Chapter 9
Instrumentation
Vaginal instrument trolley (Video 7: Vaginal instrument trolley)
Video 7 Vaginal instrument trolley
Video 7: Vaginal instrument trolley shows all that is required for the vaginal trolley. From the left, the reader will see the urinary bag, the syringe for the Foley inflation and the Foley catheter. The blue tube is the ‘vaginal delineator tube’ which is used to delineate the vaginal cuff when it is about to be opened. At this time, the uterine manipulator has been removed and the supporting structures of the uterus have been dealt with (uterine arteries, parametrium).
The next instrument is the uterine manipulator – Sankpal’s modified uterine manipulator. Next in order are the series of graduated dilators which are used to dilate the cervix up to size 9. As a number 9 is sufficient to insert the Sankpal manipulator, it is not necessary to clutter the table with the remaining larger dilators.
Two vulselli and two speculi are next. These instruments are useful when vaginal morcellation (Video 8: Uterine morcellation through the vaginal route) of a large uterus is required. The vulselli are used to grasp the anterior and posterior lips of the cervix at the same time for better traction on the bigger size uterus and aid retrieval of the specimen. The speculi are placed in the vagina to hold back the bladder and protect the rectum as the specimen is removed. Finally, the steel cup is used for antiseptic applied in the vaginal preparation.
Video 8 Uterine morcellation through the vaginal route
Uterine manipulator
The uterine manipulator is the key player in laparoscopic hysterectomy. It moves the uterus in any desired angle: up, down or to the sides. It also facilitates maintaining vital structures away from the operative field. Admittedly, it also is possible to manipulate the uterus from above with a myoma screw. However, the senior author prefers the uterine manipulator for a number of reasons unless the uterus is more than the 20 weeks size or is fixed in place owing to pathologies such as endometriosis and/or pelvic inflammatory disease.
- The myoma screw requires an additional port which is occupied throughout the entire surgery. The site of insertion into the uterus may require frequent change in order to bring the desired anatomic region into the operative field. Frequent changing of the screw location causes bleeding which disturbs the operative field and may prolong the operative time. Finally, using the myoma screw, rotation of uterus is limited as compared with vaginal manipulation (Video 9: Sankpal’s modified uterine manipulator and range of movements in total laparoscopic hysterectomy).
- The Sankpal manipulator has a length of 36 cm from the tip to the handle end. It is autoclavable and reusable. The manipulator tip is 8.5 cm which is angulated to 45° and faces the ceiling at the start of the operation. At the time of the bladder dissection, the position of the manipulator is reversed by closing the tips and rotating the manipulator position. Now the tips face the floor when the surgeon is ready to perform the bladder dissection and push it away from the anterior surface of the lower part of the uterus (Video 10: Rotating movement of the manipulator for bladder dissection). A guard in front of the joint separates the angle from the handle. The guard measures 4.5 cm in width. The distal tip is sufficiently long (8.5 cm) so that it can fit into a uterine cavity similar in size to a 14–16 weeks’ gestation. Such cavity sizes are common even if the uteruses are much larger, because the cavity does not normally enlarge as fibroids grow. A Sankpal manipulator is useful until the uterocervical length is more than 16–18 cm. The tips of the manipulator expand laterally to 5–6 cm which helps gripping the uterus to facilitate elevation and rotation movements.
- The manipulator guard lies tightly against the external cervical os. This tight fit helps push the entire uterus into the abdomen without perforation of the fundus by the tip of the manipulator. It also helps delineating the cervico-vaginal junction, which in turn identifies the extent of the bladder dissection off the vagina and facilitates effective skeletonization of the uterine vessels (Video 11: Manipulator guard facilitating bladder dissection and skeletonization of uterine vessels).
- The manipulator guard also makes the vaginal fornices prominent, thus protecting the bladder margins and ureters laterally. In addition, the upward push by the vaginal assistant on the manipulator protects the ureters by letting them fall laterally. At the same time the bladder is protected when the vaginal fornices are elevated (Video 12: Manipulator guard protecting the bladder margin and ureter).
- The handle of the manipulator is sufficiently long for better control of uterine manipulation (elevation, rotation and a combination of these two motions). In contrast, a smaller handle (available widely on other manipulators) would enter the vagina and disappear from view when the uterus is pushed cephalad, thus obstructing full rotational motion.
Video 9 Sankpal’s modified uterine manipulator and range of movements in total laparoscopic hysterectomy
Video 10 Rotating movement of manipulator for bladder dissection
Video 11 Manipulator guard facilitating bladder dissection and skeletonization of uterine vessels
Video 12 Manipulator guard protecting bladder margin and ureter
Vaginal delineator tube (Video 13: Vaginal delineator tube)
Video 13 Vaginal delineator tube
This device is made of polypropylene or ceramic with a diameter of 5.7 cm and a length of approximately 25 cm. The distal end is open and the proximal end has a cap which screws on. This cap has a hole which can be occluded with the thumb in order to assist in maintaining pneumoperitoneum when the vaginal cuff is opened. The tube is easily accommodated in the vagina unless the patient is postmenopausal with atrophy or has not given birth vaginally. Its presence within the vagina helps delineate the upper extent of the vagina at the moment the surgeon incises the upper vaginal cuff to remove the uterus. When the uterus has been removed, the proximal end of the vaginal tube helps in identifying the vaginal cuff edges and facilitating its closure without loss of pneumoperitoneum.
Laparoscopic instrument trolley (Video 14: Instrument trolley)
Video 14 Instrument trolley
The laparoscopic instrument trolley should contain:
- Laparoscope: Given a choice, the senior author prefers the 10 mm 30° telescope, because it has a ‘look down’ capacity that allows a view of the lower pelvis and the sides of a large uterus even if multiple fibroids are present, or when the bowel comes down and tends to obstruct the surgical field. It is also possible to use a 5 mm 30° telescope, but the surgeon may not be satisfied with the light transmission (Figure 10). The larger the telescope diameter, the greater the brightness. The senior author recommends a 10 mm laparoscope for operative surgery and a 5 mm telescope for diagnostic work. Some modern 5 mm telescopes have a better degree of illumination, but this is not always the case and certainly not so with an older instrument.
- Trocars (10 mm – one only; two 5 mm trocars – rarely a third 5 mm trocar is required)
- Tooth grasper forceps (2 ´ 4) with flat jaws and no gap between them (1)
- Curved scissors (1)
- Needle holder (1)
- Bipolar forceps
- Polyglactin suture number 1 on half circle round body curved needle (Universal code 2347) 25–30 cm in length
- Myoma screw (normally used towards the end of the surgery to stabilize the uterus at the time of colpotomy incision after removal of the uterine manipulator)
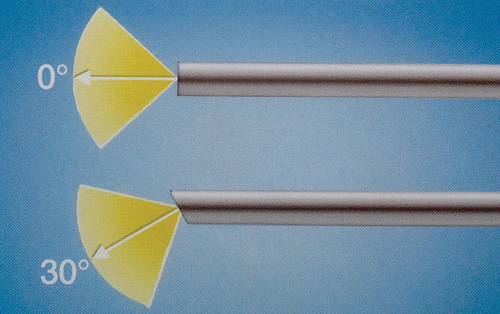
Figure 10 Light transmission with 30° laparoscope
A curved scissors with short blades is preferred because the sharpness of the blade remains intact for a longer time. The need to change the laparoscopic scissors is variable and depends upon the quality of the scissors and the frequency with which it is used. In general, it should be changed once every 3–6 months or after 50–100 hysterectomies, as scissors tend to get blunt.
The tooth grasper forceps (2 ´ 4) with flat jaws without any gap is specifically used as an assistant grasper in laparoscopic suturing of the vaginal vault. The handle of the tooth forceps should be without ratchet; rather, it should have free flowing movement.
The design of the needle holder should be such that the handle should be in line with the long axis of the barrel of the needle driver. Simply stated, the handle should not be pistol shaped. The needle holder should have a minimum number of ratchets. A high number of ratchets results in uncontrolled movements at the tip of the needle driver, making the suturing process difficult owing to needle movement as the ratchets are loosened or tightened. The needle driver should have only two or three ratchets. The first ratchet holds the needle but allows manipulation to get the needle in an upright position. The second ratchet locks the needle in place; the release mechanism should be simple so that one click easily releases the needle. The senior author prefers to use the needle holder in the dominant right hand and the tooth grasper (2 ´ 4) in the non-dominant hand. This simulates laparotomy suturing techniques.
The bipolar forceps is a standard electrosurgical instrument long used in laparoscopic surgery. It was invented by Kleppinger in the mid-1970s after a concept proposed by Rioux1. Numerous modifications to the original design have come to market since the initial prototype appeared. However, the concept remains exactly the same 40 years later. Bipolar cautery is much safer than monopolar cautery and its use results in far fewer bowel and organ injuries from sparking and thermal spread within the tissue. Its use in laparoscopic hysterectomy is standard, because it ensures a level of safety. The senior author prefers to use the bipolar grasper to grasp the tissue securely while coagulating. The grasper can be used as a dissector and an atraumatic grasper to manipulate the bowel and other delicate tissues. Of great importance, it can be utilized consistently throughout the surgery from start to finish without the need to waste time changing to and from other energy sources. In contrast, devices which use ultrasound technologies may be excellent at some steps of surgery, but require backup of bipolar energy sources and cannot be used consistently and effectively throughout the procedure.
Number 1 polyglactin delayed absorbable suture is used on a half-circle curved needle to effect vaginal closure. As in laparotomy, curved needles have universal application and maximum efficiency. The length of the suture should be approximately 25–30 cm. A suture longer than 30 cm is cumbersome to handle efficiently in laparoscopy.
Endovision cart
Progress in laparoscopic surgical skills depends on clear intraoperative vision and good instruments. It is important to have a good quality camera and optics in order to obtain crystal clear vision. The senior author prefers a high resolution camera (>1000 lines), along with a high resolution monitor, both of which allow tissue differentiation and clear visualization while performing the surgery. Without such a camera, it is more cumbersome to differentiate tissue planes when dissecting. Examples of problem areas include endometrioitic adhesions between the rectum and the posterior uterine surface, bladder adhesions anteriorly to the underlying lower uterus and cervix after cesarean section, or dissection of the bladder in a postmenopausal patient.
It is advisable to use a light source which provides bright light. Lower light intensity creates a pixelated or grainy image on the monitor making the surgical steps tedious. Two light sources are currently in wide use: Xenon and LED.
A good bipolar generator (preferably with an auto stop facility) is a vital part of the laparoscopic armamentarium Most modern bipolar generators are adequate to accomplish safe laparoscopic hysterectomy. As with any other energy source, the use of bipolar technology is associated with thermal spread of 7–10 mm from the point of coagulation. The amount of thermal spread and resulting damage to tissue depends upon the duration of the coagulation process. Stated another way, a series of small coagulation bursts reduces the possibility of tissue injury compared to the long sustained thermal coagulation. For this reason modern coagulation units have built-in 30 second autostops or stop immediately when coagulation has been sensed by the machine. A thorough knowledge of the bipolar principle is necessary for all surgeons, because the market is filled with so called ‘high end efficiency’ bipolar electrosurgical generators. It is not the machine that makes the surgery more efficient; it is the technique and planning of the surgeon.
The senior author uses a technique to keep the vital structures away from the point of coagulation in order to avoid thermal damage. It is his belief that the technique of dissection of the bladder and the skeletonization of the uterine vessels is more important than the type of electrosurgical generator used. The reader must always be aware that thermal spread is an inherent part of the coagulation process irrespective of the type of generator and technology that is selected.
One should use a CO2 insufflator which provides a continuous high flow at a set flow rate with a cut off mechanism when a set pressure is reached. It is advisable to use an insufflator which provides warm CO2 to prevent hypothermia. Care should be taken to use a filter while insufflating. The insufflator should prominently show the flow rate and the pressure settings on its display monitor (Figure 11). The abdominal pressure is maintained at 12–14 mmHg during surgery and it is pre-set. High flow rate and pressure settings are used only for a brief period of time during insertion of the Veress needle. A continuous intra-abdominal pressure more than 16 mmHg may reduce the venous return to the heart and cause cardiovascular compromise.

Figure 11 Insufflator showing readings
The extent of image recording is variable. One should be particular to obtain the patient’s consent if a recording is made. Various commercial video recording devices and computer programs are available. Modern endovision cameras have the facility to generate video images in the form of composite SVHS, DV and DVI formats. Most commercial video recorders use these output formats to create videos. Of these, the DVI recorders are uncommon and, currently, are extremely expensive. For educational purposes, it is sufficient to utilize either S-Video or DV outputs. Modern high definition cameras come with the facility of inbuilt recording directly to the USB drive which is under the surgeon’s control. The authors jointly believe that while it is appropriate to provide the patient with a small number of photographs that illustrate the anatomy and pathology, it is not advisable to provide a full recording of the entire surgical procedure for reasons noted previously.
1 Rioux JE, Cloutier D. A new bipolar instrument for laparoscopic tubal sterilization. Am J Obstet Gynecol 1974;119:737–9
