This chapter should be cited as follows:
Devlieger R, Miserez L, et al., Glob Libr Women's Med
ISSN: 1756-2228; DOI 10.3843/GLOWM.421683
Nutrition in the Periconceptional, Pregnancy and Postpartum Periods
Volume Editor:
DOI 10.3843/GLOWM.00000
Chapter
Counseling and prevention in women living with obesity
VIDEO 13
Obesity is a chronic, relapsing, progressive disease associated with severe complications and comorbidities. Adequate preconception counseling is important for women who are overweight or obese and are planning to become pregnant. Excess weight in the preconception period can influence fecundability (average per-cycle probability of conception), as well as the trajectory of metabolic changes during pregnancy and in the postpartum period due to inflammation, dyslipidemia and insulin resistance.
INTRODUCTION
Maternal obesity is a growing public health concern that poses significant risks to both mothers and their offspring. The prevalence of obesity among women of reproductive age has increased dramatically over the past decades, largely due to sedentary lifestyle, unhealthy dietary habits and genetic predisposition. Understanding the consequences of maternal obesity and identifying strategies to prevent excessive gestational weight gain is critical for improving maternal and neonatal health outcomes.
MATERNAL OBESITY
Obesity is defined as a body mass index (BMI) of 30 kg/m2 or higher. In the context of pregnancy, maternal obesity is associated with numerous complications. These include an increased risk of gestational diabetes mellitus (GDM), hypertensive disorders, pre-eclampsia and Cesarean delivery. Additionally, maternal obesity has long-term implications, such as postpartum weight retention, cardiovascular disease and a predisposition to obesity in subsequent pregnancies1,2.
The prevalence of maternal obesity varies globally, with higher rates observed in developed countries. Social determinants such as socioeconomic status, education level and access to healthcare significantly influence these rates. The rising prevalence of maternal obesity reflects broader societal trends in obesity and highlights the need for targeted interventions1,2.
INFLUENCE OF MATERNAL BMI ON REPRODUCTION AND PREGNANCY
Maternal BMI has a profound impact on reproductive health and pregnancy outcomes. Elevated BMI levels can impair fertility, increase the likelihood of pregnancy complications and negatively affect fetal development2.
Effects on fertility2
Obesity is associated with hormonal imbalances, which can lead to ovulatory dysfunction and infertility. Polycystic ovary syndrome (PCOS), a common condition linked to obesity, exacerbates these issues. Additionally, obesity reduces the success rates of assisted reproductive technologies (ART), such as in vitro fertilization (IVF), due to poor oocyte quality and endometrial receptivity.
Pregnancy complications2
During pregnancy, maternal obesity is a risk factor for various complications:
- Gestational diabetes mellitus (GDM): Obese women are more prone to insulin resistance, which increases the risk of developing GDM. GDM can result in macrosomia (large-for-gestational-age infants), birth trauma and neonatal hypoglycemia.
- Hypertensive disorders: Obese pregnant women have a higher risk of developing chronic hypertension and pre-eclampsia. These conditions can lead to preterm delivery, placental abruption and maternal morbidity.
- Delivery complications: Obesity increases the likelihood of prolonged labor, failed labor induction and Cesarean delivery. Surgical complications, such as wound infections and thromboembolism, are also more common in obese women.
Impact on fetal and neonatal health2
Maternal obesity adversely affects fetal development and long-term health. Some key concerns include:
- Congenital anomalies: Obesity increases the risk of neural tube defects and other congenital anomalies.
- Macrosomia: Excessive fetal growth can lead to birth injuries and necessitate Cesarean delivery.
- Long-term effects: Offspring of obese mothers are more likely to develop childhood obesity, metabolic syndrome, and type-2 diabetes, perpetuating the cycle of obesity.
HOW TO PREVENT MATERNAL OBESITY AND EXCESSIVE GESTATIONAL WEIGHT GAIN
Preventing maternal obesity and excessive gestational weight gain requires a multifaceted approach, including lifestyle modifications, healthcare interventions and community support.
Preconception care3,4
Addressing obesity before pregnancy is essential. Preconception counseling can help women understand the risks associated with maternal obesity and motivate them to adopt healthier behaviors. Key components of preconception care include.
- Nutritional counseling: Encouraging a balanced diet rich in fruits, vegetables, whole grains and lean proteins.
- Physical activity: Promoting regular exercise tailored to individual fitness levels.
- Weight management: Setting realistic weight-loss goals before conception.
- Medication: Medication including GLP-1 agonists are increasingly being used to obtain a healthy BMI prior to pregnancy. As safety during pregnancy is unclear, these medications should be stopped before conception5.
- Metabolic and bariatric surgery (MBS): In case of severe obesity of grade II and higher, surgical management of obesity will effectively reduce adiposity and improve some reproductive outcomes. However, pregnancy after MBS should be considered high risk and requires specialized follow-up in order to avoid complications like prematurity and growth restriction in the fetus6.
Healthy weight gain during pregnancy
Guidelines from organizations like the Institute of Medicine (IOM)7 provide recommendations for appropriate weight gain during pregnancy based on prepregnancy BMI. These guidelines emphasize the importance of monitoring weight gain and adjusting dietary and physical activity levels as needed.
Lifestyle modifications2
- Dietary interventions:
- Adopt a nutrient-dense diet that meets the caloric needs of pregnancy without exceeding them.
- Avoid processed foods high in sugar and saturated fats.
- Physical activity:
- Engage in moderate-intensity activities, such as walking, swimming or prenatal yoga, for at least 150 minutes per week.
- Consult with healthcare providers to ensure exercise routines are safe and appropriate.
- Behavioral support:
- Seek support from dietitians, counselors and support groups to maintain motivation and adherence to healthy habits.
Healthcare interventions2
- Regular monitoring: Frequent prenatal visits to track weight gain and identify potential complications early.
- Screening and management: Early screening for GDM and hypertension in obese women to minimize risks.
- Pharmacological interventions: In some cases, medication may be prescribed to manage obesity-related complications, though these should be used cautiously during pregnancy.
Community and policy-level initiatives2
- Promote public health campaigns that raise awareness about maternal obesity and healthy lifestyles.
- Improve access to affordable, nutritious food and safe spaces for physical activity.
- Encourage workplace policies that support maternal health, such as maternity leave and lactation accommodations.
1
Recommended weight gain during pregnancy7.
Pre-pregnancy BMI | BMI Category | Recommended total weight gain | Rate of weight gain |
<18.5 | Underweight | 12.5–18.0 | 0.44–0.58 kg/week |
18.5–24.9 | Normal Weight | 11.5–16.0 | 0.35–0.50 kg/week |
25.0–29.9 | Overweight | 7.0–11.5 | 0.23–0.33 kg/week |
≥ 30.0 | Obese | 5.0–9.0 | 0.17–0.27 kg/week |
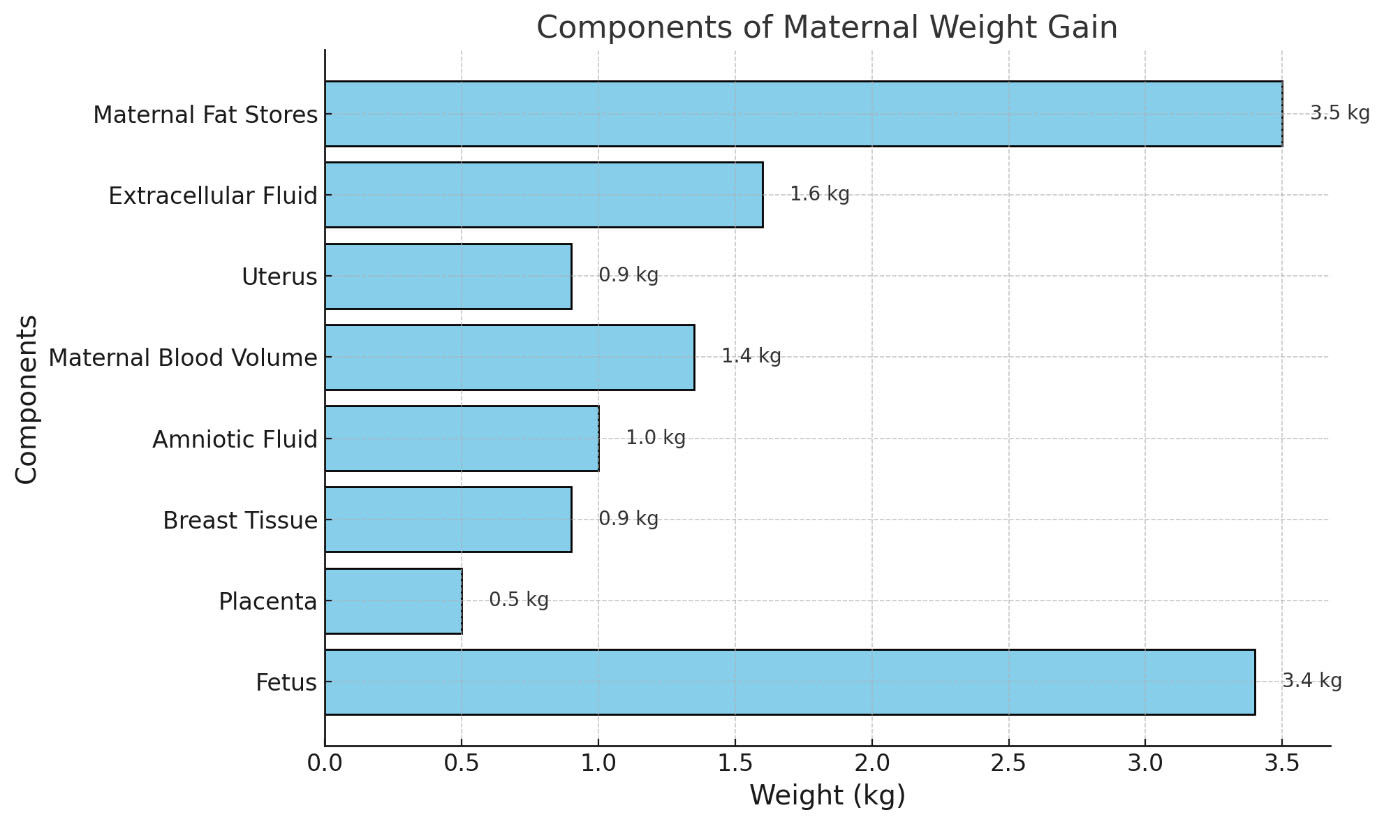
Below is an illustrative breakdown of the typical components contributing to maternal weight gain during pregnancy:
1
Components of maternal weight gain8. (Note: Values are approximate and may vary between individuals.)
CONCLUSION
Maternal obesity is a complex issue with far-reaching implications for maternal and child health. By addressing obesity before conception, promoting healthy lifestyles during pregnancy and implementing supportive healthcare interventions, it is possible to mitigate the risks associated with maternal obesity and excessive gestational weight gain. Collaborative efforts at the individual, healthcare and community levels are essential for creating healthier generations and breaking the cycle of obesity.
CONFLICTS OF INTEREST
Author(s) statement awaited.
REFERENCES
Chooi YC, Ding C, Magkos F. The epidemiology of obesity. Metabolism [Internet]. 22 september 2018;92:6–10. Available from: https://doi.org/10.1016/j.metabol.2018.09.005 | |
Creanga AA, Catalano PM, Bateman BT. Obesity in Pregnancy. N Engl J Med. 2022 Jul 21;387(3):248–259. doi: 10.1056/NEJMra1801040. PMID: 35857661. Available from: https://doi.org/10.1056/nejmra1801040 | |
Stephenson J, Heslehurst N, Hall J, Schoenaker DAJM, Hutchinson J, Cade JE, Poston L, Barrett G, Crozier SR, Barker M, Kumaran K, Yajnik CS, Baird J, Mishra GD. Before the beginning: nutrition and lifestyle in the preconception period and its importance for future health. Lancet. 2018 May 5;391(10132):1830–1841. doi: 10.1016/S0140–6736(18)30311–8. Available from: https://doi.org/10.1016/s0140-6736(18)3031-8 | |
Fleming TP, Watkins AJ, Velazquez MA, Mathers JC, Prentice AM, Stephenson J, Barker M, Saffery R, Yajnik CS, Eckert JJ, Hanson MA, Forrester T, Gluckman PD, Godfrey KM. Origins of lifetime health around the time of conception: causes and consequences. Lancet. 2018 May 5;391(10132):1842–1852. doi: 10.1016/S0140-6736(18)30312-X. Available from: https://doi.org/10.1016/s0140-6736(18)30312-x | |
Drummond RF, Seif KE, Reece EA. Glucagon-like peptide-1 receptor agonist use in pregnancy: a review. Am J Obstet Gynecol. 2025 Jan;232(1):17–25. doi: 10.1016/j.ajog.2024.08.024. Epub 2024 Aug 23. PMID: 39181497. | |
Ceulemans D, Deleus E, Benhalima K, van der Schueren B, Lannoo M, Devlieger R. Pregnancy After Metabolic Bariatric Surgery: Risks and Rewards for Mother and Child. 2024 Dec 11. doi: 10.1111/1471-0528.18032. Epub ahead of print. PMID: 39663779. | |
Weight gain during pregnancy [Internet]. Available from: https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2013/01/weight-gain-during-pregnancy#:~:text=Given%20the%20limited%20data%20by,births%20and%20postpartum%20weight%20retention | |
Rasmussen KM, Yaktine AL. Composition and components of Gestational Weight gain: Physiology and metabolism [Internet]. Weight Gain During Pregnancy – NCBI Bookshelf. 2009. Available from: https://www.ncbi.nlm.nih.gov/books/NBK32815/ |
Online Study Assessment Option
All readers who are qualified doctors or allied medical professionals can automatically receive 1.5 Continuing Professional Development points plus a Study Completion Certificate from GLOWM for successfully answering four multiple-choice questions (randomly selected) based on the study of this chapter. Medical students can receive the Study Completion Certificate only.
(To find out more about the Continuing Professional Development awards program CLICK HERE)
