Chapter 8
Theater Ergonomics
(see Video 5: Theater ergonomics)
Video 5 Theater ergonomics
Figure 7 is a schematic representation of an operating theater designed to maximize functionality. It is axiomatic that not all operating theaters will conform to this diagram. However, the main point is to ensure patient safety. If the surgeon is of the opinion that laparoscopy cannot be safely performed in an old facility with an inadequate electrical supply, then surgery should not be initiated. This figure only applies to the operating room set up (Video 5: Theater ergonomics).
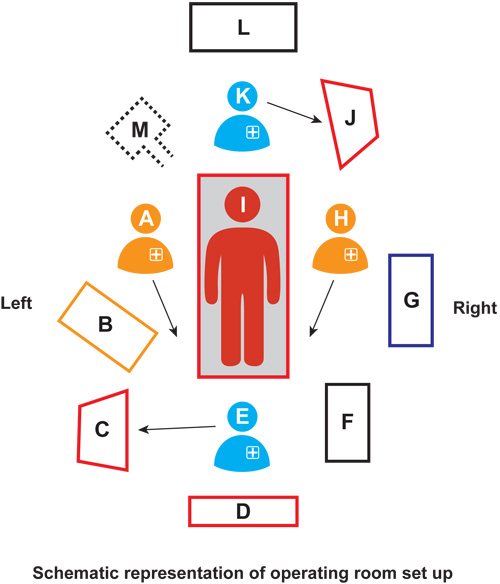
Figure 7 Schematic diagram of operation room set up: A, main surgeon; B, laparoscopy instrument trolley; C, monitor for vaginal assistant; D, main monitor for operating surgeon and assistant; E, vaginal assistant; F, vaginal instrument trolley; G, accessory instrument trolley; H, assistant surgeon; I, patient; J, anesthesia work station; K, anesthesiologist; L, emergency drug trolley; M, patient body warmer unit; arrows indicate direction of vision
For surgical ergonomics, the senior author prefers to stand on the right side of the patient for laparoscopic hysterectomy. Standing on the right side replicates the process the surgeon uses for the abdominal hysterectomy with the extension of his hands with laparoscopic instruments. Individuals who prefer to stand on the left side of the patient are left handed or have been trained in this manner. Ideally two assistants are required. The first stands opposite the surgeon and follows directions as given. The second sits between the patient’s legs and performs crucial functions related to uterine manipulation. This includes elevating the uterus out of the lower pelvis to bring it closer to the operating instruments as well as rotating the uterus so that the pedicles are brought from the lateral to the anterior position, thereby facilitating cauterization and division. Such motions also minimize blood loss and injury to lateral structures such as the ureter. If this plan is ignored, the surgeon will likely dig deeper and deeper to reach appropriate structures, lose heart, and open the patient to complete the operation which in all likelihood will never be attempted again.
It is preferable that the assistant sitting at the vaginal end be a scrub nurse rather than a physician who would prefer to look at the monitor rather than maintain the optimum uterine position. The main job of the vaginal assistant is to perform uterine manipulation with the help of the manipulator. This person’s job is crucial for the smooth running of the surgical procedure.
The major role of the assistant surgeon is to hold the camera in such a position so that the surgical site is centered on the monitor screen. The camera should not be so close to the tip of the electrosurgical equipment that the remainder of the field is not visible. Specifically, a part of the bowel should always be visualized in relation to the tip and the joint of the operating instrument (Video 6: Relation between tip of bipolar forceps, the activated joint and bowel). If this principle is followed, it is far less likely that an electrosurgical or mechanical bowel injury will occur.
Video 6 Relation between tip of bipolar forceps, the activated joint and bowel
The assistant surgeon should be well versed with the movement of the 30° telescope which has a ‘look down capacity’ and can reach to any part of the pelvis.
As noted above, the laparoscopic instrument trolley should remain close by the surgeon’s side so that he/she can pick up an individual instrument when needed rather than ask for it from a nurse. Importantly, the surgeon may keep a mental image of the desired instrument in mind and may choose it instantaneously, whereas the scrub nurse may not be familiar with the verbalized description of the instrument. In this construct, the surgeon himself takes the instruments from the instrument trolley which has been placed close by.
It is important to avoid clutter by preselection of only those instruments that are likely to be used in the operation. Figure 8 shows the senior author’s laparoscopy instrument trolley with a total of 10 instruments. These are sufficient to accomplish a straightforward hysterectomy from start to finish, unless the morcellator is needed. The instruments are laid out in the sequential order that they will be used. Floor clutter with cables and tubing can be avoided with careful planning and appropriate theater layout before the operation begins.

Figure 8 Main instrument trolley with a total of 10 instruments
A separate trolley is used for accessory instruments but otherwise required instruments including the fiber optic cable, the suction and irrigation tubing, cautery wire, and the sterile camera cover. If instead these were placed on the principle instrument trolley, they would add to clutter and confusion when the surgeon is looking for the required operative instrument (Figure 9).

Figure 9 Accessory instrument trolley
