
Painful periods and heavy menstrual bleeding
An educational
initiative
supported by

Written by experienced doctors, midwives and other medical professionals – and approved by a specialist Editorial Board
Enhancing the Welfare of Women
Expert Health Information for Women












The authors of this PAINFUL PERIODS AND HEAVY MENSTRUAL BLEEDING program are:
- Dr Winnie Mwebia
Obstetrician Gynecologist/Assistant Principal Clinical Research Scientist, KEMRI Centre for Global Health Research, Kenya - Dr Dorcus Muchiri
Consultant Obstetrician Gynaecologist/Reproductive Medicine Specialist/Women's Health Researcher and Educator, The George Institute for Global Health, Imperial College London NHS Hospitals Trust, London, UK; and Bonita Centre for Women's Health, Nairobi, Kenya
The Welfare of Women program has been created under the General Editorship of Dr Kate Lightly, University of Liverpool, UK and is overseen by an expert International Editorial Board
The cost of producing this resource has been partly funded by an educational grant from GSK
Thank you for watching this Welfare of Women video. We would welcome your views and feedback. Please complete this short questionnaire.
Painful periods and heavy menstrual bleeding
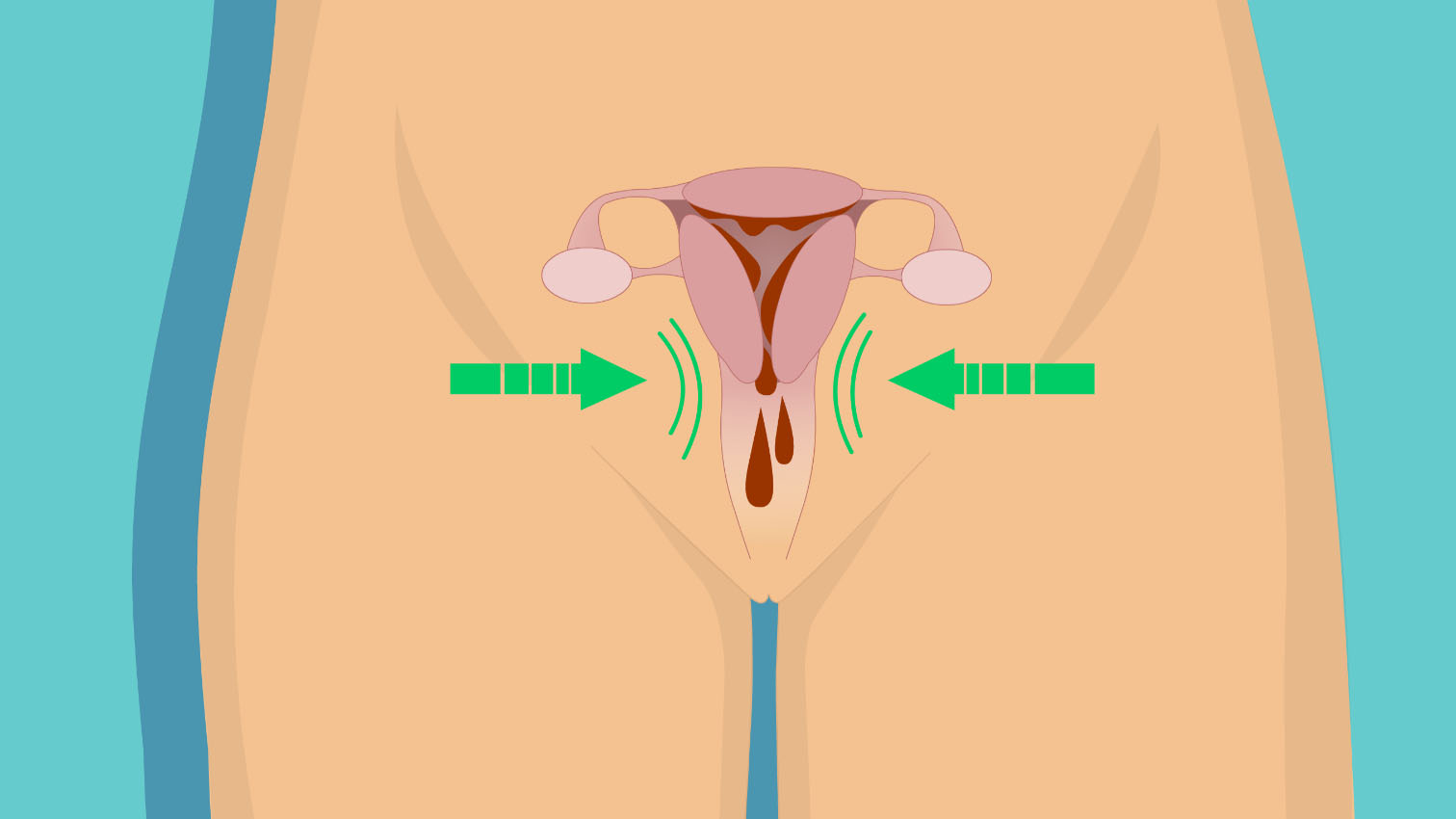
Painful periods (also known as dysmenorrhea), is the painful cramping felt in the lower abdomen (tummy), lower back and/or inner thighs during periods (menses).
Period pains are grouped into two groups; normal period pains and pain due to an underlying pelvic problem such as endometriosis or fibroids.
What is normal bleeding?
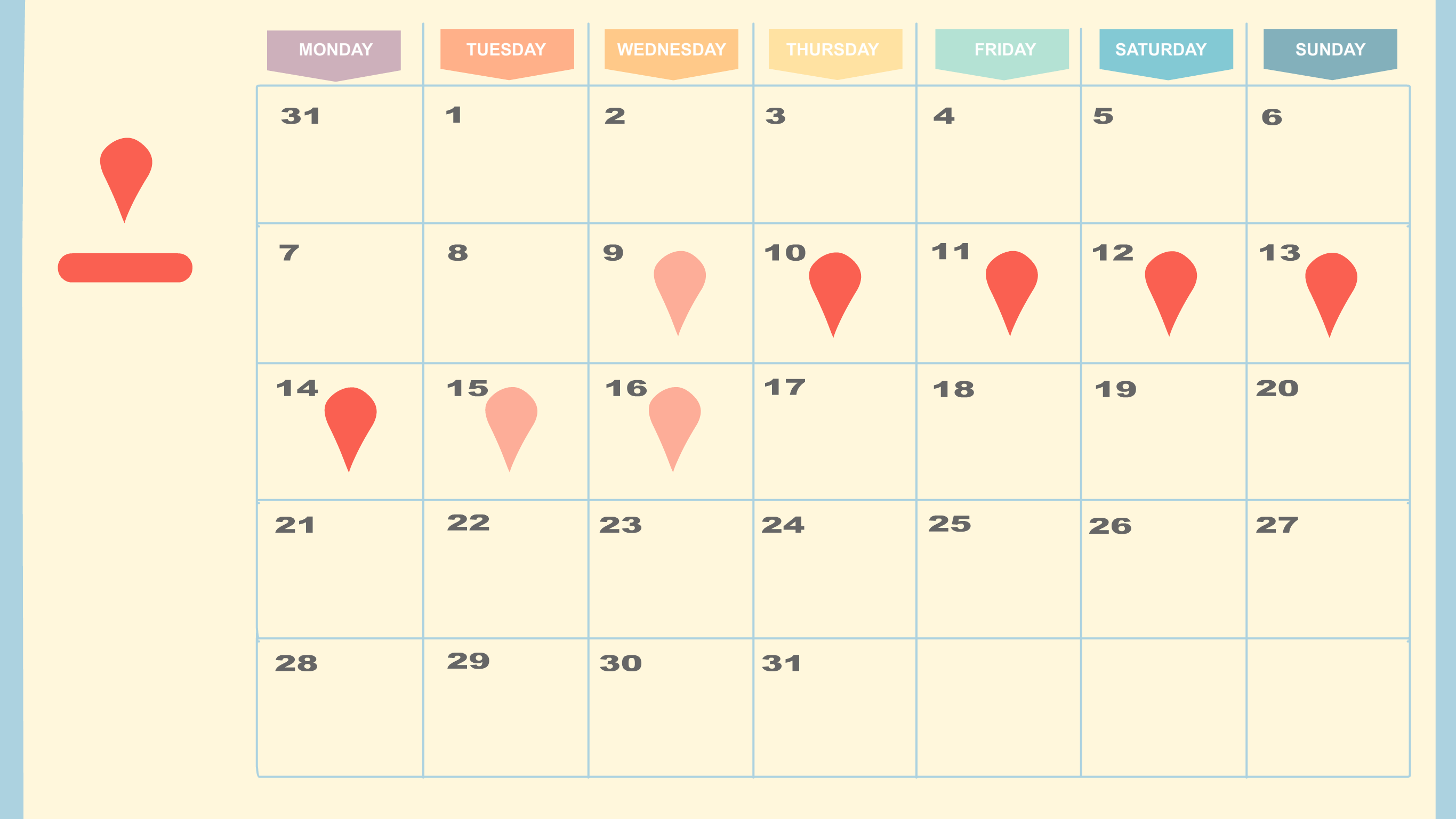
Normal periods usually last less than 8 days.
They come roughly every month, and can be between 24 and 38 days.
The pain sets in within the first few months of periods starting.
The pain is usually mild and does not stop with normal daily functioning.
It is not associated with underlying health problems, and gets better with time and after childbirth in many women.
Other symptoms which may come with periods include mood changes, nausea, vomiting, tiredness and diarrhea.
What is considered abnormal bleeding?
Heavy menstrual bleeding (enough to affect your quality of life)
Irregular gaps between periods
Long periods (more than 8 days)
Bleeding in between periods
Bleeding after sex
Infrequent periods or no periods
What are the other symptoms to look out for?
Pain or heaviness of the lower abdomen outside the time of having a period
Painful sexual intercourse
Pain passing urine or opening bowels
Severe pain which interferes with normal functioning
Difficulty getting pregnant
Repeated pregnancy losses
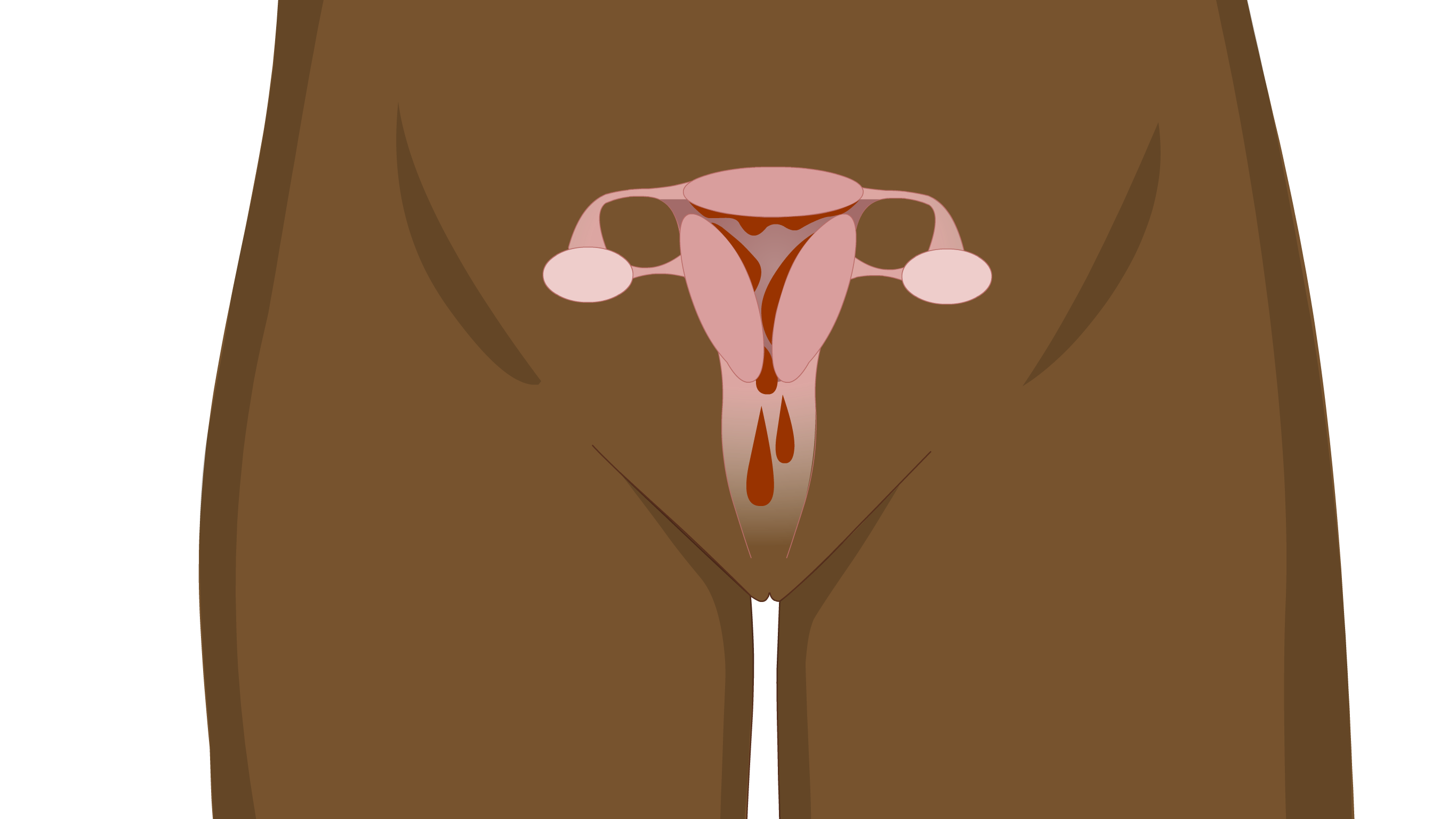
What causes the pain in periods?
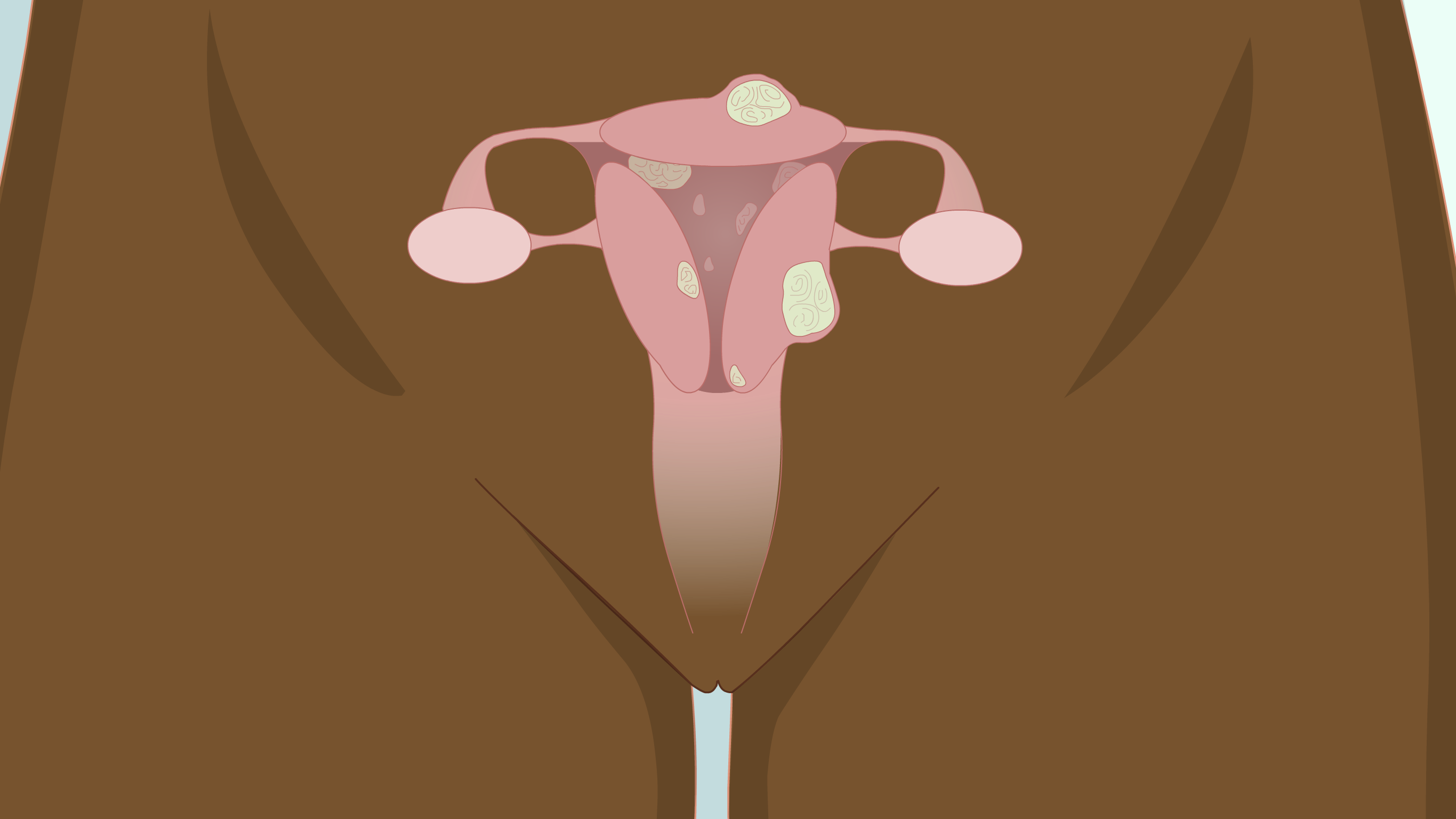
The body produces chemicals called prostaglandins during the time of the period. These make the uterus contract and tighten. Abnormal pain is often because of other conditions like fibroids, adenomyosis (abnormal placement of uterine muscle cells), endometriosis (where the uterine cells are outside the uterus), infection, or blockage of the cervix, vagina or genital opening.
When should you seek help?
If the pain or bleeding makes you take lots of medications.
If the pain or bleeding makes you not go to school or work.
If the pain or bleeding is getting worse month by month.
If the pain or bleeding occurs at times when you are not expecting your period.
If the pain or bleeding lasts longer than 8 days.
What will a healthcare provider do when they see you?
They will ask you some questions to understand the problem.
They may check your blood pressure and pulse rate.
Examinations can vary and are not always needed. Your healthcare worker may examine your tummy and may sometimes recommend an internal examination. They can check the neck of the womb (cervix) with a device called a speculum, or feel the womb with an internal examination through the vagina. The examination should not be painful and you must always give consent before you have it.
They may organize scans, blood tests, urine tests or swabs to help with the diagnosis.
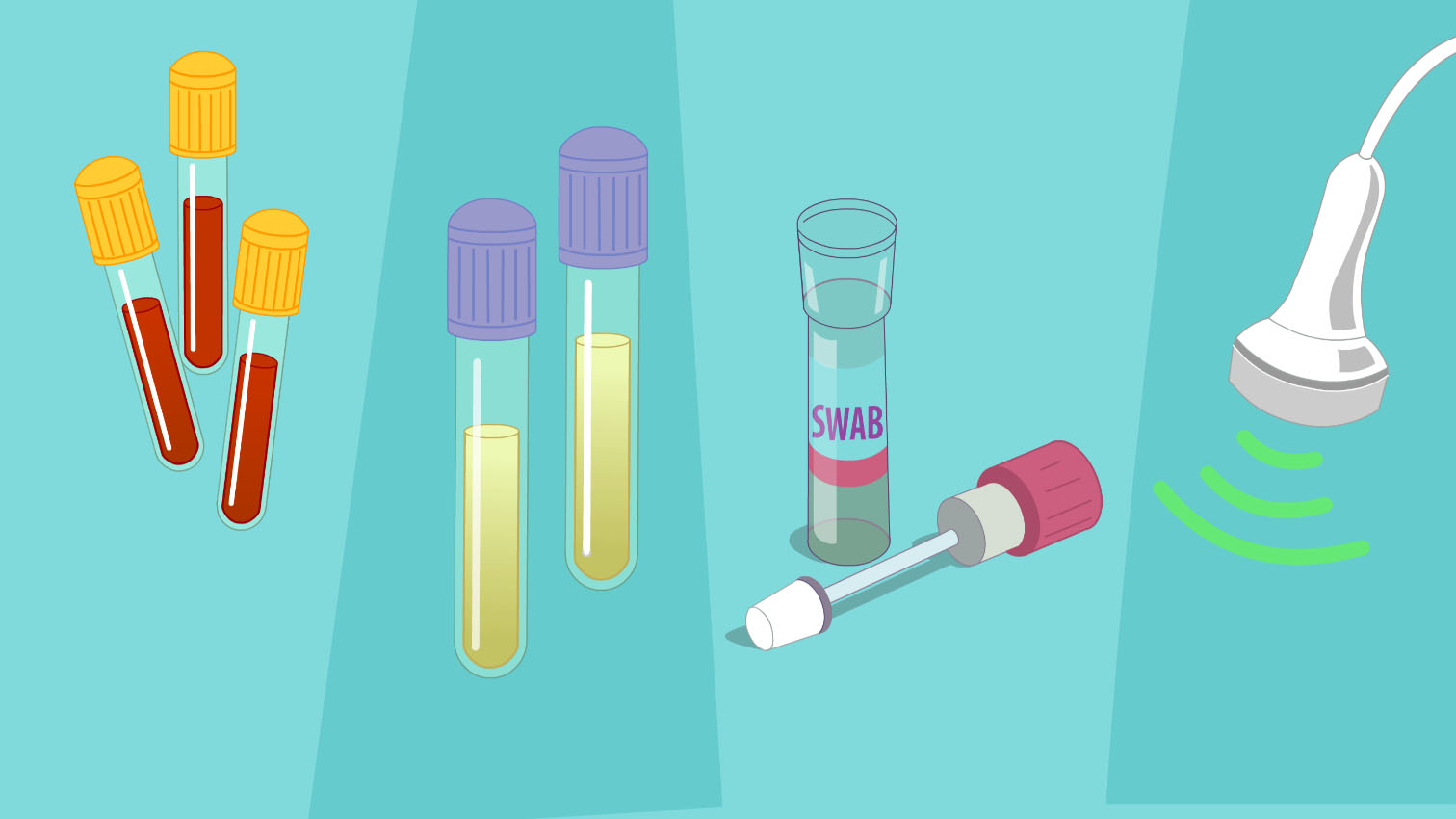
Depending on what they find, they may very occasionally ask for more complex imaging tests like CT or MRI.
How is period pain treated?
For mild period pain, some simple measures may help relieve symptoms:
use of warm compresses such as a heating pad or hot water bottle on the lower abdomen and lower back, and massage of the lower back;
having a healthy lifestyle, with regular exercise, no smoking, reduced caffeine and animal-fat intake and good rest.
How is more severe pain treated?
Medication for period pain ranges from simple pain medication such as brufen, hyoscine (buscopan) and paracetamol to other pain relievers such as diclofenac, mefenamic acid, ketoprofen and naproxen, which can be used for moderate-to-severe pain in some cases.
Different forms of contraception such as the hormonal contraceptive pill, implant, injectectable contraceptive and hormone intrauterine devices, such as Mirena, are often used to reduce pain and bleeding. Contraceptives which contain hormones can make your periods lighter or less frequent. These treatments are very safe for most women but take a few months to work.
Antibiotics may be required if the cause of pain is found to be an infection.

Different drugs can be used in combination, as deemed necessary.
When might surgery be needed?
For some women, surgery may be necessary for growths of the uterus such as fibroids, polyps or adenomyosis, endometriosis or blockage of any part of the genital tract.
The type of surgery depends on what the problem is, and can involve open surgery (cut to the tummy), laparoscopy (keyhole surgery) or hysteroscopy (camera into the womb).
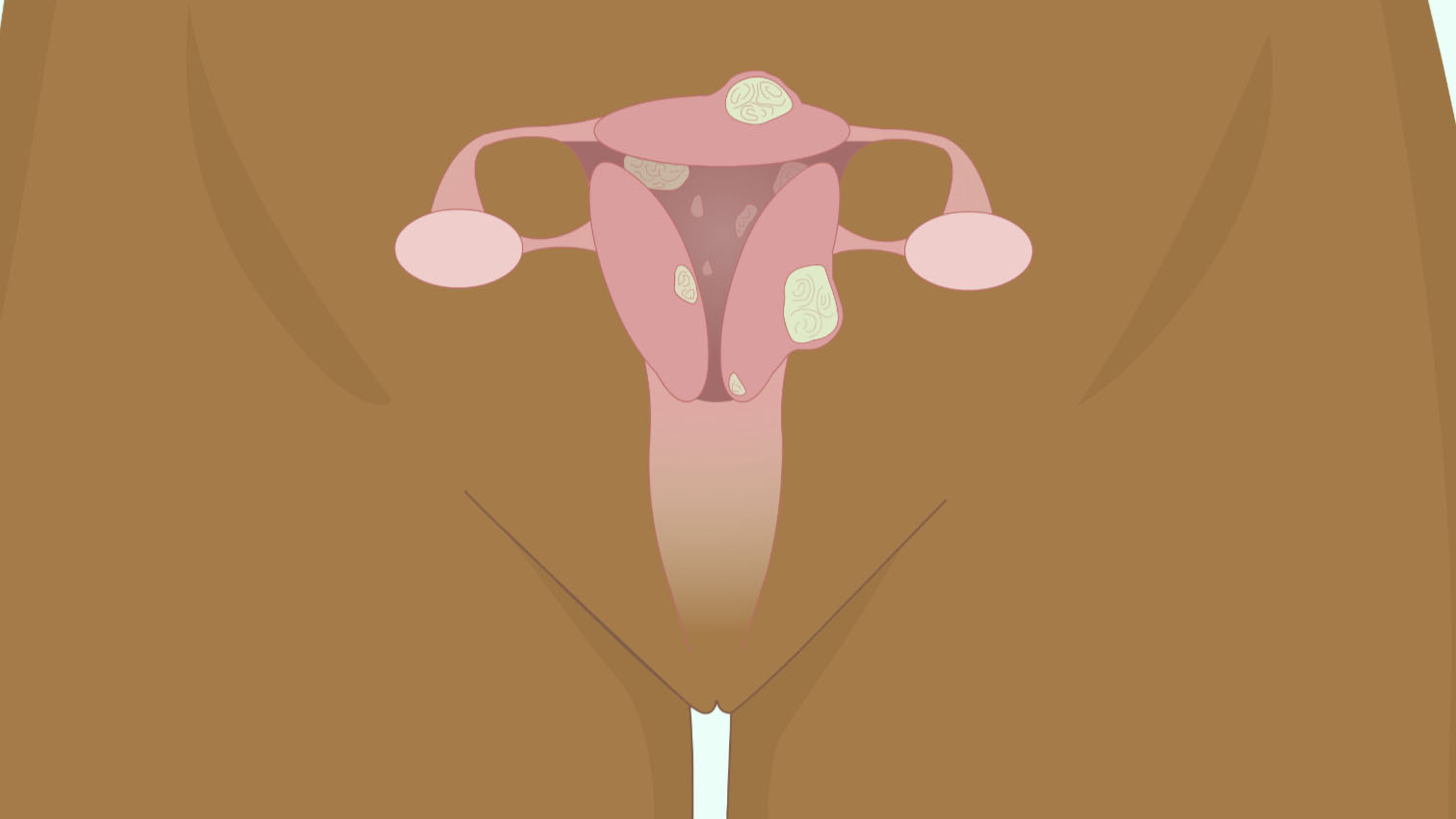
Surgery can be as simple as removal of small endometriotic tissues, removal of fibroid or adenomyoma or the complete removal of uterus and ovaries (hysterectomy). This is usually a last resort, and is more likely in older women who have completed their family.
What else should I know?
Normal period pain tends to reduce after childbirth. Also, pain from endometriosis or adenomyosis may reduce after childbirth.
Normal period pain does not affect fertility. However, if the pain is due to other underlying problems fertility may be affected. Be aware that the non-steroidal anti-inflammatory medications such as brufen, ketoprofen and diclofenac may affect fertility during the cycle when they are taken. It is therefore important to discuss fertility concerns with your medical provider if you have any concerning symptoms.
In rare cases in which there is a blockage of the cervix, vagina or the vaginal opening, pelvic pain can be experienced around the time when your period is due, without any bleeding. If you experience this, please visit your medical provider to check this out.
Painful and heavy periods are very common and can be normal or abnormal. If your periods are affecting your quality of life, see your healthcare worker to get advice.
The authors of this PAINFUL PERIODS AND HEAVY MENSTRUAL BLEEDING program are:
- Dr Winnie Mwebia, Obstetrician Gynecologist/Assistant Principal Clinical Research Scientist, KEMRI Centre for Global Health Research, Kenya
- Dr Dorcus Muchiri, Consultant Obstetrician Gynaecologist/Reproductive Medicine Specialist/Women's Health Researcher and Educator, The George Institute for Global Health, Imperial College London NHS Hospitals Trust, London, UK; and Bonita Centre for Women's Health, Nairobi, Kenya
The Welfare of Women program has been created under the General Editorship of Dr Kate Lightly, University of Liverpool, UK and is overseen by an expert International Editorial Board
The publishing reference for this program is: DOI 10.3843/GLOWM.w10068
The Welfare of Women information program is an attempt to provide women everywhere with access to reliable information about key health issues that may be relevant to them. Information is offered at three separate levels which women may select according to their preferences; firstly, short video animations with voice commentary, secondly, more detailed text-based descriptions, and thirdly, links to recommended further reading. With the animated videos, women can also select the images that they feel most comfortable in viewing from a short range of very generalized and non-specific ethnicity options. Because of the special programming used, both the videos and the text information can – when authorized – be translated into any language in a simple and rapid manner.
Recommended links for more comprehensive and detailed reading
The following websites provide more comprehensive and extensive information on this topic, which is both reliable and strongly recommended for readers who want to learn more than the details provided above:
Heavy periods
https://www.nhs.uk/conditions/heavy-periods/
Heavy Menstrual bleeding
https://www.cdc.gov/female-blood-disorders/about/heavy-menstrual-bleeding.html
Resources the author(s) used in preparing this guidance
Medscape
https://emedicine.medscape.com/article/253812-overview
CDC
https://www.cdc.gov/ncbddd/blooddisorders/women/menorrhagia.htm
NHS/RCOG
https://www.nhs.uk/conditions/heavy-periods/
ACOG
https://www.acog.org/womens-health/faqs/dysmenorrhea-painful-periods
https://www.acog.org/clinical/clinical-guidance/committee-opinion/articles/2018/12/dysmenorrhea-and-endometriosis-in-the-adolescent
Cleveland Clinic
https://my.clevelandclinic.org/health/diseases/4148-dysmenorrhea
The Royal Pharmaceutical Society
https://pharmaceutical-journal.com/article/ld/case-based-learning-dysmenorrhoea-management

