm.36 To avoid damage to the bowel and bladder during coagulating the myoma, the position and depth of the fiber in the myoma must be known at all times. Unlike bipolar myolysis in which the needles are inserted into the myoma before activation of power, the laser must be activated before touching the fibroid to achieve penetration into the myoma. The laser tip is advanced into the leiomyoma and then removed slowly to achieve maximum coagulation. To cool the fiber tip, fluid is used continuously. Excess blood is suctioned and tissues are thoroughly lavaged. Nd:YAG laser power more than 40 watts causes vaporization as well as coagulation, but the use of these higher powers result in a more rapid completion of the procedure.
Myomas are generally coagulated in both the anterior and horizontal plane. The use of an operating laparoscope facilitates the performance of the horizontal punctures and the myolysis of posterior fibroids. Because the laser fibers produce a coagulation zone of 5 mm, punctures are repeated in a drilling fashion at multiple concentric sites at 5-mm intervals.
A 5-cm leiomyoma takes approximately 10 punctures per diameter, or a total of 50–75 punctures. An 8-cm leiomyoma can be thoroughly coagulated in approximately half an hour. At the end of the procedure the surface of the leiomyoma appears blanched and scarred.
The Circumferential Technique
The multiple serosal punctures required to preform myolysis results in formation of significant pelvic adhesions. As an alternative, Goldfarb introduced the circumferential technique.35 The goal of this technique was to destroy the vasculature of the fibroid and indirectly results in degeneration and shrinkage of the fibroid rather than directly destroy the myoma. Bipolar 5-cm needles are used in this method rather than the Nd:YAG laser. The needle are manufactures in a 30-cm and 45-cm overall length. The longer instrument is designed for use through the operating laparoscope. The needles are sequentially inserted into the base of the myoma in a circumferential manner. Fifty to 75 watts of coagulating current is then applied until the desired endpoint of cyanosis of the myoma is achieved. This generally occurs in 10–12 seconds.
Pregnancy Considerations
Desire for future fertility is considered a contraindication to myolysis. Although successful pregnancies have been reported after myolysis, two cases of uterine rupture in pregnant patients has also been reported.37, 38 Uterine rupture occurred at 32 and 39 weeks' gestation. respectively, with death occurring in the 32-week-old fetus.
Crymyolysis
Cryomyolysis is a procedure similar to myolysis. Various types of cryoprobes have been adapted and used for cryomyolysis. The size of the ice ball is monitored throughout the freezing with the use of ultrasound. At the current time, minimal data are available on the procedure and it should still be considered investigational.39, 40, 41
Laparoscopic Bipolar Coagulation of Uterine Vessels
The use of laparoscopy to coagulate the uterine vessels and produce fibroid necrosis has been reported in 85 women.42 Symptomatic improvement was reported in 89.4%. Mean uterine volume decreased to a mean of 46%. Two pregnancies occurred at 4 and 9 months. Both women had elective termination of these pregnancies. Three women became menopausal after the therapy, but it was uncertain if this was a consequence of the therapy. Because long-term follow-up is not available, it remains uncertain what the long-term effects of this therapy will be.
CONCLUSION
An increasing number of newer minimally invasive modalities are being developed for the treatment of uterine fibroids. Some, like uterine artery embolization, are a new use of an older technology, others are completely new developments. Whether these methods will ultimately prove to be superior to and replace older traditional methods of managing fibroid will only be proven with time.
REFERENCES
Cramer SF, Patel A: The frequency of uterine leiomyomas. Am J Clin Pathol 94:435-438, 1990 |
|
Greenberg MD, Kazamel TI: Medical and socioeconomic impact of uterine fibroids. Obstet Gynecol Clin North Am 22:625-636, 1995 |
|
Kjerulff KH, Guzinski GM, Langenberg PW et al: Hysterectomy and race. Obstet Gynecol 82:757-764, 1993 |
|
Townsend DE, Sparkes RS, Baluda MC et al: Unicellular histogenesis of uterine leiomyomas as determined by electrophoresis by glucose-6-phosphate dehydrogenase. Am J Obstet Gynecol 107:1168-1173, 1970 |
|
Huang SC, Yu CH, Huang RT et al: Intratumoral blood flow in uterine myoma correlated with a lower tumor size and volume, but not correlated with cell proliferation or angiogenesis. Obstet Gynecol 87:1019-1024, 1996 |
|
Broekmans FJ, Hompes PG, Heitbrink MA et al: Two-step gonadotropin-releasing hormone agonist treatment of uterine leiomyomas: standard-dose therapy followed by reduced-dose therapy. Am J Obstet Gynecol 175:1208-1216, 1996 |
|
Costantini S, Anserini P, Valenzano M et al: Luteinizing hormone-releasing hormone analog therapy of uterine fibroid: analysis of results obtained with buserelin administered intranasally and goserelin administered subcutaneously as a monthly depot. Eur J Obstet Gynecol Reprod Biol 37:63-69, 1990 |
|
Palomba S, Affinito P, Di Carlo C et al: Long-term administration of tibolone plus gonadotropin-releasing hormone agonist for the treatment of uterine leiomyomas: effectiveness and effects on vasomotor symptoms, bone mass, and lipid profiles. Fertil Steril 72:889-895, 1999 |
|
Hackenberg R, Gesenhues T, Deichert U et al: The response of uterine fibroids to GnRH-agonist treatment can be predicted in most cases after one month. Eur J Obstet Gynecol Reprod Biol 45:125-129, 1992 |
|
de Aloysio D, Altieri P, Pretolani G et al: The combined effect of a GnRH analog in premenopause plus postmenopausal estrogen deficiency for the treatment of uterine leiomyomas in perimenopausal women. Gynecol Obstet Invest 39:115-119, 1995. |
|
Donnez J, Schrurs B, Gillerot S et al: Treatment of uterine fibroids with implants of gonadotropin-releasing hormone agonist: assessment by hysterography. Fertil Steril 51:947-950, 1989 |
|
Serra GB, Panetta V, Colosimo M et al: Efficacy of leuprorelin acetate depot in symptomatic fibromatous uteri: The Italian Multicentre Trial. Clin Ther 14:57-73, 1992 |
|
van Leusden HA: Symptom-free interval after triptorelin treatment of uterine fibroids: long-term results. Gynecol Endocrinol 6:189-198, 1992 |
|
Murphy AA, Morales AJ, Kettel LM et al: Regression of uterine leiomyomata to the antiprogesterone RU486: dose-response effect. Fertil Steril 64:187-190, 1995 |
|
Ravina JH, Herbreteau D, Ciraru-Vigneron N et al: Arterial embolisation to treat uterine myomata. Lancet 346:671-672, 1995 |
|
Hurst BS, Stackhouse DJ, Matthews ML et al: Uterine artery embolization for symptomatic uterine myomas. Fertil Steril 74:855-869, 2000 |
|
Ravina JH, Bouret JM, Ciraru-Vigneron N et al: [Recourse to particular arterial embolization in the treatment of some uterine leiomyoma]. Bull Acad Natl Med 181:233-246, 1997 |
|
Sniderman KW, Sos TA, Alonso DR: Transcatheter embolization with Gelfoam and Avitene: the effect of Sotradecol on the duration of arterial occlusion. Invest Radiol 16:501-507, 1981 |
|
Walker WJ: Bilateral uterine artery embolisation of fibroids. In: Hutton C, Seth SS, (eds): Menorrhagia. Oxford, ISIS Medical Media, 1999 |
|
Burbank F, Hutchins FL Jr: Uterine artery occlusion by embolization or surgery for the treatment of fibroids: a unifying hypothesis - transient uterine ischemia. J Am Assoc Gynecol Laparosc 7:S1-49, 2000 |
|
Bradley EA, Reidy JF, Forman RG et al: Transcatheter uterine artery embolisation to treat large uterine fibroids. Br J Obstet Gynaecol 105:235-240, 1998 |
|
Payne JF, Haney AF: Serious complications of uterine artery embolization for conservative treatment of fibroids. Fertil Steril 79:128-131, 2003 |
|
Pron G, Bennett J, Common A et al: The Ontario Uterine Fibroid Embolization Trial. Part 2. Uterine fibroid reduction and symptom relief after uterine artery embolization for fibroids Fertil Steril 79:120-127, 2003. |
|
Goodwin SC, Spies JB, Worthington-Kirsch R et al: Uterine artery embolization for treatment of leiomyomata: long-term outcomes fromthe FIBROID Registry. Obstet Gynecol 2008;111(1):22-33. |
|
Spies JB, Scialli AR, Jha RC et al: Initial results from uterine fibroid embolization for symptomatic leiomyomata. J Vasc Interv Radiol 10:1149-1157, 1999 |
|
Hata K, Hata T, Maruyama R et al: Uterine sarcoma: can it be differentiated from uterine leiomyoma with Doppler ultrasonography? A preliminary report Ultrasound Obstet Gynecol 9:101-104, 1997 |
|
McLucas B, Adler L, Perrella R: Predictive factors for success in uterine fibroid embolization. Boston, SMIT/CIMIT 11th Annual Scientific Meeting, 1999 |
|
Goodwin SC, Walker WJ: Uterine artery embolization for the treatment of uterine fibroids. Curr Opin Obstet Gynecol 10:315-320, 1998 |
|
Siskin GP, Tublin ME, Stainken BF et al: Bilateral uterine artery embolization for the treatment of menorrhagia due to adenomyosis SCVIR Annual Meeting, 2000 |
|
Ravina JH, Vigeron NO, Aymard A et al: Pregnancy after embolization of uterine myoma: Report 12 cases. Fertil Steril 73:1241-1243, 2000 |
|
Forman RG, Reidy J, Nott V et al: Fibroids and fertility. Boston, SMIT/CIMIT 11th Annual Scientific Meeting, 1999 |
|
Vaezy S, Fujimoto VY, Walker C et al: Treatment of uterine fibroid tumors in a nude mouse model using high-intensity focused ultrasound. Am J Obstet Gynecol 183:6-11, 2000 |
|
Hindley J, Gedroyc WM, Regan L et al: MRI guidance of focused ultrasound therapy of uterine fibroids: early results. AJR Am J Roentgenol 2004;183(6):1713-19 |
|
Stewart EA, Rabinovici J, Tempany CM et al: Clinical outcomes of focused ultrasound surgery for the treatment of uterine fibroids. Fertil Steril 2006;85(1):22-9 |
|
Goldfarb HA: Laparoscopic coagulation of myoma (myolysis). Obstet Gynecol Clin North Am 22:807-819, 1995 |
|
Goldfarb HA: Nd:YAG laser laparoscopic coagulation of symptomatic myomas. J Reprod Med 37:636-638, 1992 |
|
Vilos GA, Daly LJ, Tse BM: Pregnancy outcome after laparoscopic electromyolysis. J Am Assoc Gynecol Laparosc 5:289-292, 1998 |
|
Phillips DR, Milim SJ, Nathanson HG et al: Experience with laparoscopic leiomyoma coagulation and concomitant operative hysteroscopy. J Am Assoc Gynecol Laparosc 4:425-433, 1997 |
|
Zreik TG, Rutherford TJ, Palter SF et al: Cryomyolysis, a new procedure for the conservative treatment of uterine fibroids. J Am Assoc Gynecol Laparosc 5:33-38, 1998 |
|
Olive DL, Rutherford T, Zreik T et al: Cryomyolysis in the Conservative Treatment of Uterine Fibroids. J Am Assoc Gynecol Laparosc 3:S36, 1996 |
|
Odnusi KO, Rutherford TJ, Olive DL et al: Cryomyolysis in the Management of Uterine Fibroids: Technique and Complications. Surg Technol Int VIII:173-178, 2000 |
|
Liu WM, Ng HT, Wu YC et al: Laparoscopic bipolar coagulation of uterine vessels: a new method for treating symptomatic fibroids. Fertil Steril 75:417-422, 2001 |